The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

Account Management
Log in to manage your policy, generate a certificate of insurance (COI), make a payment, and more.
Log in to your account to update your information or manage your policy.
Download a Certificate of Insurance (COI) to provide to your employer.
Make a Payment
Make a one-time payment, set up autopay, or update your payment information.
Submit a notice of an incident or claim in just minutes.
Topics on this page:
Why Critical Thinking in Nursing Is Important
8 examples of critical thinking in nursing, improving the quality of patient care, the importance of critical thinking in nursing.
Jul 24, 2024
While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you’re not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what’s the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child’s behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient’s surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There’s lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jul 24, 2024. Originally published on Aug 25, 2021.
- Career Growth
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
The product descriptions provided here are only brief summaries and may be changed without notice. The full coverage terms and details, including limitations and exclusions, are contained in the insurance policy. If you have questions about coverage available under our plans, please review the policy or contact us at 833-242-3794 or [email protected] . “20% savings” is based on industry pricing averages.
Berxi™ is a part of Berkshire Hathaway Specialty Insurance ( BHSI ). Insurance products are distributed through Berkshire Hathaway Global Insurance Services, California License # 0K09397. BHSI is part of Berkshire Hathaway’s National Indemnity group of insurance companies, consisting of National Indemnity and its affiliates, which hold financial strength ratings of A++ from AM Best and AA+ from Standard & Poor’s. The rating scales can be found at www.ambest.com and www.standardandpoors.com , respectively.
No warranty, guarantee, or representation, either expressed or implied, is made as to the correctness, accuracy, completeness, adequacy, or sufficiency of any representation or information. Any opinions expressed herein are subject to change without notice.
The information on this web site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment, and does not purport to establish a standard of care under any circumstances. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only based upon the information available at the time of presentation, and does not constitute medical, legal, regulatory, compliance, financial, professional, or any other advice.
BHSI makes no representation and assumes no responsibility or liability for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to consider and confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician or medical care provider. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING THAT YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
BHSI is not a medical organization, and does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information contained on or available through this web site. BHSI IS NOT RESPONSIBLE FOR, AND EXPRESSLY DISCLAIMS ALL LIABILITY FOR, ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER SERVICES OR PRODUCTS THAT YOU OBTAIN AFTER REVIEWING THIS WEB SITE.
Want Berxi articles delivered straight to your inbox? Sign up for our monthly newsletter below!
" * " indicates required fields
How we use your email address Berxi will not sell or rent your email address to third parties unless otherwise notified. Other than where necessary to administer your insurance policy or where required by law, Berxi will not disclose your email address to third parties. Your email address is required to identify you for access to the Berxi website. You may also receive newsletters, product updates, and communications about quotes and policies.
Paul Dughi is a contributing writer for Berxi, as well as a journalist and freelance writer. He has held executive management positions in the media industry for the past 25 years.
Related Articles

Breaking Bad News to Patients: A Nurse’s Guide to SPIKES
Michael Walton Jul 24, 2024

Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
Kristy Snyder Jul 24, 2024

The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Paul Dughi Aug 28, 2024
- Pre-Nursing
- Nursing School
- After Graduation
How to Apply Critical Thinking in Nursing

- Over 125 Years of Healthcare Expertise: 125+ years of combined healthcare experience with a focus in nursing education.
- Exceptional User Satisfaction: 4.9/5 average rating from 3,500+ reviews across TrustPilot , WorthePenny , Better Business Bureau, and other trusted review sites.
- Proven Success: Over 1 million nurses served since 2012 with a 99% NCLEX pass rate ( 2024 NCLEX average pass rate = 79%).
- Team Composition: Staff includes RNs, MSNs, DHSs, nursing professors, and current/former NCLEX question writers.
Jump to Sections
Harnessing the power of critical thinking can be the key to becoming a successful and competent nurse.
Developing and refining your critical thinking skills is crucial as you embark on your nursing journey. By doing so, you’ll enhance your ability to provide high-quality care, advance your professional growth, and contribute to the ever-evolving nursing field.
What is critical thinking in nursing?
Critical thinking is an essential cognitive process that enables nurses to analyze, evaluate, and synthesize information to make informed decisions. In the context of nursing, it involves observing, interpreting, and responding to patient needs effectively.
Critical thinking allows nurses to go beyond memorized facts and apply logical reasoning to address patient problems holistically.
As a nurse, you’ll encounter multifaceted healthcare scenarios, each presenting its unique challenges. Critical thinking enables you to approach these situations systematically, evaluate the available data, identify relevant factors, and understand the patient’s condition comprehensively.
By employing critical thinking skills, you can differentiate between urgent and non-urgent issues, prioritize care, anticipate potential complications, and adapt your interventions accordingly. This analytical approach helps minimize errors, promote patient safety, and achieve positive patient outcomes.
Why is critical thinking important in nursing?
Critical thinking serves as the backbone of nursing practice. You’ll encounter various uncertainties, changing conditions, and ethical dilemmas as a nurse. Developing critical thinking abilities empowers you to navigate these challenges confidently and provide optimal patient care.
In nursing, critical thinking is crucial for the following reasons:
- Enhanced Clinical Judgment: Critical thinking enables assessing complex situations, analyzing available information, and drawing logical conclusions. It enhances your clinical judgment, allowing you to make informed decisions based on the best available evidence and expert consensus.
- Effective Problem Solving: Nursing involves encountering problems and finding effective solutions. Critical thinking equips you with the tools to identify underlying issues, explore alternative options, and implement interventions that address the root cause of the problem.
- Patient Advocacy: Critical thinking empowers you to advocate for your patients’ needs. By actively engaging in critical inquiry, you can challenge assumptions, question policies, and promote patient-centered care.
- Adapting to Changing Environments: Healthcare is constantly evolving, with new research findings, technologies, and treatments emerging regularly. Developing critical thinking skills helps you adapt to these changes, ensuring you stay updated and deliver evidence-based care.
Examples of Critical Thinking in Nursing
Let’s dive into some real-life examples that highlight how critical thinking plays a crucial role in nursing practice:
- Prioritization: Imagine working in an emergency department where multiple patients arrive simultaneously with varying degrees of severity. Utilizing critical thinking, you can assess each patient’s condition, prioritize care based on the urgency of their needs, and allocate resources effectively.
- Medication Administration: When administering medication, critical thinking prompts you to cross-check the prescribed dose, assess potential drug interactions or allergies, and evaluate the patient’s response to the medication. This proactive approach ensures patient safety and minimizes medication errors.
- Ethical Dilemmas: Critical thinking helps you navigate complex ethical dilemmas by analyzing the values at stake, considering legal and ethical principles, and collaborating with the healthcare team to make decisions that align with the patient’s best interests.
Supplement Your Nursing Studies and Boost Your Grades
At SimpleNursing , we understand the significance of critical thinking in nursing education. Our comprehensive digital study tools are designed to enhance your critical thinking abilities, providing you with interactive case studies, practice questions, and simulated patient scenarios.
Boost your confidence and excel in your nursing studies with SimpleNursing’s innovative study resources.
Sign up for a free trial and take your nursing study skills to new heights.
Get FREE Stuff
Let us email you free weekly content to help you pass nursing school and the NCLEX
- Nursing school study guides
- Exclusive video access
- Exam practice questions
- Subscriber-only discounts
Share this post
Nursing students trust simplenursing.

SimpleNursing Student Testimonial
Most recent posts.

Nursing Diagnosis: A Complete Guide for Students & Professionals
What is one of the most essential tools in a nurse's toolkit? If you answered…

Top 10 Least Stressful Nursing Jobs
When you decided to become a nurse, you knew it would involve long hours and…

Nursing Interventions: Implementing Effective Client Care Plans
If you’re struggling to wrap your head around the term “nursing interventions,” don’t worry —…

How to Write a Nursing Care Plan – A Simple Guide for Nurses
In nursing, one size rarely fits all, especially when it comes to providing top-notch client…
Find what you are interested in
Education: SimpleNursing Editorial Team Education

Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1293 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Thinking Critically About the Quality of Critical Thinking Definitions and Measures

Criticality in Osteopathic Medicine: Exploring the Relationship between Critical Thinking and Clinical Reasoning

A guide to critical thinking: implications for dental education
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Margaret McCartney:...
Nurses are critical thinkers
Rapid response to:
Margaret McCartney: Nurses must be allowed to exercise professional judgment
- Related content
- Article metrics
- Rapid responses
Rapid Response:
The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice. Nurses’ ability to recognize and respond to signs of patient deterioration in a timely manner plays a pivotal role in patient outcomes (Purling & King 2012). Errors in clinical judgement and decision making are said to account for more than half of adverse clinical events (Tomlinson, 2015). The focus of the nurse clinical judgement has to be on quality evidence based care delivery, therefore, observational and reasoning skills will result in sound, reliable, clinical judgements. Clinical judgement, a concept which is critical to the nursing can be complex, because the nurse is required to use observation skills, identify relevant information, to identify the relationships among given elements through reasoning and judgement. Clinical reasoning is the process by which nurses observe patients status, process the information, come to an understanding of the patient problem, plan and implement interventions, evaluate outcomes, with reflection and learning from the process (Levett-Jones et al, 2010). At all times, nurses are responsible for their actions and are accountable for nursing judgment and action or inaction.
The speed and ability by which the nurses make sound clinical judgement is affected by their experience. Novice nurses may find this process difficult, whereas the experienced nurse should rely on her intuition, followed by fast action. Therefore education must begin at the undergraduate level to develop students’ critical thinking and clinical reasoning skills. Clinical reasoning is a learnt skill requiring determination and active engagement in deliberate practice design to improve performance. In order to acquire such skills, students need to develop critical thinking ability, as well as an understanding of how judgements and decisions are reached in complex healthcare environments.
As lifelong learners, nurses are constantly accumulating more knowledge, expertise, and experience, and it’s a rare nurse indeed who chooses to not apply his or her mind towards the goal of constant learning and professional growth. Institute of Medicine (IOM) report on the Future of Nursing, stated, that nurses must continue their education and engage in lifelong learning to gain the needed competencies for practice. American Nurses Association (ANA), Scope and Standards of Practice requires a nurse to remain involved in continuous learning and strengthening individual practice (p.26)
Alfaro-LeFevre, R. (2009). Critical thinking and clinical judgement: A practical approach to outcome-focused thinking. (4th ed.). St Louis: Elsevier
The future of nursing: Leading change, advancing health, (2010). https://campaignforaction.org/resource/future-nursing-iom-report
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J., & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: an educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today. 30(6), 515-520.
NMC (2010) New Standards for Pre-Registration Nursing. London: Nursing and Midwifery Council.
Purling A. & King L. (2012). A literature review: graduate nurses’ preparedness for recognising and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23–24), 3451–3465
Thompson, C., Aitken, l., Doran, D., Dowing, D. (2013). An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies, 50 (12), 1720 - 1726 Tomlinson, J. (2015). Using clinical supervision to improve the quality and safety of patient care: a response to Berwick and Francis. BMC Medical Education, 15(103)
Competing interests: No competing interests

15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)

Last updated on August 19th, 2023
Critical thinking is a powerful tool that nurses use to make informed decisions, provide top-notch care, and untangle complex problems.
Think of it as a toolbox filled with skills that let nurses dig deeper, understand better, and think smarter.
In this article, we’re going to explore the 15 super-important attitudes of critical thinking in nursing .
Each attitude is like a special key that helps nurses unlock the best care for their patients. Let’s dive in and learn about each attitude.
How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
15 Attitudes of Critical Thinking in Nursing
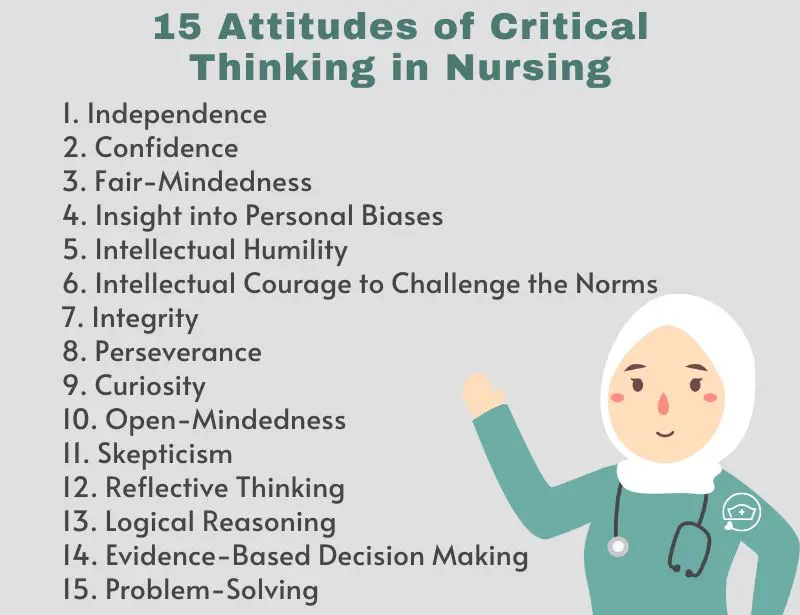
1. Independence
Independence is like thinking for yourself and making your own choices. Imagine you’re deciding what book to read, and you pick one that interests you, not just what others like – that’s being independent.
In nursing, independence means using your own judgment to provide the best care.
For, example, consider Rachel, a nurse, who considers various options to treat a patient’s pain, not just following what others do. Rachel’s independence helps her find solutions tailored to each patient’s needs.
Just like choosing your own book, independent nurses think critically and make decisions based on what’s best for their patients.
2. Confidence
Confidence is like believing in yourself and your abilities, even when faced with challenges. Imagine you’re trying a new activity, and you trust that you can learn and do well – that’s having confidence.
In nursing, confidence means having faith in your skills and judgment to provide excellent care. Example: For instance, think of Ava, a nurse, who remains composed when a patient’s condition suddenly worsens.
She knows she can handle the situation because of her training and experience. Ava’s confidence allows her to make quick and effective decisions during critical moments.
Just like trusting yourself in a new activity, confident nurses trust their expertise to deliver top-notch care to their patients.
3. Fair-Mindedness
Fair-mindedness is like treating everyone equally and making judgments based on facts, not personal feelings. Imagine you’re playing a game, and you give every player the same chance to win – that’s being fair-minded.
In nursing, fair-mindedness means being impartial and considering all viewpoints without bias.
For example, picture Liam, a nurse, who listens to both the patient and the family when making a decision about treatment.
He doesn’t let his own opinions influence his judgment. Liam’s fair-mindedness ensures that he provides balanced and patient-focused care.
Just like being fair in a game, fair-minded nurses make decisions that are just and unbiased, promoting the best outcomes for their patients.
4. Insight into Personal Biases
Insight into personal biases is like looking at yourself from the outside to see if your own feelings might affect your decisions. Imagine you have a favorite color, and you realize you tend to choose things in that color even if other options might be better – that’s being aware of your bias.
In nursing, insight into personal biases means being mindful of your own preferences and not letting them cloud your judgment.
For instance, think of Maya, a nurse, who knows she might prefer a particular treatment because it worked for her family member.
However, she steps back and considers what’s truly best for her patient’s situation. Maya’s insight helps her provide care that’s unbiased and patient-centered.
Just like being aware of your color preference, insight into personal biases helps nurses make decisions that are based on what’s right for their patients, not influenced by their own feelings.
5. Intellectual Humility
Intellectual humility is like knowing that you don’t have all the answers and being open to learning from others. Imagine you’re playing a video game, and you ask a friend for tips because they’re better at it – that’s being humble about your skills.
In nursing, intellectual humility means recognizing that you can always learn more and considering others’ expertise.
Picture James, a nurse, who seeks advice from experienced colleagues when faced with a complex case.
He knows that learning from others can lead to better patient care. James’s intellectual humility helps him grow as a nurse and keeps him open to new perspectives.
Just like seeking gaming tips, intellectual humility encourages nurses to value knowledge from various sources and continuously improve their practice.
6. Intellectual Courage to Challenge the Norms
Intellectual courage to challenge the norms is like having the bravery to question things that everyone believes are true. Imagine you’re playing a game with your friends, and everyone agrees on the rules – but you speak up and suggest a new way to play.
In nursing, intellectual courage means daring to question established practices and seeking innovative solutions.
For instance, think of Sarah, a nurse, who notices that a routine procedure might be improved for patient comfort.
Instead of staying silent, she speaks up and proposes a change, backed by research and careful thought. Sarah’s intellectual courage drives her to challenge the status quo for the sake of better patient care.
Just like suggesting a new game rule, nurses with this attitude challenge norms to advance healthcare practices and outcomes.
7. Integrity
Integrity is like being honest and doing the right thing, even when nobody’s watching. Imagine finding a lost wallet on the street – instead of keeping it, you return it to its owner because it’s the right thing to do.
In nursing, integrity means always acting ethically and responsibly, even in challenging situations.
Picture Emma, a nurse, who follows protocols and makes decisions based on what’s best for her patients, not personal gain.
Emma’s integrity shines when she prioritizes honesty, fairness, and patient well-being in every action she takes.
Just like returning that wallet, integrity is a nurse’s commitment to uphold high moral standards and maintain the trust placed in them by patients and their families.
8. Perseverance
Perseverance is like having a never-give-up attitude, even when things get tough. Imagine you’re trying to solve a challenging puzzle – even if it takes time and effort, you keep going until you find the solution.
In nursing, perseverance means facing obstacles and difficulties head-on without giving up.
For example, consider Mark, a nurse, who’s dealing with a complex patient case. Despite encountering roadblocks and uncertainties, Mark doesn’t lose hope.
He keeps researching, consulting colleagues, and trying different approaches until he finds the right solution for his patient.
Just like working through a tough puzzle, perseverance empowers nurses to keep pushing forward and find the answers that lead to the best care outcomes.
9. Curiosity
Curiosity is like having a hunger for knowledge that never goes away. Imagine you’re exploring a new place, and every corner seems to hide something interesting – you want to know what’s around the next bend.
In nursing, curiosity means having a strong desire to learn and discover.
Picture Anna, a nurse, who’s always asking questions like “Why?” and “How?” She’s not content with just knowing the basics; she wants to dive deeper and understand the “whys” behind patient conditions and treatments.
Anna’s curiosity drives her to stay updated with the latest research and innovative methods. Just like an explorer seeking new horizons, curious nurses seek new ways to provide better care for their patients.
10. Open-Mindedness
Open-mindedness is like having a door in your mind that’s always ready to welcome new ideas. Imagine you’re reading a book, and suddenly you come across a different way of thinking – instead of dismissing it, you consider it with interest.
In nursing, open-mindedness means being willing to listen to various viewpoints and explore different approaches.
For instance, think of Rachel, a nurse, who’s used to a specific way of treating wounds. But when a colleague suggests a new method, Rachel doesn’t shut the idea down.
Instead, she’s open to trying it out and seeing if it might work better for her patients. Just like being curious about new stories, open-minded nurses are curious about new ways to improve patient care.
11. Skepticism
Skepticism is like being a curious investigator who asks questions to make sure things are true. Imagine you hear about a magical potion that promises to make you fly – you might be skeptical and ask, “Is that really possible?”
In nursing, skepticism means not accepting things blindly but investigating to find the truth.
Picture Sarah, a nurse, who reads about a new treatment for pain relief. Instead of immediately believing it, she looks for evidence and checks if other experts agree.
Sarah’s skepticism helps her make sure that the treatments she uses are safe and effective for her patients.
Just like asking questions about that magical potion, nurses use skepticism to make informed decisions based on facts.
12. Reflective Thinking
Reflective thinking is like looking back at your day and thinking about what went well and what you could improve. Imagine you finished playing a game and you think about how you did – that’s reflective thinking!
In nursing, it’s when nurses take a moment to think about their actions, decisions, and interactions with patients.
For example, let’s say Jessica, a nurse, had a challenging day where she had to juggle multiple tasks. At the end of her shift, she takes a few minutes to reflect.
She thinks about what she did right, like comforting a worried patient, and what she could do better, like managing her time more efficiently.
This reflection helps Jessica learn from her experiences and become an even better nurse.
Just like looking in a mirror to see yourself, reflective thinking helps nurses see their actions and grow from them.
13. Logical Reasoning
Logical reasoning is like putting together the pieces of a puzzle to see the bigger picture. It’s about thinking step by step to reach a smart conclusion.
Imagine you have a math problem to solve. You start with the information you know and use logical steps to find the answer.
Similarly, nurses use logical reasoning to understand their patients’ situations
Let’s say Emily, a nurse, has a patient with a high fever and a sore throat. She gathers information about the symptoms, asks questions, and puts all the clues together.
By using logical steps, Emily figures out that the patient might have a throat infection and can recommend the right treatment.
Just like solving a puzzle, logical reasoning helps nurses connect the dots and make decisions that make sense for their patient’s health.
14. Evidence-Based Decision Making
Evidence-based decision-making is like being a detective who gathers clues before solving a mystery.
For instance, imagine Alex, a nurse, who wants to find the best way to help patients with diabetes manage their blood sugar levels.
Instead of guessing, he reads research studies and talks to experts in the field. Alex uses the facts he collects to choose treatments that are proven to work.
Just like a detective uses evidence to solve a case, Alex uses evidence to make informed decisions that lead to better patient outcomes.
15. Problem-Solving
Problem-solving is like being a detective on a mission. Think of it like when you have to figure out how to fix a broken toy.
For instance, Linda, a nurse, faces a challenge when a patient’s pain medication isn’t working well. Instead of giving up, she gathers information, talks to the patient, and works with the medical team to find a better solution.
Linda’s problem-solving skills help her piece together the right treatment plan, just like solving a tricky puzzle.
- What is Critical Thinking in Nursing? (Explained W/ Examples)
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
Critical thinking is a powerful tool that nurses use every day. These 15 attitudes are like a treasure map that guides nurses through the world of healthcare.
From being independent thinkers to having the courage to challenge norms, these attitudes help nurses provide the best care possible.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.
We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them)
By Hannah Meinke on 07/05/2021
The nursing profession tends to attract those who have natural nurturing abilities, a desire to help others, and a knack for science or anatomy. But there is another important skill that successful nurses share, and it's often overlooked: the ability to think critically.
Identifying a problem, determining the best solution and choosing the most effective method to solve the program are all parts of the critical thinking process. After executing the plan, critical thinkers reflect on the situation to figure out if it was effective and if it could have been done better. As you can see, critical thinking is a transferable skill that can be leveraged in several facets of your life.
But why is it so important for nurses to use? We spoke with several experts to learn why critical thinking skills in nursing are so crucial to the field, the patients and the success of a nurse. Keep reading to learn why and to see how you can improve this skill.
Why are critical thinking skills in nursing important?
You learn all sorts of practical skills in nursing school, like flawlessly dressing a wound, taking vitals like a pro or starting an IV without flinching. But without the ability to think clearly and make rational decisions, those skills alone won’t get you very far—you need to think critically as well.
“Nurses are faced with decision-making situations in patient care, and each decision they make impacts patient outcomes. Nursing critical thinking skills drive the decision-making process and impact the quality of care provided,” says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing.
For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they must evaluate which patients should be treated first. While they rely on their training to measure vital signs and level of consciousness, they must use critical thinking to analyze the consequences of delaying treatment in each case.
No matter which department they work in, nurses use critical thinking in their everyday routines. When you’re faced with decisions that could ultimately mean life or death, the ability to analyze a situation and come to a solution separates the good nurses from the great ones.
How are critical thinking skills acquired in nursing school?
Nursing school offers a multitude of material to master and upholds high expectations for your performance. But in order to learn in a way that will actually equip you to become an excellent nurse, you have to go beyond just memorizing terms. You need to apply an analytical mindset to understanding course material.
One way for students to begin implementing critical thinking is by applying the nursing process to their line of thought, according to Vest. The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation.
“One of the fundamental principles for developing critical thinking is the nursing process,” Vest says. “It needs to be a lived experience in the learning environment.”
Nursing students often find that there are multiple correct solutions to a problem. The key to nursing is to select the “the most correct” solution—one that will be the most efficient and best fit for that particular situation. Using the nursing process, students can narrow down their options to select the best one.
When answering questions in class or on exams, challenge yourself to go beyond simply selecting an answer. Start to think about why that answer is correct and what the possible consequences might be. Simply memorizing the material won’t translate well into a real-life nursing setting.
How can you develop your critical thinking skills as a nurse?
As you know, learning doesn’t stop with graduation from nursing school. Good nurses continue to soak up knowledge and continually improve throughout their careers. Likewise, they can continue to build their critical thinking skills in the workplace with each shift.
“To improve your critical thinking, pick the brains of the experienced nurses around you to help you get the mindset,” suggests Eileen Sollars, RN ADN, AAS. Understanding how a seasoned nurse came to a conclusion will provide you with insights you may not have considered and help you develop your own approach.
The chain of command can also help nurses develop critical thinking skills in the workplace.
“Another aid in the development of critical thinking I cannot stress enough is the utilization of the chain of command,” Vest says. “In the chain of command, the nurse always reports up to the nurse manager and down to the patient care aide. Peers and fellow healthcare professionals are not in the chain of command. Clear understanding and proper utilization of the chain of command is essential in the workplace.”
How are critical thinking skills applied in nursing?
“Nurses use critical thinking in every single shift,” Sollars says. “Critical thinking in nursing is a paramount skill necessary in the care of your patients. Nowadays there is more emphasis on machines and technical aspects of nursing, but critical thinking plays an important role. You need it to understand and anticipate changes in your patient's condition.”
As a nurse, you will inevitably encounter a situation in which there are multiple solutions or treatments, and you'll be tasked with determining the solution that will provide the best possible outcome for your patient. You must be able to quickly and confidently assess situations and make the best care decision in each unique scenario. It is in situations like these that your critical thinking skills will direct your decision-making.
Do critical thinking skills matter more for nursing leadership and management positions?
While critical thinking skills are essential at every level of nursing, leadership and management positions require a new level of this ability.
When it comes to managing other nurses, working with hospital administration, and dealing with budgets, schedules or policies, critical thinking can make the difference between a smooth-running or struggling department. At the leadership level, nurses need to see the big picture and understand how each part works together.
A nurse manager , for example, might have to deal with being short-staffed. This could require coaching nurses on how to prioritize their workload, organize their tasks and rely on strategies to keep from burning out. A lead nurse with strong critical thinking skills knows how to fully understand the problem and all its implications.
- How will patient care be affected by having fewer staff?
- What kind of strain will be on the nurses?
Their solutions will take into account all their resources and possible roadblocks.
- What work can be delegated to nursing aids?
- Are there any nurses willing to come in on their day off?
- Are nurses from other departments available to provide coverage?
They’ll weigh the pros and cons of each solution and choose those with the greatest potential.
- Will calling in an off-duty nurse contribute to burnout?
- Was this situation a one-off occurrence or something that could require an additional hire in the long term?
Finally, they will look back on the issue and evaluate what worked and what didn’t. With critical thinking skills like this, a lead nurse can affect their entire staff, patient population and department for the better.
Beyond thinking
You’re now well aware of the importance of critical thinking skills in nursing. Even if you already use critical thinking skills every day, you can still work toward strengthening that skill. The more you practice it, the better you will become and the more naturally it will come to you.
If you’re interested in critical thinking because you’d like to move up in your current nursing job, consider how a Bachelor of Science in Nursing (BSN) could help you develop the necessary leadership skills.
EDITOR’S NOTE: This article was originally published in July 2012. It has since been updated to include information relevant to 2021.
- Share on Facebook
- Share on Twitter
- Share on Pinterest
- Share on LinkedIn
Request More Information
Talk with an admissions advisor today.
Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid (for those who qualify)
- Customized Support Services
- Detailed Program Plans
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- 10 digits with no dashes or spaces
- No country code (e.g. "1" for USA)
There is an error in ZIP code. Make sure your answer has only 5 digits.
We offer tuition savings for many employers—see if yours is one of them.
Please enter Corporate Employer.
Can’t find your employer? Select "Other Employer Not In List" or "Not Employed".
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Hannah Meinke

Posted in General Nursing
- nursing education
Related Content

Brianna Flavin | 05.07.2024

Brianna Flavin | 03.19.2024

Robbie Gould | 11.14.2023

Noelle Hartt | 11.09.2023
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.
- Visit Nurse.com on Facebook
- Visit Nurse.com on YouTube
- Visit Nurse.com on Instagram
- Visit Nurse.com on LinkedIn
Nurse.com by Relias . © Relias LLC 2024. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.8(4); 2021 Jul
Factors associated with the critical thinking ability of professional nurses: A cross‐sectional study
Tuan van nguyen.
1 Faculty of Nursing and Medical Technology, Can Tho University of Medicine and Pharmacy, Can Tho Vietnam
2 School of Nursing, College of Medicine, Chang Gung University, Taoyuan Taiwan

Hsueh‐Erh Liu
3 Department of Rheumatology, Chang Gung Memorial Hospital, Linkou Taiwan
4 Department of Nursing, College of Nursing, Chang Gung University of Science and Technology, Taoyuan, Taiwan
Associated Data
The data that support the findings of this study are available from the corresponding author upon reasonable request.
To measure the level of critical thinking among Vietnamese professional nurses and to identify the related factors.
A cross‐sectional design was used.
The total sample included 420 professional nurses. Data were collected from July to September 2019 in three public hospitals located in Southwestern Vietnam. The level of critical thinking was measured using the Vietnamese version of the Nursing Critical Thinking in Clinical Practice Questionnaire. The data were analysed using the independent Student's t tests, ANOVA, Pearson's correlation and regression analysis.
Most of the participants had a low (48.3%) or moderate (45.5%) level of critical thinking. Age, gender, ethnicity, education level, health condition, duration of working as a nurse, duration of working in the current hospital, having heard the term “critical thinking” and work position had an impact on the critical thinking ability. Work position and gender explained 11% of the total variance in critical thinking ability.
1. INTRODUCTION
Critical thinking is defined as the cognitive process of reasoning that involves trying to minimize errors and to maximize positive outcomes while attempting to make a decision during patient care (Zuriguel‐Pérez et al., 2015 ). The importance of critical thinking in nursing practice has been identified in the literature (Chang et al., 2011 ; Ludin, 2018 ; Mahmoud & Mohamed, 2017 ; Yurdanur, 2016 ; Zuriguel‐Pérez et al., 2015 ). The current nursing environment has become more complex and demanding, especially regarding the acuity and safety of patients and the rapid turnover rate of hospitalization. If professional nurses want to provide high‐quality care, critical thinking is required (Berkow et al., 2011 ; Brunt, 2005 ; Fero et al., 2009 ; Zuriguel‐Pérez et al., 2015 ). Nurses are often the first‐line professionals to observe and provide direct care for patients. Therefore, critical thinking is a necessary skill for them to be able to analyse clinical situations in order to make fast and correct decisions (Lee et al., 2017 ). More importantly, critical thinking can also improve patient outcomes by preventing habitual thinking that may lead to incorrect medication or procedures (Fesler‐Birch, 2005 ). The critical thinking ability of nurses can have an impact on the patient's safety, and it is a priority in educational programs for healthcare providers (Berkow et al., 2011 ; Buerhaus et al., 2006 ). We can identify those with poor critical thinking and provide in‐service education. Although critical thinking has been shown that is influenced by the experience and knowledge acquired during clinical practice (Zuriguel‐Pérez et al., 2015 ), other personal information needs to be considered to clarifying. Therefore, it is essential to measure the levels of critical thinking and to identify the work‐related and personal‐related factors that influence the critical thinking of nurses.
2. BACKGROUND
The literature has identified that there is a relationship between leadership and positive patient outcomes, such as fewer medication errors and nosocomial infections, lower patient mortality and higher patient satisfaction (Van Dyk et al., 2016 ; Wong, 2015 ). Alongside leadership, critical thinking is an important factor that supports the management. They can apply critical thinking skills in decision‐making and problem‐solving, and they can develop strategies that help staff nurses to improve their critical thinking ability (Van Dyk et al., 2016 ; Wong, 2015 ; Zuriguel‐Pérez et al., 2018 ). Thus, the ability to think critically is necessary for nurses because it will help them to effectively make decisions and to solve problems in practice.
Although the importance of critical thinking in nursing practice has been identified, a limited number of studies have been conducted in this population. Particularly, few hospitals have evaluated the critical thinking skills of nurses before employment or during the clinical competency evaluation (Lang et al., 2013 ). By reviewing 90 articles to assess the current state of the scientific knowledge regarding critical thinking in nursing, Zuriguel‐Pérez et al., ( 2015 ) found that only 16 studies used working nurses as participants. Furthermore, Zuriguel‐Pérez et al., ( 2018 ) reported that few studies have explored the critical thinking ability of nurse managers (NMs). Moreover, several studies have identified that working nurses have a low (Lang et al., 2013 ; Yurdanur, 2016 ) or moderate level of critical thinking (Chang et al., 2011 ; Lang et al., 2013 ; Zuriguel‐Pérez et al., 2018 ). To the researchers’ knowledge, no studies have investigated this issue in Vietnam.
In order to improve the quality and safety of patient care, various types of professional nurses have been established, such as Registered Nurses (RNs), NMs and administrative assistants (AAs). RNs provide direct care to the patients, NMs are responsible for forwarding management and delivering expert clinical care for patients, and AAs are an integral part of maintaining the quality of patient care. The AAs perform administrative tasks (e.g. filing, taking meeting minutes and distributing them and undertaking regular reports) that help NMs to spend more time assisting staff nurses and taking care of patients (Locke et al., 2011 ). Therefore, RNs, NMs and AAs need to cooperate to help patients to regain their health.
In Vietnam, professional nurses work in three different positions, which are NMs, general nurses (GNs) and AAs (Ministry of Health, 1997 ). Specifically, NMs are recognized as head nurses in Western countries, and their responsibilities are in charge of organizing and implementing comprehensive patient care and conduct a variety of administrative work (e.g. planning and assigning work to nurses, planning the acquisition of tools and consumables, checking care sheets, recording daily labour). GNs are similar to RNs in Western countries, and they provide direct and comprehensive care to patients. AAs perform administrative tasks (e.g. keeping records about the hospitalized and discharged patients, preserving medical records, managing daily medications). They also participate in patients care if necessary (Ministry of Health, 1997 , 2011 ). Although the roles of these three types of professional nurses are different, their final goal is the same to provide holistic care for patients. With the cooperation and effort of these three types of professional nurses, patients can recover. Therefore, more surveys are needed that examine these participants’ level of critical thinking and the associated work‐related factors.
Previous studies have also found that several personal‐related factors are associated with the nurses' critical thinking ability, which are age, gender, ethnicity, education qualification, working experience and shift work (Chang et al., 2011 ; Feng et al., 2010 ; Howenstein et al., 1996 ; Lang et al., 2013 ; Ludin, 2018 ; Mahmoud & Mohamed, 2017 ; Ryan & Tatum, 2012 ; Wangensteen et al., 2010 ; Yildirim et al., 2012 ; Yurdanur, 2016 ; Zuriguel‐Pérez et al., 2018 ). However, the relationships between the critical thinking ability and these variables are inconsistent. For example, age and critical thinking have been found to be positively correlated (Chang et al., 2011 ; Ludin, 2018 ; Zuriguel‐Pérez et al., 2018 ), negatively correlated (Howenstein et al., 1996 ) and not related (Lang et al., 2013 ; Mahmoud & Mohamed, 2017 ; Yurdanur, 2016 ). Gender and critical thinking have been reported with a statistically significant relationship (Liu et al., 2019 ; Ludin, 2018 ) and no relationship (Mahmoud & Mohamed, 2017 ; Wangensteen et al., 2010 ). Level of education and critical thinking have been found in a positive association (Chang et al., 2011 ; Ludin, 2018 ) and not association (Lang et al., 2013 ; Mahmoud & Mohamed, 2017 ). Year of experiences and critical thinking have been shown to be positively correlated (Chang et al., 2011 ; Ludin, 2018 ), negatively correlated (Howenstein et al., 1996 ) and not related (Lang et al., 2013 ; Mahmoud & Mohamed, 2017 ). Those inconsistent findings indicated the relationships between the personal‐characteristics and the critical thinking ability of professional nurses need further exploration. Therefore, this study aimed to examine the level of critical thinking of professional nurses and to explore the work‐related and personal‐related factors. This is the first study to investigate this issue in Vietnam. The results of the current study will make a significant contribution to the literature because it will provide thorough descriptions of the critical thinking of professional nurses and its associated factors. Furthermore, the findings may be used as a baseline for nurse managers and nurse educators to propose further strategies to improve this ability in professional nurses.
3.1. Research design
A cross‐sectional design was used. The Strengthening the Reporting of Observational Studies in Epidemiology guidelines were applied in this report (Von Elm et al., 2014 ).
3.2. Setting and sampling
Data collection was carried out from July to September 2019 in three representative and major public hospitals located in the Southwestern region of Vietnam. These hospitals have the same organizational structure, role of treating, operation of professional nursing and provide similar quality of health care to people around that area. The total numbers of professional in these three hospitals nurses were around 1,200. Besides, our study has two steps. The first step was to translate the English version of the Nursing Critical Thinking in Clinical Practice Questionnaire (N‐CT‐4 Practice) into the Vietnamese version. In that step, we used data as a pilot study to estimate the sample size in the second step, which was reported here. Sample size calculation was done by the formula: n = 1.96 2 × p × (1‐p)/0.05 2 , where p = .46 came from the poor level of critical thinking among nurses in the first step and 0.05 indicated the acceptable margin of error (5.0%); 382 participants were required by this formula. An additional 10% of participants were done to adjust for potential failures such as withdrawals or missing data (Suresh & Chandrashekara, 2012 ). Therefore, in total, 420 participants were required for this study. Convenience sampling was conducted to recruit the sample. The inclusion criteria were the nurses' employed full‐time employment in the study hospitals. Participants who participated in step 1 or being absent during the data collection such as sick leave or delivering a baby were excluded. Participants were grouped in each hospital and received an envelope with all questionnaires. Then, researchers explained the research's purpose, benefits and risks to the potential participants and the procedure for ensuring confidentiality, and the voluntary nature of the participation. The informed consent form was signed immediately after they agreed to participate in this study. Then, the participants were required to complete the questionnaires in 20 to 30 min and to return them to the data collector.
3.3. Data assessment
3.3.1. sample characteristics.
This instrument collected data about the personal information and occupational variables. The personal information included age, gender, marital status, ethnicity, religion, education level and self‐rated health conditions. The occupational variables were the duration of working as a nurse, the duration of working in the current hospital, the duration of working in the specific position, having heard the term “critical thinking” or not, previous exposure to critical thinking training or education or not, and type of work position.
3.3.2. Vietnamese version of the Nursing Critical Thinking in Clinical Practice Questionnaire ((N‐CT‐4 Practice (V‐v))
The N‐CT‐4 Practice (V‐v) was used to measure the critical thinking ability of the professional nurses. The original instrument (N‐CT‐4 Practice) was established and classified based on the four dimensions of the 4‐circle critical thinking model of Alfaro‐LeFevre (Zuriguel‐Pérez et al., 2017 ). These four dimensions were personal; intellectual and cognitive; interpersonal and self‐management; and technical dimensions. The personal dimension has 39 items to assess the individual pattern of intellectual behaviours; the intellectual and cognitive dimension has 44 items to assesses the knowledge of activity comprehension connected to the nursing process and decision‐making. For the interpersonal and self‐management dimension, it has 20 items to analyse interpersonal abilities that allow for therapeutic communication with patients and health teams and to gain information that is associated with the patient in the clinical environment. The final one, the technical dimension, has 6 items to is concerned with knowledge and expertise in the procedures that are part of the discipline of nursing. This scale has 109 items that are rated using a four‐point Likert response format (1 = never or almost never, 2 = occasionally, 3 = often, and 4 = always or almost always), for example: “I recognize my own emotions.” (item 1); “I have the scientific knowledge required to carry out my professional practice.” (item 40); “I adapt information to the needs and capacities of the patient.” (item 84); “I possess skills in the use of information and communication technologies needed to produce optimal professional results.” (item 105). The total score is obtained from the sum of the 109 items. The scores range from 109–436, and they are categorized into a low level (score <329), moderate level (score between 329–395) and high level (score >395). The overall Cronbach's alpha was 0.96, and the intraclass correlation coefficient (ICC) was 0.77 (Zuriguel‐Pérez et al., 2017).
The N‐CT‐4 Practice (V‐v) was translated, and its psychometric properties were tested with 545 Vietnamese nurses. The results showed that the N‐CT‐4 Practice (V‐v) has acceptable reliability (Cronbach's alpha) and validity (content and construct validity). Particularly, the overall Cronbach's alpha was 0.98, with that of the four dimensions ranging from 0.86–0.97. The ICC was 0.81 over two weeks. The item content validity index was 1.0. Moreover, the goodness‐of‐fit indexes in a confirmatory factor analysis showed acceptable values, which were χ 2 / df = 2.87, root mean square error of approximation (RMSEA) = 0.059, standardized root mean square residual (SRMR) = 0.063, comparative fit index (CFI) = 0.73 and Tucker Lewis index (TLI) = 0.72 (T. V. Nguyen & Liu, 2021 ). Therefore, the N‐CT‐4 Practice (V‐v) can be used to measure the critical thinking ability of Vietnamese professional nurses.
3.4. Ethical considerations
This study conformed with the ethical principles of the Declaration of Helsinki (Helsinki Declaration, 2013 ), and it was granted research ethics committee approval by the ethical review board of the first author's institution.
3.5. Data analysis
The data were analysed using SPSS for Windows version 23.0 (IBM Corp.), and both descriptive and inferential statistics were calculated. The level of significance for all analyses was set at < 0.05. First, descriptive statistics were employed to summarize the collected data. The continuous variables were described using the mean and standard deviation ( SD ), and the frequency and percentage (%) were used for the categorical variables. Next, independent Student's t tests, analysis of variance (with Scheffe's post hoc comparison) and Pearson's correlation analysis were conducted to explore the association between the critical thinking ability and the personal and occupational factors. Then, a multiple regression analysis using the stepwise method was performed to identify the predictors of critical thinking ability (Pallant, 2010 ).
4.1. Characteristics of the participants
A total of 420 participants completed the questionnaires; the characteristics of overall participants and subjects in each group are listed in Table 1 . Three groups of subjects were included, which were NMs (24.8%), GNs (49.8%) and AAs (25.4%), respectively. Regarding the personal variables, almost all participants were Vietnamese (96.7%), no religion (73.1%) and had good health condition (60%). Meanwhile, the comparison among each group showed that age ( F = 9.89, p < .001), gender (χ 2 = 6.48, p < .05), marital status (χ 2 = 6.77, p < .05) and education level (χ 2 = 147.38, p < .001) had reached the statistical significance. Further analysis showed that the age of NMs was significantly older than subjects in both the GN and AA group, AA group had a higher ratio of that in the GN group, and the AA group had a higher ratio of married one than the GN group. For educational levels, subjects in the NM group had a higher ratio of bachelor and master degree, whereas the other two groups had a high ratio of diploma and associate degree.
Characteristics of the participants ( n = 420)
| Variables | Totals | Comparisons among work position | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NM ( = 104) | GN ( = 209) | AA ( = 107) | χ | (1) NM | (2) GN | (3) AA | ‐test | Scheffe's post hoc | |||
| (%) | Mean ± | (%) | Mean ± | ||||||||
| Personal variables | |||||||||||
| Age (years) | 32.54 ± 7.32 | 35.22 ± 7.08 | 31.46 ± 7.0 | 32.05 ± 7.56 | 9.89 | (1) > (2), (3) | |||||
| Gender | |||||||||||
| Male | 105 (25) | 28 (26.9) | 60 (28.7) | 17 (15.9) | 6.48 | ||||||
| Female | 315 (75) | 76 (73.1) | 149 (71.3) | 90 (84.1) | |||||||
| Marital status | |||||||||||
| Single/divorced/widowed | 169 (40.2) | 34 (32.7) | 97 (46.4) | 38 (35.5) | 6.77 | ||||||
| Married | 251 (59.8) | 70 (67.3) | 112 (53.6) | 69 (64.5) | |||||||
| Ethnicity | |||||||||||
| Vietnamese | 406 (96.7) | 101 (97.1) | 205 (98.1) | 100 (93.5) | 4.79 | ||||||
| Other | 14 (3.3) | 3 (2.9) | 4 (1.9) | 7 (6.5) | |||||||
| Religion | |||||||||||
| No | 307 (73.1) | 82 (78.8) | 149 (71.3) | 76 (71) | 2.33 | ||||||
| Yes | 113 (26.9) | 22 (21.2) | 60 (28.7) | 31 (29) | |||||||
| Education level | |||||||||||
| Diploma | 126 (30.0) | 3 (2.9) | 90 (43.1) | 33 (30.8) | 147.38 | ||||||
| Associate | 123 (29.3) | 8 (7.7) | 64 (30.6) | 51 (47.7) | |||||||
| Bachelor's/graduate | 171 (40.7) | 93 (89.4) | 55 (26.3) | 23 (21.5) | |||||||
| Self‐rated health condition | |||||||||||
| Very good | 51 (12.1) | 9 (8.7) | 27 (12.9) | 15 (14) | 6.63 | ||||||
| Good | 252 (60.0) | 71 (68.3) | 126 (60.3) | 55 (51.4) | |||||||
| Fair/bad/very bad | 117 (27.9) | 24 (23.1) | 56 (26.8) | 37 (34.6) | |||||||
| Work‐related factors | |||||||||||
| Duration of working as a nurse (years) | 9.30 ± 7.05 | 12.30 ± 7.12 | 8.08 ± 6.42 | 8.75 ± 7.20 | 13.08 | (1) > (2), (3) | |||||
| Duration of working in the current hospital (years) | 8.81 ± 6.85 | 11.66 ± 7.02 | 7.66 ± 6.33 | 8.29 ± 6.93 | 12.98 | (1) > (2), (3) | |||||
| Duration of working in the specific position (years) | 6.10 ± 5.46 | 5.06 ± 4.94 | 7.41 ± 6.21 | 4.05 ± 3.27 | 14.79 | (2) > (1) > (3) | |||||
| Heard the term "CT" | |||||||||||
| No | 280 (66.7) | 56 (53.8) | 151 (72.2) | 73 (68.2) | 10.74 | ||||||
| Yes | 140 (33.7) | 48 (46.2) | 58 (27.8) | 34 (31.8) | |||||||
| Previous exposure to CT training/education | |||||||||||
| No | 420 (100) | 104 (100) | 209 (100) | 107 (100) | |||||||
Abbreviations: AA, Administrator assistant; CT , Critical thinking; GN, General nurse; NM, Nurses manager ; SD , standard deviation.
Chi‐square and one‐way ANOVA test; significant at * p < .05; ** p < .01; *** p < .001.
Regarding work‐related factors, the characters of all participants and subjects in each group are also listed in Table 1 . The comparison of professional experience, such as duration of working as a nurse, duration of working in the current hospital, duration of working in this specific position and heard the terminology of "critical thinking" showed a significant statistical difference among the three groups ( p < .001). They showed that NMs had a longer duration of working as a nurse (mean = 12.30, SD = 7.12) and duration of working in the current hospital (mean = 11.6, SD = 7.02) than the other two groups; GNs had the longest duration of working in the specific position (mean = 7.41, SD = 6.21). More subjects in the NM group heard the terminology of "critical thinking" than subjects in the other two groups. However, none of the subjects had been exposed to critical thinking training or education. Furthermore, there was a positive correlation among age, the duration of working as a nurse, the duration of working in the current hospital and duration of working in a specific position ( r = .78–.975, p < .01).
4.2. Level of the critical thinking of the professional nurses
The mean of the total scores of the N‐CT‐4 Practice (V‐v) for all participants was 333.86 ± 40.22 (with the average score/item = 3.06 ± 0.37), the median score was 331 (interquartile range [IQR] = 311–359), and it ranged from 204–436, which indicates that they generally had a moderate level of critical thinking. Meanwhile, most of the participants reported a low (48.3%) or moderate (45.5%) level of critical thinking. Only 6.2% of the participants had a high level of critical thinking. Regarding the four dimensions of the N‐CT‐4 Practice (V‐v), the average sum score was 119.52 ± 14.19 (with the average score/item = 3.06 ± 0.36) in the personal dimension, 136.38 ± 17.62 (with the average score/item = 3.10 ± 0.40) in the intellectual and cognitive dimension, 68.71 ± 12.65 (with the average score/item = 3.44 ± 0.63) in the interpersonal and self‐management dimension and 18.09 ± 3.01 (with the average score/item = 3.01 ± 0.50) in the technical dimension.
4.3. Work‐related and personal‐related factors associated with critical thinking ability
There were statistically significant associations between the critical thinking ability and some work‐related factors, such as work position ( F = 23.30, p < .001), duration of working as a nurse ( r = 0.15, p < .01), duration of working in the current hospital ( r = 0.13, p < .05) and having heard the term "critical thinking" ( t = −2.48, p < .05; Table 2 ). The findings indicated that NMs had higher scores than GNs and AAs. Moreover, nurses who had worked for a longer duration as a nurse or worked longer in the current hospital had a higher critical thinking ability. Meanwhile, those who had not heard the term "critical thinking" had lower scores than participants who had heard this term.
Association between the participants’ characteristics and the critical thinking ability ( n = 420)
| Variables | Mean ± | a/b/ ‐value | ‐value | Scheffe's comparison |
|---|---|---|---|---|
| Personal factors | ||||
| Age | 0.12 | . | ||
| Gender | ||||
| Male | 341.70 ± 37.29 | 2.32 | . | |
| Female | 331.24 ± 40.88 | |||
| Marital status | ||||
| Single/divorced/widowed | 331.24 ± 40.49 | −1.09 | .275 | |
| Married | 335.62 ± 40.03 | |||
| Ethnicity | ||||
| Vietnamese | 334.57 ± 39.57 | 1.97 | . | |
| Other | 313.07 ± 53.73 | |||
| Religion | ||||
| No | 334.63 ± 39.39 | 0.65 | .516 | |
| Yes | 331.75 ± 42.51 | |||
| Education level | ||||
| (1) Diploma | 327.84 ± 38.20 | 7.45 | . | 3 > 1, 2 |
| (2) Associate | 327.50 ± 39.25 | |||
| (3) Bachelor's/graduate | 342.86 ± 40.80 | |||
| Self‐rated health condition | ||||
| (1) Very good | 343.94 ± 37.25 | 3.41 | . | 1 > 3 |
| (2) Good | 334.97 ± 39.47 | |||
| (3) Fair/bad/very bad | 327.06 ± 42.19 | |||
| Occupational factors | ||||
| Duration of working as a nurse | 0.15 | . | ||
| Duration of working in the current hospital | 0.13 | . | ||
| Duration of working in the specific position | 0.07 | .184 | ||
| Heard the term “critical thinking” | ||||
| No | 330.44 ± 39.68 | −2.48 | . | |
| Yes | 340.69 ± 40.56 | |||
| Work position | ||||
| (1) Nurse manager | 355.49 ± 38.53 | 23.30 | 1 > 2, 3 | |
| (2) General nurse | 329.11 ± 32.79 | |||
| (3) Administrative assistant | 322.11 ± 46.89 | |||
The bolded values indicate the level of statistical significance (with p < .05; p < .01; or p < .001) between the independent and dependent variables.
Abbreviations: SD , standard deviation.
There were statistically significant associations between the critical thinking ability and some personal‐related factors, such as age ( r = 0.12, p < .05), gender ( t = 2.32, p < .05), ethnicity ( t = 1.97, p < .05), education level ( F = 7.45, p < .01) and health condition ( F = 3.14, p < .05; Table 2 ). The findings indicated that the older nurses reported a higher critical thinking ability, and male nurses had a higher score than female ones. Vietnamese participants had higher scores than participants with other ethnicities. Participants with a bachelor's/graduate degree level of education had higher scores than participants with a diploma and associate degree level of education. Those with very good health had a higher score than participants who rated their health as fair/bad/very bad.
All of the statistically significant variables identified in the univariate analysis were selected as independent variables to determine the predictors of critical thinking ability. For the regression analysis, the categorical variables were first coded as dummy variables. The factors of having never heard of “critical thinking,” being an NM being male, being Vietnamese, having a diploma degree and being in very good health were selected as the standard factors. The results of the stepwise multiple regression method showed that there were only two predictors, namely the variables of work position and gender. Working as an AA or GN or being female can predict the critical thinking ability, and they accounted for 11% of the total variance ( F = 17.12, p < .001). This indicates that the AAs and GNs had a lower level of critical thinking than the NMs. Besides, when compared with male nurses, the female nurses exhibited a lower level of critical thinking (Table 3 ).
Predictors of the critical thinking ability ( n = 420)
| Model | Beta | ‐value | square | ‐value | ‐value | |
|---|---|---|---|---|---|---|
| Constant | 362.11 | 0.11 | 17.12 | |||
| Administrative assistant | −32.38 | −0.351 | ||||
| General nurse | −26.55 | −0.330 | ||||
| Female | −9.05 | −0.098 | . |
5. DISCUSSION
This study showed that the critical thinking ability of most professional nurses was at a low or moderate level. This finding is consistent with previous studies (Chang et al., 2011 ; Lang et al., 2013 ; Zuriguel‐Pérez et al., 2018 ). Using the same tool, Zuriguel‐Pérez et al. ( 2018 ) found that the median score of the N‐CT‐4 Practice was 363 (IQR = 340–386) for clinical nurses in Spain. Our study found a slightly lower median score (331; IQR = 311–359) but it was still in a moderate level (range of score: 329–395). Although critical thinking is a relatively new issue in Vietnamese professional nurses, it is not a brand new concept. Certain elements have been included in the nursing curriculum and clinical practice (e.g. the nursing process, problem‐based learning, evidence‐based practice). Therefore, up to 66.7% of participants had never heard the term "critical thinking," but 45.5% still reported a moderate level when measured using the N‐CT‐4 Practice (V‐v).
In Vietnam, clinical professional nurses are categorized into NMs, GNs and AAs with different job descriptions. Critical thinking ability has been identified as an important component for the high quality of care around the world, except in Vietnam. In order to identify this ability, we collected data from 3 hospitals in one region and grouped these data for analysis. Based on the comparison among NMs, GNs and AAs, it was found that NMs had a higher level of critical thinking than GNs and AAs. This can be explained by the fact that NMs have a higher age, work experience and high educational qualification than the other two groups. This result partially supports the finding that NMs report a slightly higher level of critical thinking than RNs (Zuriguel‐Pérez et al., 2018 ). Critical thinking is a necessary skill for effective and efficient management. Evidently, at present, NMs with a high level of critical thinking create positive practice environments that can help the staff nurses to deliver high quality and safe patient care (Zori et al., 2010 ). Therefore, all healthcare personnel needs to learn and apply critical thinking in order to conduct their work effectively and efficiently.
For clinical nurses, continuous in‐service education is very important to update their knowledge and skill of care. Literature found various factors associated with curriculum design and learning of critical thinking ability. Therefore, grouping subjects in the present study together in order to identify the related factors could help the development of further in‐service education of critical thinking ability effectively and efficiently. In this study, a statistically significant positive correlation was found between the critical thinking ability and age, the duration of working as a nurse and the duration of working in the current hospital. These findings are consistent with previous studies. For example, older nurses have a higher level of critical thinking than younger ones (Chang et al., 2011 ; Chen et al., 2019 ; Feng et al., 2010 ; Ludin, 2018 ; Wangensteen et al., 2010 ; Yurdanur, 2016 ; Zuriguel‐Pérez et al., 2018 ), and nurses with more experience report a better critical thinking ability than those with less experience (Chang et al., 2011 ; Chen et al., 2019 ; Feng et al., 2010 ; Ludin, 2018 ). Older and experienced nurses are more mature in their way of thinking (Chen et al., 2019 ; Ludin, 2018 ). Because there were statistically significant positive correlations among age, the duration of working as a nurse and the duration of working in the current hospital. This indicates that older nurses have a longer duration of working as a nurse or working in the current hospital so they have better critical thinking. However, the correlation between these factors and critical thinking in the current study is small; further explorations are suggested.
This study showed that there is a significant association between critical thinking ability and gender and ethnicity, which is also supported by the literature. Ludin ( 2018 ) found that female nurses reported a lower critical thinking ability than male nurses. Traditionally, females have generally had fewer opportunities to receive education and more difficulty asserting their rights during decision‐making than males in Vietnam (L. T. Nguyen et al., 2017 ). Even today, the phenomenon of gender inequality still exists in certain areas in Vietnam. This traditional burden and the limited opportunities to practice in a clinical care setting might lower the levels of the female participants’ critical thinking. Ethnicity has a similar impact, as found in the present study. For example, it has been reported that Caucasian and Hispanic/Latino participants have a significantly higher critical thinking ability than African American participants (Lang et al., 2013 ) and that Malaysian and Indian participants report different levels of critical thinking; nevertheless, only 0.9% of the participants were Indian (Ludin, 2018 ). However, in the present study, as almost all of the participants were Vietnamese (96.7%), the skewed distribution of the ethnicity might limit the generalizability of the results. In future studies, an equal distribution of ethnicity is strongly recommended.
This study also confirmed that those who had a bachelor's/graduate degree had a higher level of critical thinking than those who had a diploma or associate degree, even though the former had never heard the term "critical thinking." A vast amount of studies has found that education has a positive impact on the level of critical thinking (Chang et al., 2011 ; Gloudemans et al., 2013 ; Ludin, 2018 ; Yildirim et al., 2012 ; Zuriguel‐Pérez et al., 2018 ). Meanwhile, this study found that participants who had heard the term "critical thinking" displayed a higher level of critical thinking than those who had not heard this term. Education might be the major reason for this variation. In the present study, only 40.7% of participants had a bachelor's/graduate degree. In order to promote their levels of critical thinking, it is necessary to arrange for them, to encourage them, to attend advanced education or to provide further content in the in‐service education.
In this study, participants with very good health had a higher level of critical thinking than participants who self‐rated their health as fair/bad/very bad. Health status does have an impact on work productivity, job performance, quality of care and extra learning (Letvak et al., 2011 ). Thus, poor health limits their learning and critical thinking ability. This ability is an important predictor of real‐life outcomes (e.g. interpersonal, work, financial, health and education) (Butler et al., 2017 ). Therefore, the causal effects between health and critical thinking ability need further exploration.
In the current study, only the female gender and the type of work position as an AA or GN were identified as predictors, and they explained only 11% of the total variance of critical thinking ability in the regression model. The uneven distribution of gender and work position might be the reason for the low variance. Even though the male was significantly less than the female, NM was fewer than GN and AA. More factors need to be included in further studies.
The limitations of this study include that it used a convenience sample from only three public hospitals located in the Southwestern part of Vietnam. This sample does not represent all professional nurses in Vietnam. The N‐CT‐4 Practice is the instrument with good psychometric properties specific for clinical practice and translated into English (Zuriguel‐Pérez et al., 2017), Persian (FallahNezhad & Ziaeirad, 2018 ) and Turkish (Urhan & Seren, 2019 ). Different points of the Likert response format were selected by tools to measure critical thinking ability. For example, the N‐CT‐4 Practice selected a four‐point Likert response and it was rated in frequency, such as 1 = never or almost never and 4 = always or almost always. However, a seven‐point Likert scale for the Critical Thinking Disposition Assessment (CTDA) was selected and rated in levels of agreement, such as 1 for very strongly disagree and 7 for very strongly agree (Cui et al., 2021 ). Which response format can be more reprinting the characters of critical thinking ability? Further investigation is strongly suggested. Besides, the N‐CT‐4 Practice (V‐v) questionnaire has too many items that may lead to the boredom of the participants to answer and thus affect the accuracy of the results. Moreover, the collapsing of three distinctly separate groups of nurses into one group for most of the analyses lead to not showing differences in critical thinking and influencing factors among the three groups. These factors all limit the generalization of the present results. Based on these limitations, it is suggested that the use of nationwide systematic sampling and an international comparison are strongly suggested in further studies. Regarding the critical thinking questionnaire, it would be better to use the revised versions with fewer questions. Therefore, developmental and psychometric properties are suggested to shorten this questionnaire.
6. CONCLUSIONS
The results demonstrate that most of the professional nurses had a low or moderate critical thinking ability. Certain personal and occupational variables were significantly associated with the level of critical thinking. Being male or working as an NM were statistically significant predictors of critical thinking ability, and they explained only 11% of the total variance.
The findings of this study indicate that it is necessary to develop strategies to improve the critical thinking ability of professional nurses. The critical thinking ability has been confirmed to be an essential factor for high‐quality health care that focuses on the quality of patient care and patient safety. Besides, providing more opportunities to pursue advanced degrees or enhancing the provision of in‐service education in hospitals that involves classroom teaching or web‐based learning is strongly recommended for this specific group of nurses. Consequently, the quality of patient care could be improved.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
The authors would like to thank the expert panel, translators, research assistants, the hospitals and all of the clinical nurses who participated in this study. We are indebted to the study participants and would like to dedicate the research findings to improving the critical thinking ability of Vietnamese professional nurses in the future. No specific grant was received from funding agencies in the public, commercial, or not‐for‐profit sectors.
Van Nguyen T, Liu H‐E. Factors associated with the critical thinking ability of professional nurses: A cross‐sectional study . Nurs Open . 2021; 8 :1970–1980. 10.1002/nop2.875 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
DATA AVAILABILITY STATEMENT
- Berkow, S. , Virkstis, K. , Stewart, J. , Aronson, S. , & Donohue, M. (2011). Assessing individual frontline nurse critical thinking . Journal of Nursing Administration , 41 ( 4 ), 168–171. 10.1097/NNA.0b013e3182118528 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brunt, B. A. (2005). Critical thinking in nursing: An integrated review . The Journal of Continuing Education in Nursing , 36 ( 2 ), 60–67. 10.3928/0022-0124-20050301-05 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buerhaus, P. I. , Donelan, K. , Ulrich, B. T. , Norman, L. , & Dittus, R. (2006). State of the registered nurse workforce in the United States . Nursing Economics , 24 ( 1 ), 6. [ PubMed ] [ Google Scholar ]
- Butler, H. A. , Pentoney, C. , & Bong, M. P. (2017). Predicting real‐world outcomes: Critical thinking ability is a better predictor of life decisions than intelligence . Thinking Skills and Creativity , 25 , 38–46. 10.1016/j.tsc.2017.06.005 [ CrossRef ] [ Google Scholar ]
- Chang, M. J. , Chang, Y. J. , Kuo, S. H. , Yang, Y. H. , & Chou, F. H. (2011). Relationships between critical thinking ability and nursing competence in clinical nurses . Journal of Clinical Nursing , 20 ( 21–22 ), 3224–3232. 10.1111/j.1365-2702.2010.03593.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen, F.‐F. , Chen, S.‐Y. , & Pai, H.‐C. (2019). Self‐reflection and critical thinking: The influence of professional qualifications on registered nurses . Contemporary Nurse , 55 ( 1 ), 59–70. 10.1080/10376178.2019.1590154 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cui, L. , Zhu, Y. , Qu, J. , Tie, L. , Wang, Z. , & Qu, B. (2021). Psychometric properties of the critical thinking disposition assessment test amongst medical students in China: A cross‐sectional study . BMC Medical Education , 21 ( 1 ), 1–8. 10.1186/s12909-020-02437-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Helsinki Declaration (2013). Ethical principels for medical research involving human subject . Helsinki Declaration. [ Google Scholar ]
- FallahNezhad, Z. , & Ziaeirad, M. (2018). The relationship between the quality of working life and critical thinking of nurses in Milad Hospital of Isfahan, Iran . Preventive Care in Nursing and Midwifery Journal , 8 ( 3 ), 62–68. 10.29252/pcnm.8.3.62 [ CrossRef ] [ Google Scholar ]
- Feng, R. C. , Chen, M. J. , Chen, M. C. , & Pai, Y. C. (2010). Critical thinking competence and disposition of clinical nurses in a medical center . Journal of Nursing Research , 18 ( 2 ), 77–87. 10.1097/JNR.0b013e3181dda6f6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fero, L. J. , Witsberger, C. M. , Wesmiller, S. W. , Zullo, T. G. , & Hoffman, L. A. (2009). Critical thinking ability of new graduate and experienced nurses . Journal of Advanced Nursing , 65 ( 1 ), 139–148. 10.1111/j.1365-2648.2008.04834.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fesler‐Birch, D. M. (2005). Critical thinking and patient outcomes: A review . Nursing Outlook , 53 ( 2 ), 59–65. 10.1016/j.outlook.2004.11.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gloudemans, H. A. , Schalk, R. M. , & Reynaert, W. (2013). The relationship between critical thinking skills and self‐efficacy beliefs in mental health nurses . Nurse Education Today , 33 ( 3 ), 275–280. 10.1016/j.nedt.2012.05.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Howenstein, M. A. , Bilodeau, K. , Brogna, M. J. , & Good, G. (1996). Factors associated with critical thinking among nurses . The Journal of Continuing Education in Nursing , 27 ( 3 ), 100–103. 10.3928/0022-0124-19960501-04 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang, G. M. , Beach, N. L. , Patrician, P. A. , & Martin, C. (2013). A cross‐sectional study examining factors related to critical thinking in nursing . Journal for Nurses in Professional Development , 29 ( 1 ), 8–15. 10.1097/NND.0b013e31827d08c8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee, D. S. , Abdullah, K. L. , Subramanian, P. , Bachmann, R. T. , & Ong, S. L. (2017). An integrated review of the correlation between critical thinking ability and clinical decision‐making in nursing . Journal of Clinical Nursing , 26 ( 23–24 ), 4065–4079. 10.1111/jocn.13901 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Letvak, S. , Ruhm, C. , & Lane, S. (2011). The impact of nurses' health on productivity and quality of care . JONA. The Journal of Nursing Administration , 41 ( 4 ), 162–167. 10.1097/NNA.0b013e3182118516 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu, N.‐Y. , Hsu, W.‐Y. , Hung, C.‐A. , Wu, P.‐L. , & Pai, H.‐C. (2019). The effect of gender role orientation on student nurses’ caring behaviour and critical thinking . International Journal of Nursing Studies , 89 , 18–23. 10.1016/j.ijnurstu.2018.09.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Locke, R. , Leach, C. , Kitsell, F. , & Griffith, J. (2011). The impact on the workload of the ward manager with the introduction of administrative assistants . Journal of Nursing Management , 19 ( 2 ), 177–185. 10.1111/j.1365-2834.2011.01229.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ludin, S. M. (2018). Does good critical thinking equal effective decision‐making among critical care nurses? A cross‐sectional survey . Intensive & Critical Care Nursing , 44 , 1–10. 10.1016/j.iccn.2017.06.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mahmoud, A. S. , & Mohamed, H. A. (2017). Critical thinking disposition among nurses working in puplic hospitals at port‐said governorate . International Journal of Nursing Sciences , 4 ( 2 ), 128–134. 10.1016/j.ijnss.2017.02.006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ministry of Health (1997). Decision No. 1895/1997/QĐ‐BYT of the ministry of health on the promulgation of Hospital Regulations . Retrieved from http://vbpl.yte.gov.vn/van‐ban‐phap‐luat/quyet‐dinh‐18951997qd‐byt‐.1.2286.html
- Ministry of Health (2011). Circular No. 07/2011/TT‐BYT dated 26/01/2011 of the Ministry of Health on guiding on patient care in hospitals . Retrieved from https://kcb.vn/wp‐content/uploads/2015/07/TT‐07.2011.TT‐BYT‐ngay‐26.01.2011.pdf .
- Nguyen, L. T. , Annoussamy, L. C. , & LeBaron, V. T. (2017). Challenges Encountered by Vietnamese Nurses When Caring for Patients With Cancer . Paper presented at the Oncology nursing forum. [ PubMed ]
- Nguyen, T. V. , & Liu, H. E. (2021). The Vietnamese version of the nursing critical thinking in clinical practice questionnaire: Translation and psychometric evaluation . Nursing Open , 1–8. 10.1002/nop2.834 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pallant, J. (2010). SPSS survival manual: A step by step guide to data analysis using SPSS . Maidenhead. Open University Press/McGraw‐Hill. [ Google Scholar ]
- Ryan, C. , & Tatum, K. (2012). Objective measurement of critical‐thinking ability in registered nurse applicants . Journal of Nursing Administration , 42 ( 2 ), 89–94. 10.1097/NNA.0b013e318243360b [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Suresh, K. , & Chandrashekara, S. (2012). Sample size estimation and power analysis for clinical research studies . Journal of Human Reproductive Sciences , 5 ( 1 ), 7. 10.4103/0974-1208.97779 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ] Retracted
- Urhan, E. , & Seren, A. K. H. (2019). Validity and reliability of Turkish version of the nursing critical thinking in clinical practice questionnaire . University of Health Sciences Journal of Nursing , 1 ( 3 ), 147–156. [ Google Scholar ]
- Van Dyk, J. , Siedlecki, S. L. , & Fitzpatrick, J. J. (2016). Frontline nurse managers' confidence and self‐efficacy . Journal of Nursing Management , 24 ( 4 ), 533–539. 10.1111/jonm.12355 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , Vandenbroucke, J. P. , & Initiative, S. (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies . International Journal of Surgery , 12 ( 12 ), 1495–1499. 10.1016/j.ijsu.2014.07.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wangensteen, S. , Johansson, I. S. , Bjorkstrom, M. E. , & Nordstrom, G. (2010). Critical thinking dispositions among newly graduated nurses . Journal of Advanced Nursing , 66 ( 10 ), 2170–2181. 10.1111/j.1365-2648.2010.05282.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wong, C. A. (2015). Connecting nursing leadership and patient outcomes: State of the science . Journal of Nursing Management , 23 ( 3 ), 275–278. 10.1111/jonm.12307 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yildirim, B. , Özkahraman, Ş. , & Ersoy, S. (2012). Investigation of critical thinking disposition in nurses working in public hospitals . International Journal of Business, Humanities and Technology , 2 , 61–67. [ Google Scholar ]
- Yurdanur, D. (2016). Critical Thinking Competence and Dispositions among Critical Care Nurses: A Descriptive Study . International Journal , 9 ( 2 ), 489. [ Google Scholar ]
- Zori, S. , Nosek, L. J. , & Musil, C. M. (2010). Critical thinking of nurse managers related to staff RNs’ perceptions of the practice environment . Journal of Nursing Scholarship , 42 ( 3 ), 305–313. 10.1111/j.1547-5069.2010.01354.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zuriguel‐Pérez, E. , Falcó‐Pegueroles, A. , Roldán‐Merino, J. , Agustino‐Rodriguez, S. , Gómez‐Martín, M. C. , & Lluch‐Canut, M. T. (2017). Development and psychometric properties of the nursing critical thinking in clinical practice questionnaire . Worldviews on Evidence‐Based Nursing , 14 ( 4 ), 257–264. 10.1111/wvn.12220 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zuriguel‐Pérez, E. , Lluch Canut, M. T. , Falcó Pegueroles, A. , Puig Llobet, M. , Moreno Arroyo, C. , & Roldán Merino, J. (2015). Critical thinking in nursing: Scoping review of the literature . International Journal of Nursing Practice , 21 ( 6 ), 820–830. 10.1111/ijn.12347 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zuriguel‐Pérez, E. , Lluch‐Canut, M. T. , Agustino‐Rodríguez, S. , Gómez‐Martín, M. D. C. , Roldán‐Merino, J. , & Falcó‐Pegueroles, A. (2018). Critical thinking: A comparative analysis between nurse managers and registered nurses . Journal of Nursing Management , 26 ( 8 ), 1083–1090. 10.1111/jonm.12640 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Open access
- Published: 05 September 2024
Breaking the taboo of using the nursing process: lived experiences of nursing students and faculty members
- Amir Shahzeydi ORCID: orcid.org/0000-0001-9095-2424 1 , 2 ,
- Parvaneh Abazari ORCID: orcid.org/0000-0003-4024-2867 3 , 4 ,
- Fatemeh Gorji-varnosfaderani ORCID: orcid.org/0000-0001-6830-982X 5 ,
- Elaheh Ashouri ORCID: orcid.org/0000-0002-7566-6566 6 ,
- Shahla Abolhassani ORCID: orcid.org/0000-0002-5191-7586 6 &
- Fakhri Sabohi ORCID: orcid.org/0000-0003-1448-6606 6
BMC Nursing volume 23 , Article number: 621 ( 2024 ) Cite this article
Metrics details
Despite the numerous advantages of the nursing process, nursing students often struggle with utilizing this model. Therefore, studies suggest innovative teaching methods to address this issue. Teaching based on real clinical cases is considered a collaborative learning method that enhances students’ active learning for the development of critical thinking and problem-solving skills. In this method, students can acquire sufficient knowledge about patient care by accessing authentic information.
The aim of the present study was to investigate the experiences of nursing students and faculty members regarding the implementation of nursing process educational workshops, based on real case studies.
A qualitative descriptive study.
Participants
9 Nursing students and 7 faculty members from the Isfahan School of Nursing and Midwifery who attended the workshops.
This qualitative descriptive study was conducted from 2021 to 2023. Data was collected through semi-structured individual and focus group interviews using a qualitative content analysis approach for data analysis.
After analyzing the data, a theme titled “Breaking Taboos in the Nursing Process” was identified. This theme consists of four categories: “Strengthening the Cognitive Infrastructure for Accepting the Nursing Process,” “Enhancing the Applicability of the Nursing Process,” “Assisting in Positive Professional Identity,” and “Facilitating a Self-Directed Learning Platform.” Additionally, thirteen subcategories were obtained.
The data obtained from the present study showed that conducting nursing process educational workshops, where real clinical cases are discussed, analyzed, and criticized, increases critical thinking, learning motivation, and understanding of the necessity and importance of implementing the nursing process. Therefore, it is recommended that instructors utilize this innovative and effective teaching method for instructing the nursing process.
Peer Review reports
Introduction
The nursing process is a systematic and logical method for planning and providing nursing care [ 1 ] that provides an opportunity for nurses to efficiently and dynamically utilize their knowledge and expertise. It also creates a common language, known as nursing diagnosis, which facilitates action, promotes creative solutions, and minimizes errors in patient care [ 2 ]. Clinical education, based on the nursing process, provides an appropriate setting for nursing students to gain clinical experiences and foster professional development [ 3 ].
Despite the numerous advantages, nursing students face difficulties in implementing this model in various countries [ 4 , 5 ], lack of appropriate knowledge, lack of clinical practice, and insufficient learning are among the most significant obstacles to the implementation of the nursing process by students. This can be attributed to the poor quality of education regarding this important nursing care model. Therefore, it is necessary for educators in this field to use innovative and participatory teaching methods [ 3 , 6 ]. According to research conducted in Iran, 72% of nursing faculty members use passive teaching methods. Meanwhile, 92% of nursing students prefer active and innovative learning methods over traditional and passive methods [ 7 ]. Therefore, the use of modern methods, which aim to stimulate students’ thinking and enhance their responsiveness in acquiring and applying knowledge, can be effective [ 6 ].
Case-based learning is a collaborative learning method that aims to develop and enhance critical thinking and problem-solving skills [ 8 ]. Teaching the nursing process based on clinical and real cases can be very important in terms of promoting critical thinking, simulating real experiences, enhancing clinical judgment, and ultimately improving the quality and effectiveness of education [ 8 , 9 ]. In this method, students gain sufficient knowledge about patient care by accessing real information, improving their skills in patient assessment, and gaining personal nursing experience. This leads to a better understanding of comprehensive care and prepares individuals for future professional roles [ 9 ].
Very few studies have been conducted on teaching methods and their impact on the quality of nursing process [ 10 , 11 ]. In Iran, case-based trainings have mostly focused on hypothetical cases [ 1 , 12 ]. In other countries, most studies conducted on the case-based educational method have not focused on the nursing process. The few studies that have been conducted on the nursing process have either not been based on real clinical cases [ 13 ] or, if clinical cases have been researched, the studies have been conducted quantitatively [ 8 , 9 ] While qualitative research provides researchers with more opportunities to discover and explain the realities of the educational environment and gain a better understanding of many challenging aspects related to the nursing education process. Researchers are able to provide a practical model that helps improve and enhance the current process by gaining insight and a deep understanding of what is happening in the field of study [ 14 ]. This study represents the first qualitative research that describes the lived experiences of nursing students and faculty members regarding the teaching of the nursing process through real-based case workshops.
Study design
This qualitative descriptive study was conducted from 2021 to 2023. Qualitative descriptive studies typically align with the naturalistic inquiry paradigm, which emphasizes examining phenomena in their natural settings as much as possible within the context of research. Naturalistic inquiry, rooted in a constructivist viewpoint, enables a deeper understanding of phenomena by observing them within the authentic social world we inhabit [ 15 ]. In this type of study, researchers provide a comprehensive summary of an extraordinary occurrence or circumstance of interest and its related factors, but they do not delve into deep interpretation [ 16 ]. This study was undertaken to explore students and faculty members perceptions of the effect of the educational workshops on knowledge, skills and attitudes of students to the nursing process.
Setting and sample
Participants were selected from nursing students and faculty members who participated in nursing process workshops (Table 1 ). The criteria for entry into the study included volunteering to participate in the study and attending at least 3 sessions of the workshops.
Workshop details
The workshops were held in the conference hall of the Nursing and Midwifery Faculty. They consisted of 9 sessions, each lasting 2 h, from 16:00 to 18:00. Students from terms 2 to 8 and faculty members participated in these workshops. Each session was attended by an average of 60 members. Despite the inconvenience of scheduling the sessions outside of the official class hours, all the members stayed until the end of the meeting, showing a keen interest in the material and actively participating in discussions. Attendance was open to all students and faculty members, and participants in each of the workshop sessions were not the same.
It should be noted that all workshops were accompanied by a specialized instructor in the field of the nursing process, as well as a specialized instructor in the field of the specific disease being discussed. The details of these workshops are summarized in three stages:
First Stage
Step 1 . The researcher visited one of the inpatient clinical wards of the hospital based on the assigned topic for each workshop. They selected a patient, conducted a comprehensive assessment, and recorded the information using Gordon’s assessment form. This included the patient’s current and past medical history, paraclinical tests, physical examinations, medications, and information gathered from credible sources such as interviews with the patient and their family, medical records, and the patient’s treatment and care interventions documented in their medical file and Cardex.
Step 2 . Preparing the presentation file, which includes the following items:
Writing the comprehensive patient assessment based on step one.
Writing actual and at-risk nursing diagnoses according to PES (Problem/ Etiology/ Signs and Symptoms) and PE (Problem/ Etiology) rules, as well as collaborative problems, and then prioritizing them based on Maslow’s Hierarchy of Needs.
Writing objectives and outcomes for each nursing diagnosis based on the SMART (Specific/ Measurable/ Attainable/ Realistic/ Time Bound).
Writing nursing interventions (based on objectives and outcomes), along with the rationales according to evidence-based, up-to-date, and reliable sources for each intervention.
Step 3 . Sending the presentation file to an expert professor in the field of nursing process for review and implementing her comments.
Second stage
Step 1 . Announcing the date and time of the workshop session to students and faculty members.
Step 2 . Providing students and faculty members with a comprehensive patient assessment.
Third stage (workshop implementation)
Step 1. Presenting all stages of the nursing process based on the case study:
Providing a comprehensive assessment of the patient’s condition. (Giving time for students, faculty members, and presenters to discuss with each other, express their comments, and summarize)
Presenting diagnoses along with the objectives and expected outcomes. (Giving time for students, faculty members, and presenters to discuss with each other, express their comments, and summarize)
Presentation of nursing interventions. (Giving time for students, faculty members, and presenters to discuss with each other, express their comments, and summarize)
Presentation on assessing the level of achievement of expected outcomes and evaluating interventions. (Giving time for students, faculty members, and presenters to discuss with each other, express their comments, and summarize)
Data Collection Tools
Demographic questionnaire.
It included age, gender, Position, degree and number of sessions attended in the workshop.
Semi-structured interview
It included the following questions:
What was your motivation to attend these meetings?
Before entering the nursing process meetings, what did you expect from the meeting?
How many of your expectations were met by participating in the meetings?
How much did these meetings help you in applying the nursing process in the clinical setting?
What do you think about the continuation of such meetings?
Data collection
After obtaining official permission from the university in 2021, the phone numbers of students and faculty members who participated in more sessions of the workshop were collected in 2023. A specific time and location were subsequently arranged to contact and interview participants who had indicated their willingness to take part in the study. Approximately 40 individuals expressed their consent to participate; however, data saturation was achieved after interviewing 16 participants. It is important to note that interviews were conducted through both individual sessions and focus groups. Individual interviews were carried out with 3 faculty members, while two focus groups were conducted separately with 9 students and 4 faculty members.
Individual Interviews
The interviews were conducted in a semi-structured manner and began with a general question to establish initial and closing communication. These interviews were conducted by one of the researchers who holds a PhD in nursing and has published several qualitative articles in reputable journals. In each of these sessions, the interviewer introduced themselves and welcomed the participants. The goals of the session were discussed, and participants were given complete freedom to express their opinions. The interviewer refrained from interfering or reacting to their opinions, and the information discussed was kept completely confidential under the guise of a code. Participants were subsequently asked to provide consent for voice recording during the interviews. Once consent was obtained from the participants, their voices were recorded. Each individual interview lasted between 30 and 45 min.
Focus Group Interviews
All the conditions of these interviews were similar to individual interviews. However, in focus group sessions, an additional researcher acted as an assistant to the main interviewer. The assistant’s role was to determine the order of speaking based on the participants’ requests, observe their facial expressions while speaking, and take necessary notes. Each of the focus group sessions lasted approximately 5 h. It should be noted that participant selection and sampling continued until data saturation was achieved. Saturation of data refers to the repetition of information and the confirmation of previously collected data.
Data analysis
The qualitative content analysis approach proposed by Graneheim and Lundman was used for data analysis [ 16 ]. The recorded interviews were transcribed verbatim (The transcripts were sent to the participants for feedback and were approved by them), and then each word was carefully examined to identify codes Two independent individuals encoded the data. Words that accurately represented thoughts or concepts within the data were highlighted. Then, the researcher added her own notes about his thoughts, interpretations of the text, and initial analysis of the text. With the progression of this process, appropriate names for the codes emerged, and the codes were organized into subcategories. These subcategories were created to organize and categorize the codes within clusters. The researcher reorganized the subcategories based on their relationships, condensing them into a smaller number of organizational categories. And then the concepts of each category, subcategory, and code were developed.
Trustworthiness
Data was managed using the Lincoln and Guba criteria. These criteria include acceptability, which is equivalent to internal validity; transferability, which is equivalent to external validity; similarity, which is equivalent to reliability; and verifiability, which is equivalent to objectivity [ 17 ]. The use of member checks by participants is considered a technique for exploring the credibility of results. In this regard, the interview text and the primary codes extracted from it were made available to several participants to verify the accuracy with their experiences. External supervision was employed to ensure that the criterion of internal consistency was met. For this purpose, the data was given to a researcher who did not participate in the study. If there was agreement in the interpretation of the data, it confirmed the presence of internal consistency. Finally, an audit or verification inquiry was conducted. The researcher accurately recorded and reported all stages and processes of the research from beginning to end. This allows external supervisors to conduct audits and assess the credibility of the findings.
Data analysis resulted in the emergence of 13 subcategories, 4 categories, and 1 theme (Table 2 ).
Strengthening the intellectual infrastructure of accepting the nursing process
Subcategories such as “improving nursing perception,” “strengthening critical thinking,” “evidence-based nursing practice,” and “filling an educational gap” contributed to the emergence of the category “Strengthening the intellectual infrastructure of accepting the nursing process.”
Improving nursing perception
Participants’ experiences indicate the significant positive impact of the workshop on improving students’ perception of the nursing process. Most nurses in departments do not provide patient care based on the nursing process. As a result, students do not have the opportunity to practically experience the real application of the nursing process in the department. Instead, they only perceive the nursing process as a written task.
For me, it was a question of what the nursing process is, for instance. How difficult is it?” and it really helped me overcome my fear in a way. (P3 student) Usually, they would explain the nursing process to us, but it was not practical or based on real cases, like this. (P1 Student)
Strengthening critical thinking
Critical thinking is a fundamental skill in the nursing process that involves various stages and activities. These include questioning to gather adequate information, validating and analyzing information to comprehend the problem and its underlying factors, evaluating interventions, and making appropriate decisions for effective problem-solving. The experiences of the participating students clearly reflected the formation of these stages during the workshop sessions.
I learned in the workshop about the importance of using critical thinking to successfully connect knowledge and practice. It’s a shame that critical thinking has not been cultivated in the minds of students, and these workshops have laid the foundation for it in our minds. (P6 student) Students often come across hypothetical cases in textbooks, but when they are confronted with real cases, the circumstances are different… This is when critical thinking becomes crucial and the art of nursing is demonstrated… These sessions have made a significant contribution to this subject. (P15 Faculty member)
Evidence-based nursing practice
One of the features of the sessions was that in introducing the case from assessment to evaluation, to justify the rationale and process of collecting and formulating nursing diagnoses, establishing expected outcomes, and providing reasons for each intervention, relied on up-to-date and reliable nursing and medical resources
It had a strong scientific foundation, consistently emphasizing the importance of evidence-based practices and a scientific approach, effectively communicating this perspective to audience. (P2 Student). I became familiar with the book ‘Carpenito,’ and it helped me a lot in understanding my shortcomings. (P3 student). In my opinion, one of the factors that contributed to the effectiveness of the work was consulting the references. They emphasized that as a nurse, I should not solely rely on my personal opinion but should instead base my actions on the reference materials (P14 Faculty member).
Filling an educational gap
From the perspective of workshop participants, the workshop has increased their awareness of their limited knowledge about the application of the nursing process. It has also helped them recognize their shortcomings, and motivated them to pursue additional studies in this field.
Exactly, there was a vacant spot for this educational program in our classes. And there should have been sessions that would prove to us that nursing is not just about the theoretical concepts that faculty members teach in class. (P5 Student) The nursing process has a theoretical aspect that students learn, but when they attempt to apply it in practice, they often encounter difficulties. These sessions helped to fill the gap between theory and practice. (P15 Faculty member)
Practicality of the nursing process
Subcategories of “linking the nursing process with team care,” “demonstrating the role of the nursing process in improving care quality,” “comprehensive view in care,” and “student’s guiding light in the clinic,” Created the category “Practicality of the Nursing Process”.
Linking the nursing process with team care
Participants’ experiences indicated that participating in nursing process sessions helped them realize that the nursing process is a model that will lead to collaborative team care. Prior to attending these sessions, nursing students like nurses considered their duty to be solely executing medical orders under the supervision of clinical faculty members and staff nurses.
I realized that in certain situations, I am able to confidently express my opinion to the doctor. For instance, if I believe that a particular course of action would yield better results, I can easily communicate this and provide reasons to support my viewpoint (P7 Student). Teaching the pathway when it’s categorized with knowing what we’re assessing… Let’s go up to the patient; our confidence can really guide them along with us as we progress step by step and systematically. Often, the patient accompanies us, and sometimes they voice their unspoken concerns, which helps improve their care. It means the patient themselves are partnering with us. (P6 student)
Demonstrating the role of the nursing process in improving care quality
Strengthening the attitude and belief in the role and application of the nursing process in improving the quality of care was another concept that emerged from the experiences of the students. Presenting reports on the implementation of the nursing process on real cases led them to believe that providing care based on the nursing process results in organized care planning and enhances the quality of care.
In these workshops, the needs of patients were prioritized, documented, and then organized systematically. This concept remains ingrained in a person’s mind and enables us to deliver comprehensive care to the patient without overlooking any aspect. This has been very helpful for me, and now it greatly assists me in the clinic. (P4 Student) Another great aspect of these sessions was the emphasis they placed on the nurse-patient relationship. I could see that the students had been following up with patients for a while and implementing the process. This was very helpful to me. For instance, diagnosing based on the patient’s current health status was an ongoing process. In my opinion, the connection between the patient and nurse was more important and practical for me.(P1 Student).
Comprehensive view in care
Attention to the patient’s care needs went beyond focusing solely on physiological aspects. It involved a holistic approach that addressed the patient’s needs related to all aspects of biology, psychology, society, spirituality, and economics. This was clearly reflected in the students’ experiences during the nursing process sessions.
…I paid attention to all aspects of the patient. For example, perhaps I overlooked her anxiety issue and never took it into consideration. However, I eventually came to realize that addressing anxiety is crucial, as it is one of the primary concerns and needs of patients. (P2 Student) …that the students had a holistic view of the patient (they had examined the patient thoroughly, including the patient’s skin, etc.) and had compiled a list of the patient’s issues, paying attention to all aspects of the patient (P14 Faculty member).
Student’s guiding light in the clinic
One of the significant accomplishments of nursing process sessions, as evidenced by the students’ experiences, was the role of these sessions in assisting students in overcoming confusion and uncertainty during their internships. These sessions enabled them to establish a mental connection between the theoretical knowledge learned in the classroom and its application in the real clinical setting, also helped them understand how to effectively utilize their theoretical knowledge in a clinical learning environment.
.I was feeling incredibly lost and confused. I didn’t know what steps to take next. Many of us find ourselves in this situation, unsure of what to do. At least for me, as someone who grasps concepts better through examples, the case-based studies conducted during the workshop had a significant impact. (P6 Student)
Supporting a positive professional identity
Two subcategories, “highlighting the importance of nursing science” and “reforming the perception of nursing nature,” have contributed to the development of the category “supporting a positive professional identity.”
Highlighting the importance of nursing science
Based on students’ experiences, the nursing process sessions have been able to answer an important question. Why should they be bombarded with information and expected to possess extensive knowledge in the field of disease recognition, pathophysiology, diagnosis, treatment, and nursing care during their studies? The students believed that the content of the nursing process sessions clarified the necessity and importance of nursing knowledge for them. In these sessions, they came to believe that providing care based on the nursing process requires extensive nursing knowledge.
. In my opinion, this work showcases a significant strength by highlighting the importance of working scientifically as a nurse. Personally, I feel its impact on myself is profound. (P2 Student) In my opinion, it was very touching and captivating because it accurately portrayed the immense power of a nurse. However, amidst the demanding and difficult nature of the job, what specific details should a nurse pay attention to? and it is precisely these details that shape the work of a nurse. It was very interesting and beneficial for me. (P5 student)
Reforming the perception of nursing nature
The student is seeking ways to comprehend and value the practical aspects of nursing as a genuine science, assuming that nursing is indeed regarded as a science. Participants’ experiences have shown that nursing process sessions have been able to address this identity challenge and modify and enhance students’ understanding of the nature of nursing.
I used to believe that nursing was primarily an art complemented by science until I entered term 2 and participated in these workshops. And now I realize that it has the scientific foundation that I expected from an evidence-based practice. (P5 student). . The important point was that lower-term students, who sometimes lacked motivation and thought nursing had nothing to offer, gained motivation and had a change in perspective by attending these sessions. (P2 faculy members)
Self-directed learning facilitator
Subcategories of “stimulating a thirst for learning,” “creating a stress-free learning atmosphere,” and “teaching fishing,” formed the category of “self-directed learning facilitator.”
Stimulating a thirst for learning
Participants’ experiences indicated that the format of conducting sessions, ranging from step-by-step training to training accompanied by multiple examples, had a significant impact on creating a sense of necessity and stimulating learners’ motivation to learn.
First of all, the challenges that you yourself raised (faculty member) for example, why did you make this diagnosis?” Why did you include this action? Why is this a priority? Really, it shook me and made me think that maybe there is more to this, maybe there is more to the nursing process that I haven’t understood yet…. That’s why it became my motivation. (P3 student) …But these sessions helped me a lot. At least, they sparked my curiosity and motivated me to delve deeper into the subject. I began actively participating in these sessions and found them to be highly effective for my personal growth. (P6 student) In my opinion, one of the things that empowered the work was the act of seeking references. They emphasized that as a nurse, I should not solely rely on my personal opinion but should instead base my actions on credible sources. (P14 Faculty member)
Creating a stress-free learning atmosphere
Students believed that the absence of a legal requirement to attend these workshops, coupled with the understanding that their participation or non-participation would not be evaluated for grading purposes, would enable them to engage in these sessions without concern for their academic performance and in accordance with their own volition.
I was more scared… In my internships, for example, we would sit and talk with the instructor. However, the discussions primarily revolved around grades and other academic matters, which created a stressful environment where students were hesitant to freely express their thoughts. But the sessions here are very relaxed, and students no longer have the fear of grades. (P7 student) The essence of these sessions was that they came from the heart and inevitably touched the heart. The beauty of this program was that it was built on love. (P10 Faculty member)
Teaching fishing
Direct reference to teaching fishing in the participants’ experiences points to one of the very important features that effectively prepares the way for self-guided learning. The term “teaching fishing” was repeatedly mentioned in the participants’ experiences. They believed that these sessions served as a roadmap to easily enhance their knowledge and skills in the field of nursing process application.
.And actually, teaching fishing, as mentioned by other students, is important. In my opinion, it has a positive impact both professionally and in terms of the effectiveness of the nursing process. (P2 student) The important aspect was the involvement and full participation of the students, who prepared the materials themselves… The meaning and concept of being a student were more evident, and the talents of the students flourished. They actively participated in discussions about learning and education. (P15 Faculty member)
Planners, in their efforts to help students gain a better understanding of the nature and application of the nursing process, are constantly striving to innovate in teaching this model. The aim of the present study was to describe and explain the experiences of nursing students and faculty during clinical-based nursing process workshops involving real cases.
Hanisch et al. (2020) recommend using data from actual patients [ 18 ], and Yilmaz et al. (2015) suggest providing nursing students with opportunities to apply the nursing process in diverse patient populations during clinical training [ 19 ]. The study conducted by Karimi et al. (2011) demonstrated that organizing nursing process classes as workshops stimulated a sense of competition and superiority both among and within groups. This approach also enhanced participants’ concentration on learning the content of each session. In addition, the workshop fostered a sense of cooperation and cohesion among the students, which was evident in their increased interest and excitement [ 1 ]. The importance of utilizing workshop-based training with real clinical cases is clearly evident. When students receive data related to a real patient, they directly experience the clinical environment. This, in turn, leads to an improvement in their critical thinking and decision-making skills when they encounter similar cases. For this purpose, nursing educators can present the rich clinical cases they encounter during their internships in theory classes based on the stages of the nursing process. They can also ask students to present these cases for their peers to comment on and critique the care provided, in order to stimulate discussion.
The category of " Strengthening the intellectual infrastructure of accepting the nursing process " indicates that the teaching method used in this study has been able to help students better understand and recognize the nature and improvement of insight into the nursing process. In the study by Thuvaraka et al. (2018), 52% of participants strongly agreed on the necessity of having a positive attitude and insight towards the nursing process for its proper implementation [ 20 ]. According to the study by Mert et al. (2020), a lack of insight into the nursing profession and process can even lead students to consider dropping out of their studies [ 21 ]. The importance of reviewing the nursing education process to enhance this perception has been emphasized in various studies. Zamanzadeh et al. (2015) discuss several challenges in the implementation of the nursing process. These challenges include a lack of clarity regarding its meaning, differences in perspectives, and insufficient training leading to a lack of awareness on how to properly implement it [ 22 ]. More than 90% of students (93.5%) in the study conducted by Rajabpoor et al. (2018) [ 4 ] and over two-thirds (75.6%) of students in the study conducted by Sharghi et al. (2015) identified lack of proper training and insufficient time allocated for teaching as the most significant barriers to implementing the nursing process. They attributed this to traditional and routine teaching methods [ 23 ]. This causes students to undervalue the nursing process, perceiving it only at a theoretical level rather than practical. As a result, they become overwhelmed by the routine when working as clinical nurses [ 7 ]. Therefore, by teaching the case method based on real clinical cases, nursing instructors can strengthen students’ positive outlook and ability to apply the nursing process. This increases the percentage of students implementing the nursing process in clinical wards.
Strengthening critical thinking is one of the concepts derived from analyzing the experiences of the students and faculty who participated in the present study. Based on a review study by Carvalho et al. (2017), the utilization of the nursing process, particularly the stage of nursing diagnosis formulation, enables nurses to employ critical thinking in making judgments and providing clinical care [ 24 ]. This process also helps ensure the delivery of high-quality care [ 25 ]. But if the nursing process is presented in an undesirable manner, it suppresses critical thinking. According to Heidari et al. (2016), the nursing process resulted in students relying on copying from books, which led to a decline in creativity and an increase in their dissatisfaction [ 26 ]. According to the study conducted by Ghanbari et al. (2017), the implementation of collaborative workshops focused on the nursing process resulted in an improvement in critical thinking skills among nursing students [ 3 ]. Therefore, nursing instructors can teach theoretical classes based on the clinical cases they have experienced in the hospital. By doing so, students can immerse themselves in the clinical environment during theoretical classes, which significantly enhances their critical thinking skills.
The evidence-based nursing display was one of the achievements of nursing process educational workshops, which were based on real cases. Mackey et al. (2017) consider evidence-based practice as a means to bridge the gap between theory and practice in nursing education for undergraduate and graduate students [ 27 ]. And likewise, Sin et al. (2017) believe that nursing faculties are obligated to enhance the competence and knowledge of students for evidence-based practice by employing innovative methods [ 28 ]. Therefore, it is recommended that nursing instructors use up-to-date scientific references for nursing interventions when teaching about the nursing process of diseases. This practice helps students feel that the care they provide is supported by scientific evidence and motivating them to carry out nursing care more effectively.
One of the emerging concepts in this study was the focus on the practicality of the nursing process. In the study conducted by Agyeman-Yeboah et al. (2017), participants reported that new students and nurses tend to neglect the implementation of the nursing process when they observe experienced nurses failing to apply it in a scientific and systematic manner [ 5 ]. The lack of implementation of the nursing process by nurses is due to a lack of knowledge and a negative attitude towards it. Zerihun Adraro and Adugna Cherkos (2021) conducted a study in Ethiopia and found that the majority of nurses had inadequate knowledge, and half of them lacked a positive attitude towards the implementation of the nursing process [ 29 ]. In the study by Thuvaraka et al. (2018), only 17% of nurses had sufficient knowledge about the nursing process and implemented it [ 20 ]. One of the important experiences for students in the “Practicality of the Nursing Process” category is the development of their participatory and interprofessional spirit. They are encouraged to express their opinions about the care and treatment process of patients, rather than blindly following the doctor’s orders. According to a systematic review study, the level of physicians’ proficiency in their management systems is a significant issue for the healthcare system [ 22 ]. According to the study conducted by Nakhaee et al. (2017), doctors are the ones responsible for making decisions regarding all patient matters, while the efforts of nurses often go unappreciated. This lack of recognition can result in a decline in their self-esteem [ 30 ]. While according to Adamy et al. (2019), the implementation of the nursing process at a professional level is highly effective in creating an independent nursing role, rather than just serving as assistants to physicians. This implementation also enhances the credibility of the nursing profession [ 31 ]. The recommendation of the present researchers to nursing instructors is to take a significant step in enhancing the knowledge and independent spirit of nursing students by basing their teaching on real clinical cases. When students perceive that they have independence and are not merely following doctors’ orders, their engagement in operationalizing the nursing process and evidence-based care will increase.
Strengthening the holistic perspective was one of the positive experiences for students and faculty members who attended these workshops. According to the study by Hackett et al. (2017), physical problems can result in mental stress among patients. Therefore, it is essential to consider all dimensions of care [ 32 ]. According to Ericsson (1995), humans should be considered as a whole, and nursing care should be tailored to address biological, psychological, social, and spiritual aspects [ 33 ]. The importance of holistic care has been emphasized by Florence Nightingale, who encouraged caregivers to practice it [ 34 ]. Holistic care emphasizes partnership and dialogue between nurse and patient about health care needs [ 35 ]. Adequate training is crucial in ensuring that nurses and nursing students are well-prepared to meet the diverse needs of patients and deliver comprehensive care [ 36 ]. It is recommended for nursing instructors to focus on the mental aspect in addition to the physical aspect when teaching the nursing process and encourage students to apply this approach during clinical internships.
Another advantage of these sessions was the successful implementation of the nursing process in apprenticeship. Work disorder and confusion in implementing the nursing process are significant challenges. According to the study by Korkut et al. (2021), students were unable to collect appropriate data from their patients and were confused when formulating and prioritizing nursing diagnoses, determining goals, and planning care. However, due to the fear of receiving a low grade, they were compelled to present fabricated data [ 37 ]. Therefore, nursing instructors should incorporate real clinical cases encountered during internships into their theoretical classes. This simulation helps students perform better in implementing the nursing process in the hospital environment later on.
During these workshop sessions, the students’ awareness of the professional identity of nursing was heightened. They came to understand that this professional identity is a crucial principle that underpins their comprehension of nursing and scientific care. As a result, they recognized the significance of studying pathophysiology and the fundamental principles of scientific care for different diseases. Professional identity is described as a person’s perception of themselves within a profession or the collective identity of the profession [ 38 ]. In nursing, professional identity plays a crucial role in delivering high-quality services to patients [ 39 ] because it effectively enhances clinical competence, self-assurance, self-esteem, and interpersonal communication skills [ 40 , 41 ]. In this regard, the study by Sun et al. (2016) found that professional identity and education level had the greatest impact on the stress levels of nursing students. The results of that study showed that developing and enhancing professional identity could be beneficial for nursing students in managing stress [ 42 ]. Similarly, according to the study by Sabanciogullari et al. (2015), there was a positive and significant correlation between nurses’ job satisfaction and professional identity. This study found that 15.5% of nurses who intended to leave their profession had insufficient professional identity and lower job satisfaction. Professional identity is a significant factor in job satisfaction [ 41 ]. According to the study by Van der Cingel et al. (2021), a lack of attention to the professional identity of nursing contributes to the departure of nursing students and young nurses from the nursing profession [ 43 ]. Therefore, focusing on professional identity in nursing education is crucial and should be a primary objective [ 38 ], despite findings from Haghighat et al. (2019) indicating that nursing education programs in Iran have not effectively nurtured nursing students [ 44 ]. This highlights a greater focus on teaching based on real clinical cases, which enhances the professional identity of nursing and facilitates the implementation of the nursing process.
“Self-directed learning facilitator” is one of the important categories identified in the present study. It encompasses three crucial concepts: “stimulating a thirst for learning”, “creating a stress-free learning atmosphere”, and “teaching fishing”. The students’ experiences indicated that engaging in discussions, asking questions, and providing answers had a significant impact on motivating them to study and enhancing their motivation for learning. This learning took place in a calm and stress-free environment. Participants were able to analyze the content calmly, as grades were not involved. As a result, they were able to diagnose what to prioritize in a clinical setting, even without the assistance of a clinical instructor. In fact, during these sessions, the instructors focused on teaching the students how to fish instead of simply giving them fish. As a result, the students’ spirit of independent learning increased. Kholmuratovich et al. (2020) stated in their study that independent learning helps students to learn effectively and efficiently [ 45 ]. It increases their independence and critical thinking skills, while also effectively enhancing their self-esteem and motivation [ 46 ]. For this reason, Lau et al. (2017) recommend promoting this teaching method in their study [ 47 ]. Based on the aforementioned studies, independent and self-directed learning leads to improved comprehension and learning, increased motivation, enhanced self-confidence, and critical thinking among students. Consequently, it can be argued that teaching based on clinical cases and workshop-based approaches, beyond aiding students in better understanding and applying the nursing process, has the potential to transform students’ overall learning approach.
Teaching the nursing process through workshops based on clinical cases has broken the taboo surrounding the application of the nursing process. The organization of these workshops in a friendly and stress-free environment, where real clinical cases were discussed, analyzed, and criticized, motivated the students to apply the nursing process in clinical setting. This approach led to a correction in their perception that they considered the implementation of the nursing process as time-consuming and unnecessary, and it also increased the students’ critical thinking abilities. The nature and process of conducting the workshops proved to be beneficial in implementing the theoretical standards in practical settings. The nursing interventions program was evidence based. This approach not only fostered students’ motivation for self-directed learning but also heightened their curiosity for acquiring knowledge. In these sessions, the approach involved teaching students how to fish rather than simply giving them fish. On the other hand, one of the significant challenges in the application of the nursing process in clinical practice by students is the lack of knowledge and skills among nurses to provide care based on the nursing process, it is recommended that these workshops also be conducted for nurses. Furthermore, action research should be employed to evaluate the role of this educational approach in enhancing the knowledge and skills of clinical nurses.
Limitations
Considering that the workshops had to be held outside of the regular class hours of the faculty, which is at 16:00, and taking into account the transportation issues of the students, the workshops could only continue until 18:00. The limitations of this study include the restricted hours and duration of these workshops. Another limitation of this study is the lack of implementation of nursing interventions by the researchers for the patient and subsequently the real evaluation of the interventions performed, due to ethical considerations. In fact, considering that the biggest problem for students is the application of the nursing process related to assessment, diagnosis, and planning, the focus of the workshops was on these stages. However, it seems that by covering all stages of the nursing process in educational workshops, the challenges faced by students in the implementation and evaluation stages can also be addressed.
Data availability
The data that support the findings of this study are available from the cor - responding author upon reasonable request.
Karimi H. Applying nursing process education in workshop framework. Procedia-Social Behav Sci. 2011;29:561–6. https://doi.org/10.1016/j.sbspro.2011.11.276 .
Article Google Scholar
Mwangi C, Meng’anyi LW, Mbugua RG. Utilization of the nursing process among nurses working at a level 5 hospital, Kenya. Int J Nurs Sci. 2019;9(1):1–11. https://doi.org/10.5923/j.nursing.20190901.01 .
Ghanbari A, Monfared A, Hoseinzadeh T, Moaddab F, Sedighi A. The impact of the nursing process education on critical thinking of nursing students. Res Med Educ. 2017;9(2):33–25.
Google Scholar
Rajabpoor M, Zarifnejad GH, Mohsenizadeh SM, Mazloum SR, Pourghaznein T, Mashmoul A, Mohammad A. Barriers to the implementation of nursing process from the viewpoint of faculty members, nursing managers, nurses, and nursing students. J Holist Nurs Midwifery. 2018;28(2):137–42. https://doi.org/10.29252/hnmj.28.2.137 .
Agyeman-Yeboah J, Korsah KA, Okrah J. Factors that influence the clinical utilization of the nursing process at a hospital in Accra, Ghana. BMC Nurs. 2017;16(30):1–7. https://doi.org/10.1186/s12912-017-0228-0 .
Nes AA, Høybakk J, Zlamal J, Solberg MT. Mixed teaching methods focused on flipped classroom and digital unfolding case to enhance undergraduate nursing students’ knowledge in nursing process. Int J Educational Res. 2021;109:1–9. https://doi.org/10.1016/j.ijer.2021.101859 .
Amouzeshi Z, Mohsenizadeh M, Amouzeshi A. Effect of teaching nursing process using integrated method (Concept map and advance organizer) on nursing students’ clinical learning. Future Med Educ J. 2015;5(1):68–71. https://doi.org/10.22038/FMEJ.2015.4042 .
Hong S, Yu P. Comparison of the effectiveness of two styles of case-based learning implemented in lectures for developing nursing students’ critical thinking ability: a randomized controlled trial. Int J Nurs Stud. 2017;68:16–24. https://doi.org/10.1016/j.ijnurstu.2016.12.008 .
Article PubMed Google Scholar
Forsgren S, Christensen T, Hedemalm A. Evaluation of the case method in nursing education. Nurse Educ Pract. 2014;14(2):164–9. https://doi.org/10.1016/j.nepr.2013.08.003 .
Kestel S, Korkmaz F. Effectiveness of blended learning in nursing process teaching: first-year nursing students. Teach Learn Nurs. 2023;18(4):212–9. https://doi.org/10.1016/j.teln.2023.07.005 .
Keshk LI, Qalawa SAA, Ibrahim NM. Effectiveness of an educational program regarding nursing process on acquiring advanced skills among internship nursing students. Int J Nurs Educ. 2018;5(2):32–44. https://doi.org/10.15640/ijn.v5n2a4 .
Gholami M, Saki M, Toulabi T, Moghadam PK, Pour AHH, Dostizadeh R. Iranian nursing students’ experiences of case-based learning: A qualitative study. J Prof Nurs 2017, 33(3):241–9. https://doi.org/10.1016/j.profnurs.2016.08.013
Raurell-Torredà M, Olivet‐Pujol J, Romero‐Collado À, Malagon‐Aguilera MC, Patiño‐Masó J, Baltasar‐Bagué A. Case‐based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47(1):34–42. https://doi.org/10.1111/jnu.12113 .
Majid U, Vanstone M. Appraising qualitative research for evidence syntheses: a compendium of quality appraisal tools. Qual Health Res. 2018;28(13):2115–31. https://doi.org/10.1177/1049732318785358 .
Bradshaw C, Atkinson S, Doody O. Employing a qualitative description approach in health care research. Global Qualitative Nurs Res. 2017;4:1–8. https://doi.org/10.1177/2333393617742282 .
Krippendorff K. Content analysis: an introduction to its methodology. Sage; 2018.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. https://doi.org/10.1111/j.1365-2648.2007.04569.x .
Hanisch M, Kroeger E, Dekiff M, Timme M, Kleinheinz J, Dirksen D. 3D-printed surgical training model based on real patient situations for dental education. Int J Environ Res Public Health. 2020;17(8):1–11. https://doi.org/10.3390/ijerph17082901 .
Article CAS Google Scholar
Yilmaz FT, Sabanciogullari S, Aldemir K. The opinions of nursing students regarding the nursing process and their levels of proficiency in Turkey. J Caring Sci. 2015;4(4):265.
Thuvaraka S, Vijayanathan S, Pakeerathy M, Subathra R, Laavanya M, Priyanthi W. Challenges faced by nurses in implementation of nursing process in special units at Teaching Hospital. Jaffna. 2018;3(1):61–4.
Mert S, Altuntaş Yildiz T, Gönen Şentürk S, Durualp E. Senior high school students’ opinions on the nursing profession: A ten-year comparative study. J Adv Nurs 2020, 76(8):2082–93. https://doi.org/10.1111/jan.14403
Zamanzadeh V, Valizadeh L, Tabrizi FJ, Behshid M, Lotfi M. Challenges associated with the implementation of the nursing process: a systematic review. Iran J Nurs Midwifery Res. 2015;20(4):411–9. https://doi.org/10.4103/1735-9066.161002 .
Article PubMed PubMed Central Google Scholar
Sharghi NR, Alami A, Khosravan S, Mansoorian MR, Ekrami A. Academic training and clinical placement problems to achieve nursing competency. J Adv Med Educ Professionalism. 2015;3(1):15–20.
Carvalho DP, Azevedo IC, Cruz GK, Mafra GA, Rego AL, Vitor AF, Santos VE, Cogo AL, Júnior MAF. Strategies used for the promotion of critical thinking in nursing undergraduate education: a systematic review. Nurse Educ Today. 2017;57:103–7. https://doi.org/10.1016/j.nedt.2017.07.010 .
Rahmani M, Alijani H, Dashtbozorge B, Haghighizadeh MH. Effect of the nursing process using via. J Clin Nurs Midwifery. 2016;5(2):75–83.
Heidari H, Mardani Hamooleh M. Nursing students’ experiences regarding nursing process: a qualitative study. Res Dev Med Educ. 2016;5(2):101–4. https://doi.org/10.15171/rdme.2016.021 .
Mackey A, Bassendowski S. The history of evidence-based practice in nursing education and practice. J Prof Nurs. 2017;33(1):51–5. https://doi.org/10.1016/j.profnurs.2016.05.009 .
Sin M-K, Bliquez R. Teaching evidence based practice to undergraduate nursing students. J Prof Nurs. 2017;33(6):447–51. https://doi.org/10.1016/j.profnurs.2017.06.003 .
Adraro Z. A Cherkos 2021 Knowledge and attitude of nurses about the nursing process in selected public hospitals in South-West Ethiopia. Adv Nurs Midwifery 30 1 34–41 https://doi.org/10.22037/jnm.v30i1.34285 .
Nakhaee S, Nasiri A. Inter-professional relationships issues among Iranian nurses and physicians: a qualitative study. Iran J Nurs Midwifery Res. 2017;22(1):8–13.
Adamy EK, Zocche DAA, Almeida MA. Contribution of the nursing process for the construction of the identity of nursing professionals. Revista Gaúcha De Enfermagem. 2019;41:1–8. https://doi.org/10.1590/1983-1447.2020.20190143 .
Hackett J. The importance of holistic care at the end of life. Ulster Med J. 2017;86(2):143–4.
PubMed PubMed Central Google Scholar
Dyrstad DN, Bodsberg KG, Søiland M, Bergesen ÅU, Urstad KH. Value of simulating holistic nursing care: a quantitative study. Clin Simul Nurs. 2021;54:113–20. https://doi.org/10.1016/j.ecns.2021.02.002 .
Hajbaghery MA, Mokhtari R. Complementary and alternative medicine and holistic nursing care: the necessity for curriculum revision. J Complement Med. 2018;5(4):1–2.
Jasemi M, Valizadeh L, Zamanzadeh V, Keogh B. A concept analysis of holistic care by hybrid model. Indian J Palliat Care. 2017;23(1):71–80. https://doi.org/10.4103/0973-1075.197960 .
Zamanzadeh V, Jasemi M, Valizadeh L, Keogh B, Taleghani F. Effective factors in providing holistic care: a qualitative study. Indian J Palliat Care. 2015;21(2):214–24. https://doi.org/10.4103/0973-1075.156506 .
Korkut S, Sahin S, Ulker T, Cidem A. Nursing students’ views of the nursing process and its challenges, and their solutions: a qualitative study. Int J Caring Sci. 2021;14(2):811–24.
Browne C, Wall P, Batt S, Bennett R. Understanding perceptions of nursing professional identity in students entering an Australian undergraduate nursing degree. Nurse Educ Pract. 2018;32:90–6. https://doi.org/10.1016/j.nepr.2018.07.006 .
Article CAS PubMed Google Scholar
Baraz PS, Memarian R, Vanaki Z. Damaged professional identity as a barrier to Iranian nursing students’clinical learning: a qualitative study 2014,3(3):1–15.
Hood K, Cant R, Baulch J, Gilbee A, Leech M, Anderson A, Davies K. Prior experience of interprofessional learning enhances undergraduate nursing and healthcare students’ professional identity and attitudes to teamwork. Nurse Educ Pract. 2014;14(2):117–22. https://doi.org/10.1016/j.nepr.2013.07.013 .
Sabanciogullari S, Dogan S. Relationship between job satisfaction, professional identity and intention to leave the profession among nurses in Turkey. J Nurs Adm Manag. 2015;23(8):1076–85. https://doi.org/10.1111/jonm.12256 .
Sun L, Gao Y, Yang J, Zang X-Y, Wang Y-G. The impact of professional identity on role stress in nursing students: a cross-sectional study. Int J Nurs Stud. 2016;63:1–8. https://doi.org/10.1016/j.ijnurstu.2016.08.010 .
Van der Cingel M, Brouwer J. What makes a nurse today? A debate on the nursing professional identity and its need for change. Nurs Philos. 2021;22(2):1–7. https://doi.org/10.1111/nup.12343 .
Haghighat S, Borhani F, Ranjbar H, Naseri P. Evaluating the formation of professional identity in Iranian nursing students after implementation of a new curriculum. J Nurs Midwifery Sci. 2019;6(3):138–43. https://doi.org/10.4103/2345-5756.231386 .
Kholmuratovich MK, Mardanqulovich A, Ravshanovich JR, Sharifovna KU, Shodiyevna BO. Methodology of improving independent learning skills of future fine art teachers (on the example of still life in colorful paintings). Int J Psychosocial Rehabilitation. 2020;24(05):285–8. https://doi.org/10.37200/IJPR/V24I5/PR201880 .
Shah UV, Chen W, Inguva P, Chadha D, Brechtelsbauer C. The discovery laboratory part II: a framework for incubating independent learning. Educ Chem Eng. 2020;31:29–37. https://doi.org/10.1016/j.ece.2020.03.003 .
Lau K. The most important thing is to learn the way to learn’: evaluating the effectiveness of independent learning by perceptual changes. Assess Evaluation High Educ. 2017;42(3):415–30. https://doi.org/10.1080/02602938.2015.1118434 .
Download references
Acknowledgements
The researchers would like to express their gratitude to the students and professors who participated in the workshops and Student Research Committee of Isfahan University of Medical Sciences.
This study was financed by the Student Vice Chancellor for Research of Isfahan University of Medical Sciences (Project number 1400254).
Author information
Authors and affiliations.
Pediatric Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran
Amir Shahzeydi
Student of Research Committee, School of Nursing and Midwifery, University of Medical Sciences, Isfahan, Iran
Nursing and Midwifery Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Parvaneh Abazari
Nursing and Midwifery Sciences Development Research Center, Najaf abad Branch, Islamic Azad University, Najaf abad, Iran
Faculty of Nursing and Midwifery, Qom University of Medical Sciences, Qom, Iran
Fatemeh Gorji-varnosfaderani
Nursing and Midwifery Care Research Center, Department of Adult Health Nursing, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
Elaheh Ashouri, Shahla Abolhassani & Fakhri Sabohi
You can also search for this author in PubMed Google Scholar
Contributions
ASH, PA, FG designed the study. ASH, PA, FG, EA, SHA, FS helded the Workshops. PA interviewed the participants. ASH and FG wrote the interviews. PA, EA and SHA analyzed the interviews. ASH, PA and FS prepared the manuscript, and all authors read and approved the final manuscript.
Corresponding author
Correspondence to Parvaneh Abazari .
Ethics declarations
Ethics approval and consent to participate.
This study has been approved by the ethics committee of Isfahan University of Medical Sciences (IR.MUI.NUREMA.REC.1400.139) in 2021. Initially, the research purpose was explained to the patients and their caregivers. They were informed that participation in the research is entirely voluntary and free of charge. Not participating in the research would not affect their care and treatment interventions. They were assured that they could withdraw from the research at any time. Furthermore, it was emphasized that their information would be presented in the workshop in a strictly confidential manner, without disclosing their names, photos, file numbers, etc. Subsequently, both oral and written consent were obtained from them. After that, the study’s purpose was also explained to nursing students and faculty members, and informed oral and written consent was obtained from them. Numeric codes were used instead of personal names to ensure the confidentiality of the interviews. The participants were free to withdraw from the study at any time. All methods were conducted following the applicable guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Shahzeydi, A., Abazari, P., Gorji-varnosfaderani, F. et al. Breaking the taboo of using the nursing process: lived experiences of nursing students and faculty members. BMC Nurs 23 , 621 (2024). https://doi.org/10.1186/s12912-024-02233-z
Download citation
Received : 05 February 2024
Accepted : 06 August 2024
Published : 05 September 2024
DOI : https://doi.org/10.1186/s12912-024-02233-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing students
- Nursing process
- Clinical case
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Breaking the taboo of using the nursing process: lived experiences of nursing students and faculty members
Affiliations.
- 1 Pediatric Cardiovascular Research Center, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan, Iran.
- 2 Student of Research Committee, School of Nursing and Midwifery, University of Medical Sciences, Isfahan, Iran.
- 3 Nursing and Midwifery Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran. [email protected].
- 4 Nursing and Midwifery Sciences Development Research Center, Najaf abad Branch, Islamic Azad University, Najaf abad, Iran. [email protected].
- 5 Faculty of Nursing and Midwifery, Qom University of Medical Sciences, Qom, Iran.
- 6 Nursing and Midwifery Care Research Center, Department of Adult Health Nursing, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
- PMID: 39237916
- PMCID: PMC11378630
- DOI: 10.1186/s12912-024-02233-z
Background: Despite the numerous advantages of the nursing process, nursing students often struggle with utilizing this model. Therefore, studies suggest innovative teaching methods to address this issue. Teaching based on real clinical cases is considered a collaborative learning method that enhances students' active learning for the development of critical thinking and problem-solving skills. In this method, students can acquire sufficient knowledge about patient care by accessing authentic information.
Objective: The aim of the present study was to investigate the experiences of nursing students and faculty members regarding the implementation of nursing process educational workshops, based on real case studies.
Design: A qualitative descriptive study.
Participants: 9 Nursing students and 7 faculty members from the Isfahan School of Nursing and Midwifery who attended the workshops.
Methods: This qualitative descriptive study was conducted from 2021 to 2023. Data was collected through semi-structured individual and focus group interviews using a qualitative content analysis approach for data analysis.
Results: After analyzing the data, a theme titled "Breaking Taboos in the Nursing Process" was identified. This theme consists of four categories: "Strengthening the Cognitive Infrastructure for Accepting the Nursing Process," "Enhancing the Applicability of the Nursing Process," "Assisting in Positive Professional Identity," and "Facilitating a Self-Directed Learning Platform." Additionally, thirteen subcategories were obtained.
Conclusion: The data obtained from the present study showed that conducting nursing process educational workshops, where real clinical cases are discussed, analyzed, and criticized, increases critical thinking, learning motivation, and understanding of the necessity and importance of implementing the nursing process. Therefore, it is recommended that instructors utilize this innovative and effective teaching method for instructing the nursing process.
Keywords: Clinical case; Education; Nursing process; Nursing students; Workshop.
© 2024. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
- Karimi H. Applying nursing process education in workshop framework. Procedia-Social Behav Sci. 2011;29:561–6. 10.1016/j.sbspro.2011.11.276.10.1016/j.sbspro.2011.11.276 - DOI
- Mwangi C, Meng’anyi LW, Mbugua RG. Utilization of the nursing process among nurses working at a level 5 hospital, Kenya. Int J Nurs Sci. 2019;9(1):1–11. 10.5923/j.nursing.20190901.01.10.5923/j.nursing.20190901.01 - DOI
- Ghanbari A, Monfared A, Hoseinzadeh T, Moaddab F, Sedighi A. The impact of the nursing process education on critical thinking of nursing students. Res Med Educ. 2017;9(2):33–25.
- Rajabpoor M, Zarifnejad GH, Mohsenizadeh SM, Mazloum SR, Pourghaznein T, Mashmoul A, Mohammad A. Barriers to the implementation of nursing process from the viewpoint of faculty members, nursing managers, nurses, and nursing students. J Holist Nurs Midwifery. 2018;28(2):137–42. 10.29252/hnmj.28.2.137.10.29252/hnmj.28.2.137 - DOI
- Agyeman-Yeboah J, Korsah KA, Okrah J. Factors that influence the clinical utilization of the nursing process at a hospital in Accra, Ghana. BMC Nurs. 2017;16(30):1–7. 10.1186/s12912-017-0228-0. 10.1186/s12912-017-0228-0 - DOI - PMC - PubMed
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 02 September 2024
Clinician perspectives and recommendations regarding design of clinical prediction models for deteriorating patients in acute care
- Robin Blythe ORCID: orcid.org/0000-0002-3643-4332 1 ,
- Sundresan Naicker ORCID: orcid.org/0000-0002-2392-4981 1 ,
- Nicole White ORCID: orcid.org/0000-0002-9292-0773 1 ,
- Raelene Donovan ORCID: orcid.org/0000-0003-0737-7719 2 ,
- Ian A. Scott ORCID: orcid.org/0000-0002-7596-0837 3 , 4 ,
- Andrew McKelliget 2 &
- Steven M McPhail ORCID: orcid.org/0000-0002-1463-662X 1 , 4
BMC Medical Informatics and Decision Making volume 24 , Article number: 241 ( 2024 ) Cite this article
Metrics details
Successful deployment of clinical prediction models for clinical deterioration relates not only to predictive performance but to integration into the decision making process. Models may demonstrate good discrimination and calibration, but fail to match the needs of practising acute care clinicians who receive, interpret, and act upon model outputs or alerts. We sought to understand how prediction models for clinical deterioration, also known as early warning scores (EWS), influence the decision-making of clinicians who regularly use them and elicit their perspectives on model design to guide future deterioration model development and implementation.
Nurses and doctors who regularly receive or respond to EWS alerts in two digital metropolitan hospitals were interviewed for up to one hour between February 2022 and March 2023 using semi-structured formats. We grouped interview data into sub-themes and then into general themes using reflexive thematic analysis. Themes were then mapped to a model of clinical decision making using deductive framework mapping to develop a set of practical recommendations for future deterioration model development and deployment.
Fifteen nurses ( n = 8) and doctors ( n = 7) were interviewed for a mean duration of 42 min. Participants emphasised the importance of using predictive tools for supporting rather than supplanting critical thinking, avoiding over-protocolising care, incorporating important contextual information and focusing on how clinicians generate, test, and select diagnostic hypotheses when managing deteriorating patients. These themes were incorporated into a conceptual model which informed recommendations that clinical deterioration prediction models demonstrate transparency and interactivity, generate outputs tailored to the tasks and responsibilities of end-users, avoid priming clinicians with potential diagnoses before patients were physically assessed, and support the process of deciding upon subsequent management.
Conclusions
Prediction models for deteriorating inpatients may be more impactful if they are designed in accordance with the decision-making processes of acute care clinicians. Models should produce actionable outputs that assist with, rather than supplant, critical thinking.
• This article explored decision-making processes of clinicians using a clinical prediction model for deteriorating patients, also known as an early warning score.
• Our study identified that the clinical utility of deterioration models may lie in their assistance in generating, evaluating, and selecting diagnostic hypotheses, an important part of clinical decision making that is underrepresented in the prediction modelling literature.
• Nurses in particular stressed the need for models that encourage critical thinking and further investigation rather than prescribe strict care protocols.
Peer Review reports
The number of ‘clinical prediction model’ articles published on PubMed has grown rapidly over the past two decades, from 1,918 articles identified with these search terms published in 2002 to 26,326 published in 2022. A clinical prediction model is defined as any multivariable model that provides patient-level estimates of the probability or risk of a disease, condition or future event [ 1 , 2 , 3 ].
Recent systematic and scoping reviews report a lack of evidence that clinical decision support systems based on prediction models are associated with improved patient outcomes once implemented in acute care [ 4 , 5 , 6 , 7 ]. One potential reason may be that some models are not superior to clinical judgment in reducing missed diagnoses or correctly classifying non-diseased patients [ 8 ]. While improving predictive accuracy is important, this appears insufficient for improving patient outcomes, suggesting that more attention should be paid to the process and justification of how prediction models are designed and deployed [ 9 , 10 ].
If model predictions are to influence clinical decision-making, they must not only demonstrate acceptable accuracy, but also be implemented and adopted at scale in clinical settings. This requires consideration of how they are integrated into clinical workflows, how they generate value for users, and how clinicians perceive and respond to their outputs of predicted risks [ 11 , 12 ]. These concepts are tenets of user-centred design, which focuses on building systems based on the needs and responsibilities of those who will use them. User-centred decision support tools can be designed in a variety of ways, but may benefit from understanding the characteristics of the users and the local environment in which tools are implemented, [ 13 ] the nature of the tasks end-users are expected to perform, [ 14 ] and the interface between the user and the tools [ 15 ].
Prediction models for clinical deterioration
A common task for prediction models integrated into clinical decision support systems is in predicting or recognising clinical deterioration, also known as early warning scores. Clinical deterioration is defined as the transition of a patient from their current health state to a worse one that puts them at greater risk of adverse events and death [ 16 ]. Early warning scores were initially designed to get the attention of skilled clinicians when patients began to deteriorate, but have since morphed into complex multivariable prediction models [ 17 ]. As with many other clinical prediction models, early warning scores often fail to demonstrate better patient outcomes once deployed [ 4 , 18 ]. The clinical utility of early warning scores likely rests on two key contextual elements: the presence of uncertainty, both in terms of diagnosis and prognosis, and the potential for undesirable patient outcomes if an appropriate care pathway is delayed or an inappropriate one is chosen [ 19 ].
The overarching goal of this qualitative study was to determine how prediction models for clinical deterioration, or early warning scores, could be better tailored to the needs of end-users to improve inpatient care. This study had three aims. First, to understand the experiences and perspectives of nurses and doctors who use early warning scores. Second, to identify the tasks these clinicians performed when managing deteriorating patients, the decision-making processes that guided these tasks, and how these could be conceptualised schematically. Finally, to address these tasks and needs with actionable, practical recommendations for enhancing future deterioration prediction model development and deployment.
To achieve our study aims, we conducted semi-structured interviews of nurses and doctors at two large, digitally mature hospitals. We first asked clinicians to describe their backgrounds, perspectives, and experience with early warning scores to give context to our analysis. We then examined the tasks and responsibilities of participants and the decision-making processes that guided these tasks using reflexive thematic analysis, an inductive method that facilitated the identification of general themes. We then identified a conceptual decision-making framework from the literature to which we mapped these themes to understand how they may lead to better decision support tools. Finally, we used this framework to formulate recommendations for deterioration prediction model design and deployment. These steps are presented graphically in a flow diagram (Fig. 1 ).
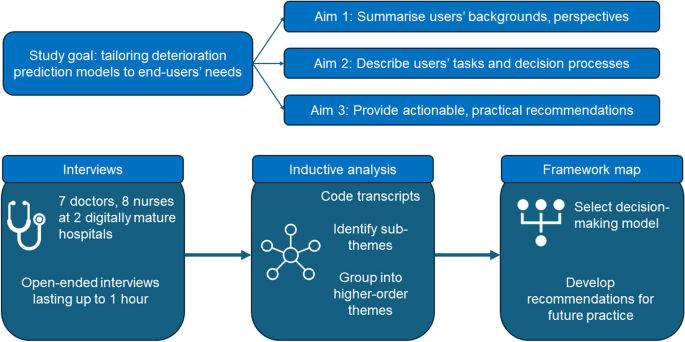
Schema of study goal, aims and methods
The study was conducted at one large tertiary and one medium-sized metropolitan hospital in Brisbane, Australia. The large hospital contained over 1,000 beds, handling over 116,000 admissions and approximately 150,000 deterioration alerts per year in 2019. Over the same period, the medium hospital contained 175 beds, handling over 31,000 admissions and approximately 42,000 deterioration alerts per year. These facilities had a high level of digital maturity, including fully integrated electronic medical records.
Clinical prediction model for deteriorating patients
The deterioration monitoring system used at both hospitals was the Queensland Adult Deterioration Detection System (Q-ADDS) [ 20 , 21 ]. Q-ADDS uses an underlying prediction model to convert patient-level vital signs from a single time of observation into an ordinal risk score describing an adult patient’s risk of acute deterioration. Vital signs collected are respiratory rate (breaths/minute), oxygen flow rate (L/minute), arterial oxygen saturation (percent), blood pressure (mmHg), heart rate (beats/minute), temperature (degrees Celsius), level of consciousness (Alert-Voice-Pain-Unresponsive) and increased or new onset agitation. Increased pain and urine output are collected but not used for score calculation [ 21 ]. The Q-ADDS tool is included in the supplementary material.
Vital signs are entered into the patient’s electronic medical record, either imported from the vital signs monitoring device at the patient’s bedside or from manual entry by nurses. Calculations are made automatically within Q-ADDS to generate an ordinal risk score per patient observation. Scores can be elevated to levels requiring a tiered escalation response if a single vital sign is greatly deranged, or if several observations are deranged by varying degrees. Scores range from 0 to 8+, with automated alerts and escalation protocols ranging from more frequent observations for lower scores to immediate activation of the medical emergency team (MET) at higher scores.
The escalation process for Q-ADDS is highly structured, mandated and well documented [ 21 ]. Briefly, when a patient’s vital signs meet a required alert threshold, the patient’s nurse is required to physically assess the patient and, depending on the level of severity predicted by Q-ADDS, notify the patient’s doctor (escalation). The doctor is then required to be notified of the patient’s Q-ADDS score, potentially review the patient, and discuss any potential changes to care with the nurse. Both nurses and doctors can escalate straight to MET calls or an emergency ‘code blue’ call (requiring cardiopulmonary resuscitation or assisted ventilation) at any time if necessary.
Participant recruitment
Participant recruitment began in February 2022 and concluded in March 2023, disrupted by the COVID-19 pandemic. Eligibility criteria were nurses or doctors at each hospital with direct patient contact who either receive or respond, respectively, to Q-ADDS alerts. An anticipated target sample size of 15 participants was established prior to recruitment, based on expected constraints in recruitment due to clinician workloads and the expected length of interviews relative to their scope, as guided by prior research [ 22 ]. As the analysis plan involved coding interviews iteratively as they were conducted, the main justification for ceasing recruitment was when no new themes relating to the study objectives were generated during successive interviews as the target sample size was approached [ 23 ].
Study information was broadly distributed via email to nurses and doctors in patient-facing roles across hospitals. Nurse unit managers were followed up during regular nursing committee meetings to participate or assist with recruitment within their assigned wards. Doctors were followed up by face-to-face rounding. Snowball sampling, in which participants were encouraged to refer their colleagues for study participation, was employed whenever possible. In all cases, study authors explained study goals and distributed participant consent forms prior to interview scheduling with the explicit proviso that participation was completely voluntary and anonymous to all but two study authors (RB and SN).
Interview process
We used a reflexive framework method to develop an open-ended interview template [ 24 ] that aligned with our study aims. Interview questions were informed by the non-adoption, abandonment, scale-up, spread and sustainability (NASSS) framework [ 25 ]. The NASSS framework relates the end-user perceptions of the technology being evaluated to its value proposition for the clinical situation to which it is being applied. We selected a reflexive method based on the NASSS for our study as we wanted to allow end-users to speak freely about the barriers they faced when using prediction models for clinical deterioration, but did not limit participants to discussing only topics that could fit within the NASSS framework.
Participants were first asked about their background and clinical expertise. They were then invited to share their experiences and perspectives with using early warning scores to manage deteriorating patients. This was used as a segue for participants to describe the primary tasks required of them when evaluating and treating a deteriorating patient. Participants were encouraged to talk through their decision-making process when fulfilling these tasks, and to identify any barriers or obstacles to achieving those tasks that were related to prediction models for deteriorating patients. Participants were specifically encouraged to identify any sources of information that were useful for managing deteriorating patients, including prediction models for other, related disease groups like sepsis, and to think of any barriers or facilitators for making that information more accessible. Finally, participants were invited to suggest ways to improve early warning scores, and how those changes may lead to benefits for patients and clinicians.
As we employed a reflexive methodology to allow clinicians to speak freely about their perspectives and opinions, answers to interview questions were optional and open-ended, allowing participants to discuss relevant tangents. Separate interview guides were developed for nurses and doctors as the responsibilities and information needs of these two disciplines in managing deteriorating patients often differ. Nurses are generally charged with receiving and passing on deterioration alerts, while doctors are generally charged with responding to alerts and making any required changes to patient care plans [ 4 ]. Interview guides are contained in the supplement.
Due to clinician workloads, member checking, a form of post-interview validation in which participants retrospectively confirm their interview answers, was not used. To ensure participants perceived the interviewers as being impartial, two study authors not employed by the hospital network and not involved in direct patient care (RB and SN) were solely responsible for conducting interviews and interrogating interview transcripts. Interviews were recorded and transcribed verbatim, then re-checked for accuracy.
Inductive thematic analysis
Transcripts were analysed using a reflexive thematic methodology informed by Braun and Clarke [ 26 ]. This method was selected because it facilitated exploring the research objectives rather than being restricted to the domains of a specific technology adoption framework, which may limit generalisability [ 27 ]. Interviews were analysed over five steps to identify emergent themes.
Each interview was broken down into segments by RB and SN, where segments corresponded to a distinct opinion.
Whenever appropriate, representative quotes for each distinct concept were extracted.
Segments were grouped into sub-themes.
Sub-themes were grouped into higher-order themes, or general concepts.
Steps 1 through 4 were iteratively repeated by RB and supervised by SN.
As reflexive methods incorporate the experiences and expertise of the analysts, our goal was to extract any sub-themes relevant to the study aims and able to be analysed in the context of early warning scores, prediction models, or decision support tools for clinical deterioration. The concepts explored during this process were not exhaustive, but repeated analysis and re-analysis of participant transcripts helped to ensure all themes could be interpreted in the context of our three study aims: background and perspectives, tasks and decision-making, and recommendations for future practice.
Deductive mapping to a clinical decision-making framework
Once the emergent themes from the inductive analysis were defined, we conducted a brief scan of PubMed for English-language studies that investigated how the design of clinical decision support systems relate to clinical decision-making frameworks. The purpose of this exercise was to identify a framework against which we could map the previously elicited contexts, tasks, and decision-making of end-users in developing a decision-making model that could then be used to support the third aim of formulating recommendations to enhance prediction model development and deployment.
RB and SN then mapped higher-order themes from the inductive analysis to the decision-making model based on whether there was a clear relationship between each theme and a node in the model (see Results).
Recommendations for improving prediction model design were derived by reformatting the inductive themes based on the stated preferences of the participants. These recommendations were then assessed by the remaining authors and the process repeated iteratively until authors were confident that all recommendations were concordant with the decision-making model.
Participant characteristics
Our sample included 8 nurses and 7 doctors of varying levels of expertise and clinical specialties; further information is contained in the supplement. Compared to doctors, nurse participants were generally more experienced, often participating in training or mentoring less experienced staff. Clinical specialities of nurses were diverse, including orthopaedics, cancer services, medical assessment and planning unit, general medicine, and pain management services. Doctor participants ranged from interns with less than a year of clinical experience up to consultant level, including three doctors doing training rotations and two surgical registrars. Clinical specialties of doctors included geriatric medicine, colorectal surgery, and medical education.
Interviews and thematic analysis
Eleven interviews were conducted jointly by RB and SN, one conducted by RB, and three by SN. Interviews were scheduled for up to one hour, with a mean duration of 42 min. Six higher-order themes were identified. These were: added value of more information; communication of model outputs; validation of clinical intuition; capability for objective measurement; over-protocolisation of care; and model transparency and interactivity (Table 1 ). Some aspects of care, including the need for critical thinking and the informational value of discerning trends in patient observations, were discussed in several contexts, making them relevant to more than one higher-order theme.
Added value of other information
Clinicians identified that additional data or variables important for decision making were often omitted from the Q-ADDS digital interface. Such variables included current medical conditions, prescribed medications and prior observations, which were important for interpreting current patient data in the context of their baseline observations under normal circumstances (e.g., habitually low arterial oxygen saturation due to chronic obstructive pulmonary disease) or in response to an acute stimulus (e.g., expected hypotension for next 4 to 8 h while treatment for septic shock is underway).
“The trend is the biggest thing [when] looking at the data , because sometimes people’s observations are deranged forever and it’s not abnormal for them to be tachycardic , whereas for someone else , if it’s new and acute , then that’s a worry.” – Registrar.
Participants frequently emphasised the critical importance of looking at patients holistically, or that patients were more than the sum of the variables used to predict risk. Senior nurses stressed that prediction models were only one part of patient evaluation, and clinicians should be encouraged to incorporate both model outputs and their own knowledge and experiences in decision making rather than trust models implicitly. Doctors also emphasised this holistic approach, adding that they placed more importance on hearing a nurse was concerned for the patient than seeing the model output. Critical thinking about future management was frequently raised in this context, with both nurses and doctors insisting that model predictions and the information required for contextualising risk scores should be communicated together when escalating the patient’s care to more senior clinicians.
Model outputs
Model outputs were discussed in two contexts. First, doctors perceived that ordinal risk scores generated by Q-ADDS felt arbitrary compared to receiving probabilities of a future event, for example cardiorespiratory decompensation, that required a response such as resuscitation or high-level treatment. However, nurses did not wholly embrace probabilities as outputs, instead suggesting that recommendations for how they should respond to different Q-ADDS scores were more important. This difference may reflect the different roles of alert receivers (nurses) and alert responders (doctors).
“[It’s helpful] if you use probabilities… If your patient has a sedation score of 2 and a respiratory rate of 10 , [giving them] a probability of respiratory depression would be helpful. However , I don’t find many clinicians , and certainly beginning practitioners , think in terms of probabilities.” – Clinical nurse consultant.
Second, there was frequent mention of alert fatigue in the context of model outputs. One doctor and two nurses felt there was insufficient leeway for nurses to exercise discretion in responding to risk scores, leading to many unnecessary alert-initiated actions. More nuance in the way Q-ADDS outputs were delivered to clinicians with different roles was deemed important to avoid model alerts being perceived as repetitive and unwarranted. However, three other doctors warned against altering MET call criteria in response to repetitive and seemingly unchanging risk scores and that at-risk patients should, as a standard of care, remain under frequent observation. Frustrations centred more often around rigidly tying repetitive Q-ADDS outputs to certain mandated actions, leading to multiple clinical reviews in a row for a patient whose trajectory was predictable, for example a patient with stable heart failure having a constantly low blood pressure. This led to duplication of nursing effort (e.g., repeatedly checking the blood pressure) and the perception that prediction models were overly sensitive.
“It takes away a lot of nurses’ critical judgement. If someone’s baseline systolic [blood pressure] is 95 [mmHg] , they’re asymptomatic and I would never hear about it previously. We’re all aware that this is where they sit and that’s fine. Now they are required to notify me in the middle of the night , “Just so you know , they’ve dropped to 89 [below an alert threshold of 90mmHg].“” – Junior doctor.
Validation of clinical intuition
Clinicians identified the ability of prediction models to validate their clinical intuition as both a benefit and a hindrance, depending on how outputs were interpreted and acted upon. Junior clinicians appreciated early warning scores giving them more support to escalate care to senior clinicians, as a conversation starter or framing a request for discussion. Clinicians described how assessing the patient holistically first, then obtaining model outputs to add context and validate their diagnostic hypotheses, was very useful in deciding what care should be initiated and when.
“You kind of rule [hypotheses] out… you go to the worst extreme: is it something you need to really be concerned about , especially if their [score] is quite high? You’re thinking of common complications like blood clots , so that presents as tachycardic… I’m thinking of a PE [pulmonary embolism] , then you do the nursing interventions.” – Clinical nurse manager.
While deterioration alerts were often seen as triggers to think about potential causes for deterioration, participants noted that decision making could be compromised if clinicians were primed by model outputs to think of different diagnoses before they had fully assessed the patient at the bedside. Clinicians described the dangers of tunnel vision or, before considering all available clinical information, investigating favoured diagnoses to the exclusion of more likely causes.
“[Diagnosis-specific warnings are] great , [but] that’s one of those things that can lead to a bit of confirmation bias… It’s a good trigger to articulate , “I need to look for sources of infection when I go to escalate"… but then , people can get a little bit sidetracked with that and ignore something more blatant in front of them. I’ve seen people go down this rabbit warren of being obsessed with the “fact” that it was sepsis , but it was something very , very unrelated.” – Nurse educator.
Objective measurement
Clinicians perceived that prediction models were useful as more objective measures of patients’ clinical status that could ameliorate clinical uncertainty or mitigate cognitive biases. In contrast to the risk of confirmation bias arising from front-loading model outputs suggesting specific diagnoses, prediction models could offer a second opinion that could help clinicians recognise opposing signals in noisy data that, in particular, assisted in considering serious diagnoses that shouldn’t be missed (e.g., sepsis), or more frequent and easily treated diagnoses (e.g., dehydration). Prediction models were also useful when they disclosed several small, early changes in patient status that provided an opportunity for early intervention.
“Maybe [the patient has] a low grade fever , they’re a bit tachycardic. Maybe [sepsis] isn’t completely out of the blue for this person. If there was some sort of tool , that said there’s a reasonable chance that they could have sepsis here , I would use that to justify the option of going for blood cultures and maybe a full septic screen. If [I’m indecisive] , that sort of information could certainly push me in that direction.” – Junior doctor.
Clinicians frequently mentioned that prediction models would have been more useful when first starting clinical practice, but become less useful with experience. However, clinicians noted that at any experience level, risk scoring was considered most useful as a triage/prioritisation tool, helping decide which patients to see first, or which clinical concerns to address first.
“[Doctors] can easily triage a patient who’s scoring 4 to 5 versus 1 to 3. If they’re swamped , they can change the escalation process , or triage appropriately with better communication.” – Clinical nurse manager.
Clinicians also stressed that predictions were not necessarily accurate because measurement error or random variation, especially one-off outlier values for certain variables, was a significant contributor to false alerts and inappropriate responses. For example, a single unusually high respiratory rate generated an unusually high risk score, prompting an unnecessary alert.
Over-protocolisation of care
The sentiment most commonly expressed by all experienced nursing participants and some doctors was that nurses were increasingly being trained to solely react to model outputs with fixed response protocols, rather than think critically about what is happening to patients and why. It was perceived that prediction models may actually reduce the capacity for clinicians to process and internalise important information. For example, several nurses observed their staff failing to act on their own clinical suspicions that patients were deteriorating because the risk score had not exceeded a response threshold.
“We’ve had patients on the ward that have had quite a high tachycardia , but it’s not triggering because it’s below the threshold to trigger… [I often need to make my staff] make the clinical decision that they can call the MET anyway , because they have clinical concern with the patient.” – Clinical nurse consultant.
A source of great frustration for many nurses was the lack of critical thinking by their colleagues of possible causes when assessing deteriorating patients. They wanted their staff to investigate whether early warning score outputs or other changes in patient status were caused by simple, easily fixable issues such as fitting the oxygen mask properly and helping the patient sit up to breathe more easily, or whether they indicated more serious underlying pathophysiology. Nurses repeatedly referenced the need for clinicians to always be asking why something was happening, not simply reacting to what was happening.
“[Models should also be] trying to get back to critical thinking. What I’m seeing doesn’t add up with the monitor , so I should investigate further than just simply calling the code.” – Clinical nurse educator.
Model transparency and interactivity
Clinicians frequently requested more transparent and interactive prediction models. These included a desire to receive more training in how prediction models worked and how risk estimates were generated mathematically, and being able to visualise important predictors of deterioration and the absolute magnitude of their effects (effect sizes) in intuitive ways. For example, despite receiving training in Q-ADDS, nurses expressed frustrations that nobody at the hospital seemed to understand how it worked in generating risk scores. Doctors were interested in being able to visualise the relative size and direction of effect of different model variables, potentially using colour-coding, combined with other contextual patient data like current vital sign trends and medications, and presented on one single screen.
The ability to modify threshold values for model variables and see how this impacted risk scores, and what this may then mean for altering MET calling criteria, was also discussed. For example, in an older patient with an acute ischaemic stroke, a persistently high, asymptomatic blood pressure value is an expected bodily response to this acute insult over the first 24–48 h. In the absence of any change to alert criteria, recurrent alerts would be triggered which may encourage overtreatment and precipitous lowering of the blood pressure with potential to cause harm. Altering the criteria to an acceptable or “normal” value for this clinical scenario (i.e. a higher than normal blood pressure) may generate a lower, more patient-centred risk estimate and less propensity to overtreat. This ability to tinker with the model may also enhance understanding of how it works.
“I wish I could alter criteria and see what the score is after that , with another set of observations. A lot of the time… I wonder what they’re sitting at , now that I’ve [altered] the bit that I’m not concerned about… It would be quite helpful to refresh it and have their score refreshed as the new score.” – Junior doctor.
Derivation of the decision-making model
Guided by the responses of our participants regarding their decision-making processes, our literature search identified a narrative review by Banning (2008) that reported previous work by O’Neill et al. (2005) [ 28 , 29 ]. While these studies referred to models of nurse decision-making, we selected a model (Fig. 2 ) that also appropriately described the responses of doctors in our participant group and matched the context of using clinical decision support systems to support clinical judgement. As an example, when clinicians referenced needing to look for certain data points to give context to a patient assessment, this was mapped to nodes relating to “Current patient data,” “Changes to patient status/data,” and “Hypothesis-driven assessment.”
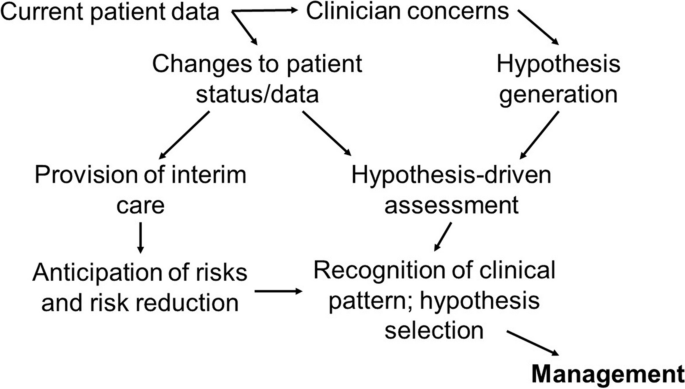
Decision-making model(Adapted from Neill’s clinical decision making framework [2005] and modified by Banning [2006]) with sequential decision nodes
Mapping of themes to decision-making model
The themes from Table 1 were mapped to the nodes in the decision-making model based on close alignment with participant responses (see Fig. 3 ). This mapping is further explained below, where the nodes in the model are described in parentheses.
Value of additional information for decision-making : participants stressed the importance of understanding not only the data going into the prediction model, but also how that data changed over time as trends, and the data that were not included in the model. (Current patient data, changes to patient status/data)
Format, frequency, and relevance of outputs : participants suggested a change in patient data should not always lead to an alert. Doctors, but not necessarily nurses, proposed outputs displayed as probabilities rather than scores, tying model predictions to potential diagnoses or prognoses. (Changes to patient status/data, hypothesis generation)
Using models to validate but not supersede clinical intuition : Depending on the exact timing of model outputs within the pathway of patient assessment, participants found predictions could either augment or hinder the hypothesis generation process. (Hypothesis generation)
Measuring risks objectively : Risk scores can assist with triaging or prioritising patients by urgency or prognostic risk, thereby potentially leading to early intervention to identify and/or prevent adverse events. (Clinician concerns, hypothesis generation)
Supporting critical thinking and reducing over-protocolised care : by acting as triggers for further assessment, participants suggested prediction models can support or discount diagnostic hypotheses, lead to root-cause identification, and facilitate interim cares, for example by ensuring good fit of nasal prongs. (Provision of interim care, hypothesis generation, hypothesis-driven assessment)
Model transparency and interactivity : understanding how prediction models worked, being able to modify or add necessary context to model predictions, and understanding the relative contribution of different predictors could better assist the generation and selection of different hypotheses that may explain a given risk score. (Hypothesis generation, recognition of clinical pattern and hypothesis selection)
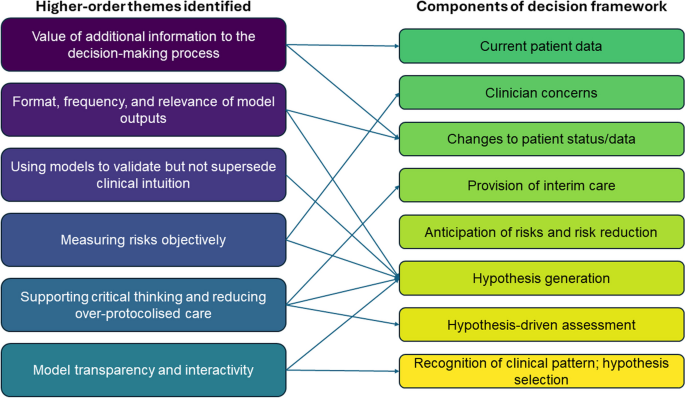
Mapping of the perceived relationships between higher-order themes and nodes in the decision-making model shown in Fig. 2
Recommendations for improving the design of prediction models
Based on the mapping of themes to the decision-making model, we formulated four recommendations for enhancing the development and deployment of prediction models for clinical deterioration.
Improve accessibility and transparency of data included in the model. Provide an interface that allows end-users to see what predictor variables are included in the model, their relative contributions to model outputs, and facilitate easy access to data not included in the model but still relevant for model-informed decisions, e.g., trends of predictor variables over time.
Present model outputs that are relevant to the end-user receiving those outputs, their responsibilities, and the tasks they may be obliged to perform, while preserving the ability of clinicians to apply their own discretionary judgement.
In situations associated with diagnostic uncertainty, avoid tunnel vision from priming clinicians with possible diagnostic explanations based on model outputs, prior to more detailed clinical assessment of the patient.
Support critical thinking whereby clinicians can apply a more holistic view of the patient’s condition, take all relevant contextual factors into account, and be more thoughtful in generating and selecting causal hypotheses.
This qualitative study involving front-line acute care clinicians who respond to early warning score alerts has generated several insights into how clinicians perceive the use of prediction models for clinical deterioration. Clinicians preferred models that facilitated critical thinking, allowed an understanding of the impact of variables included and excluded from the model, provided model outputs specific to the tasks and responsibilities of different disciplines of clinicians, and supported decision-making processes in terms of hypotheses and choice of management, rather than simply responding to alerts in a pre-specified, mandated manner. In particular, preventing prediction models from supplanting critical thinking was repeatedly emphasised.
Reduced staffing ratios, less time spent with patients, greater reliance on more junior workforce, and increasing dependence on automated activation of protocolised management are all pressures that could lead to a decline in clinical reasoning skills. This problem could be exacerbated by adding yet more predictive algorithms and accompanying protocols for other clinical scenarios, which may intensify alert fatigue and disrupt essential clinical care. However, extrapolating our results to areas other than clinical deterioration should be done with caution. An opposing view may be that using prediction models to reduce the burden of routine surveillance may allow redirection of critical thinking skills towards more useful tasks, a question that has not been explored in depth in the clinical informatics literature.
Clinicians expressed interest in models capable of providing causal insights into clinical deterioration. This is neither a function nor capability of most risk prediction models, requiring different assumptions and theoretical frameworks [ 30 ]. Despite this limitation, risk nomograms, visualisations of changes in risk with changes in predictor variables, and other interactive tools for estimating risk may be useful adjuncts for clinical decision-making due to the ease with which input values can be manipulated.
Contributions to the literature
Our research supports and extends the literature on the acceptability of risk prediction models within clinical decision support systems. Common themes in the literature supporting good practices in clinical informatics and which are also reflected in our study include: alert fatigue; the delivery of more relevant contextual information; [ 31 ] the value of patient histories; [ 32 , 33 ] ranking relevant information by clinical importance, including colour-coding; [ 34 , 35 ] not using computerised tools to replace clinical judgement; [ 32 , 36 , 37 ] and understanding the analytic methods underpinning the tool [ 38 ]. One other study has investigated the perspectives of clinicians of relatively simple, rules-based prediction models similar to Q-ADDS. Kappen et al [ 12 ] conducted an impact study of a prediction model for postoperative nausea and vomiting and also found that clinicians frequently made decisions in an intuitive manner that incorporated information both included and absent from prediction models. However, the authors recommended a more directive than assistive approach to model-based recommendations, possibly due to a greater focus on timely prescribing of effective prophylaxis or treatment.
The unique contribution of our study is a better understanding of how clinicians may use prediction models to generate and validate diagnostic hypotheses. The central role of critical thinking and back-and-forth interactions between clinician and model in our results provide a basis for future research using more direct investigative approaches like cognitive task analysis [ 39 ]. Our study has yielded a set of cognitive insights into decision making that can be applied in tandem with statistical best practice in designing, validating and implementing prediction models. [ 19 , 40 , 41 ].
Relevance to machine learning and artificial intelligence prediction models for deterioration
Our results may generalise to prediction models based on machine learning (ML) and artificial intelligence (AI), according to results of several recent studies. Tonekaboni et al [ 42 ] investigated clinician preferences for ML models in the intensive care unit and emergency department using hypothetical scenarios. Several themes appear both in our results and theirs: a need to understand the impact of both included and excluded predictors on model performance; the role of uncertain or noisy data in prediction accuracy; and the influence of trends or patient trajectories in decision making. Their recommendations for more transparent models and the delivery of model outputs designed for the task at hand align closely with ours. The authors’ focus on clinicians’ trust in the model was not echoed by our participants.
Eini-Porat et al [ 43 ] conducted a comprehensive case study of ML models in both adult and paediatric critical care. Their results present several findings supported by our participants despite differences in clinical environments: the value of trends and smaller changes in several vital signs that could cumulatively signal future deterioration; the utility of triage and prioritisation in time-poor settings; and the use of models as triggers for investigating the cause of deterioration.
As ML/AI models proliferate in the clinical deterioration prediction space, [ 44 ] it is important to deeply understand the factors that may influence clinician acceptance of more complex approaches. As a general principle, these methods often strive to input as many variables or transformations of those variables as possible into the model development process to improve predictive accuracy, incorporating dynamic updating to refine model performance. While this functionality may be powerful, highly complex models are not easily explainable, require careful consideration of generalisability, and can prevent clinicians from knowing when a model is producing inaccurate predictions, with potential for patient harm when critical healthcare decisions are being made [ 45 , 46 , 47 ]. Given that our clinicians emphasised the need to understand the model, know which variables are included and excluded, and correctly interpret the format of the output, ML/AI models in the future will need to be transparent in their development and their outputs easily interpretable.
Limitations
The primary limitations of our study were that our sample was drawn from two hospitals with high levels of digital maturity in a metropolitan region of a developed country, with a context specific to clinical deterioration. Our sample of 15 participants may be considered small but is similar to that of other studies with a narrow focus on clinical perspectives [ 42 , 43 ]. All these factors can limit generalisability to other settings or to other prediction models. As described in the methods, we used open-ended interview templates and generated our inductive themes reflexively, which is vulnerable to different types of biases compared to more structured preference elicitation methods with rigidly defined analysis plans. Member checking may have mitigated this bias, but was not possible due to the time required from busy clinical staff.
Our study does not directly deal with methodological issues in prediction model development, [ 41 , 48 ] nor does it provide explicit guidance on how model predictions should be used in clinical practice. Our findings should also not be considered an exhaustive list of concerns clinicians have with prediction models for clinical deterioration, nor may they necessarily apply to highly specialised clinical areas, such as critical care. Our choice of decision making framework was selected because it demonstrated a clear, intuitive causal pathway for model developers to support the clinical decision-making process. However, other, equally valid frameworks may have led to different conclusions, and we encourage more research in this area.
This study elicited clinician perspectives of models designed to predict and manage impending clinical deterioration. Applying these perspectives to a decision-making model, we formulated four recommendations for the design of future prediction models for deteriorating patients: improved transparency and interactivity, tailoring models to the tasks and responsibilities of different end-users, avoiding priming clinicians with diagnostic predictions prior to in-depth clinical review, and finally, facilitating the diagnostic hypothesis generation and assessment process.
Availability of data and materials
Due to privacy concerns and the potential identifiability of participants, interview transcripts are not available. However, interview guides are available in the supplement.
Jenkins DA, Martin GP, Sperrin M, Riley RD, Debray TPA, Collins GS, Peek N. Continual updating and monitoring of clinical prediction models: time for dynamic prediction systems? Diagn Prognostic Res. 2021;5(1):1.
Article Google Scholar
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594.
Article PubMed Google Scholar
Moons KG, Altman DG, Reitsma JB, Ioannidis JP, Macaskill P, Steyerberg EW, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162(1):W1–73.
Blythe R, Parsons R, White NM, Cook D, McPhail SM. A scoping review of real-time automated clinical deterioration alerts and evidence of impacts on hospitalised patient outcomes. BMJ Qual Saf. 2022;31(10):725–34.
Fahey M, Crayton E, Wolfe C, Douiri A. Clinical prediction models for mortality and functional outcome following ischemic stroke: a systematic review and meta-analysis. PLoS ONE. 2018;13(1):e0185402.
Article PubMed PubMed Central Google Scholar
Fleuren LM, Klausch TLT, Zwager CL, Schoonmade LJ, Guo T, Roggeveen LF, et al. Machine learning for the prediction of sepsis: a systematic review and meta-analysis of diagnostic test accuracy. Intensive Care Med. 2020;46(3):383–400.
White NM, Carter HE, Kularatna S, Borg DN, Brain DC, Tariq A, et al. Evaluating the costs and consequences of computerized clinical decision support systems in hospitals: a scoping review and recommendations for future practice. J Am Med Inform Assoc. 2023;30(6):1205–18.
Sanders S, Doust J, Glasziou P. A systematic review of studies comparing diagnostic clinical prediction rules with clinical judgment. PLoS ONE. 2015;10(6):e0128233.
Abell B, Naicker S, Rodwell D, Donovan T, Tariq A, Baysari M, et al. Identifying barriers and facilitators to successful implementation of computerized clinical decision support systems in hospitals: a NASSS framework-informed scoping review. Implement Sci. 2023;18(1):32.
van der Vegt AH, Campbell V, Mitchell I, Malycha J, Simpson J, Flenady T, et al. Systematic review and longitudinal analysis of implementing Artificial Intelligence to predict clinical deterioration in adult hospitals: what is known and what remains uncertain. J Am Med Inf Assoc. 2024;31(2):509–24.
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8.
Kappen TH, van Loon K, Kappen MA, van Wolfswinkel L, Vergouwe Y, van Klei WA, et al. Barriers and facilitators perceived by physicians when using prediction models in practice. J Clin Epidemiol. 2016;70:136–45.
Witteman HO, Dansokho SC, Colquhoun H, Coulter A, Dugas M, Fagerlin A, Giguere AM, Glouberman S, Haslett L, Hoffman A, Ivers N. User-centered design and the development of patient decision aids: protocol for a systematic review. Systematic reviews. 2015;4:1−8.
Zhang J, Norman DA. Representations in distributed cognitive tasks. Cogn Sci. 1994;18(1):87–122.
Johnson CM, Johnson TR, Zhang J. A user-centered framework for redesigning health care interfaces. J Biomed Inf. 2005;38(1):75–87.
Jones D, Mitchell I, Hillman K, Story D. Defining clinical deterioration. Resuscitation. 2013;84(8):1029–34.
Morgan RJ, Wright MM. In defence of early warning scores. Br J Anaesth. 2007;99(5):747–8.
Article CAS PubMed Google Scholar
Smith ME, Chiovaro JC, O’Neil M, Kansagara D, Quinones AR, Freeman M, et al. Early warning system scores for clinical deterioration in hospitalized patients: a systematic review. Annals Am Thorac Soc. 2014;11(9):1454–65.
Baker T, Gerdin M. The clinical usefulness of prognostic prediction models in critical illness. Eur J Intern Med. 2017;45:37–40.
Campbell V, Conway R, Carey K, Tran K, Visser A, Gifford S, et al. Predicting clinical deterioration with Q-ADDS compared to NEWS, between the flags, and eCART track and trigger tools. Resuscitation. 2020;153:28–34.
The Australian Commission on Safety and Quality in Health is the publisher, and the publisher location is Sydney, Australia. https://www.safetyandquality.gov.au/sites/default/files/migrated/35981-ChartDevelopment.pdf .
Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18(1):148.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are Enough? Qual Health Res. 2017;27(4):591–608.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):1–8.
Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a New Framework for Theorizing and evaluating nonadoption, abandonment, and challenges to the Scale-Up, Spread, and sustainability of Health and Care technologies. J Med Internet Res. 2017;19(11):e367.
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Res Psychol. 2021;18(3):328–52.
Campbell KA, Orr E, Durepos P, Nguyen L, Li L, Whitmore C, et al. Reflexive thematic analysis for applied qualitative health research. Qualitative Rep. 2021;26(6):2011–28.
Google Scholar
Banning M. A review of clinical decision making: models and current research. J Clin Nurs. 2008;17(2):187–95.
O’Neill ES, Dluhy NM, Chin E. Modelling novice clinical reasoning for a computerized decision support system. J Adv Nurs. 2005;49(1):68–77.
Arnold KF, Davies V, de Kamps M, Tennant PWG, Mbotwa J, Gilthorpe MS. Reflection on modern methods: generalized linear models for prognosis and intervention—theory, practice and implications for machine learning. Int J Epidemiol. 2020;49(6):2074–82.
Article PubMed Central Google Scholar
Westerbeek L, Ploegmakers KJ, de Bruijn GJ, Linn AJ, van Weert JCM, Daams JG, et al. Barriers and facilitators influencing medication-related CDSS acceptance according to clinicians: a systematic review. Int J Med Informatics. 2021;152:104506.
Henshall C, Marzano L, Smith K, Attenburrow MJ, Puntis S, Zlodre J, et al. A web-based clinical decision tool to support treatment decision-making in psychiatry: a pilot focus group study with clinicians, patients and carers. BMC Psychiatry. 2017;17(1):265.
Weingart SN, Simchowitz B, Shiman L, Brouillard D, Cyrulik A, Davis RB, et al. Clinicians’ assessments of electronic medication safety alerts in ambulatory care. Arch Intern Med. 2009;169(17):1627–32.
Baysari MT, Zheng WY, Van Dort B, Reid-Anderson H, Gronski M, Kenny E. A late attempt to involve end users in the design of medication-related alerts: Survey Study. J Med Internet Res. 2020;22(3):e14855.
Trafton J, Martins S, Michel M, Lewis E, Wang D, Combs A, et al. Evaluation of the acceptability and usability of a decision support system to encourage safe and effective use of opioid therapy for chronic, noncancer pain by primary care providers. Pain Med. 2010;11(4):575–85.
Wipfli R, Betrancourt M, Guardia A, Lovis C. A qualitative analysis of prescription activity and alert usage in a computerized physician order entry system. Stud Health Technol Inform. 2011;169:940–4.
PubMed Google Scholar
Cornu P, Steurbaut S, De Beukeleer M, Putman K, van de Velde R, Dupont AG. Physician’s expectations regarding prescribing clinical decision support systems in a Belgian hospital. Acta Clin Belg. 2014;69(3):157–64.
Ahearn MD, Kerr SJ. General practitioners’ perceptions of the pharmaceutical decision-support tools in their prescribing software. Med J Australia. 2003;179(1):34–7.
Swaby L, Shu P, Hind D, Sutherland K. The use of cognitive task analysis in clinical and health services research - a systematic review. Pilot Feasibility Stud. 2022;8(1):57.
Steyerberg EW. Applications of prediction models. In: Steyerberg EW, editor. Clinical prediction models. New York: Springer-; 2009. pp. 11–31.
Chapter Google Scholar
Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–31.
Tonekaboni S, Joshi S, McCradden MD, Goldenberg A. What Clinicians Want: Contextualizing Explainable Machine Learning for Clinical End Use. In: Doshi-Velez F, Fackler J, Jung K, Kale D, Ranganath R, Wallace B, Wiens J, editors. Proceedings of the 4th Machine Learning for Healthcare Conference; Proceedings of Machine Learning Research: PMLR; 2019;106:359–80.
Eini-Porat B, Amir O, Eytan D, Shalit U. Tell me something interesting: clinical utility of machine learning prediction models in the ICU. J Biomed Inform. 2022;132:104107.
Muralitharan S, Nelson W, Di S, McGillion M, Devereaux PJ, Barr NG, Petch J. Machine learning-based early warning systems for clinical deterioration: systematic scoping review. J Med Internet Res. 2021;23(2):e25187.
Rudin C. Stop Explaining Black Box Machine Learning Models for high stakes decisions and use interpretable models instead. Nat Mach Intell. 2019;1(5):206–15.
Blythe R, Parsons R, Barnett AG, McPhail SM, White NM. Vital signs-based deterioration prediction model assumptions can lead to losses in prediction performance. J Clin Epidemiol. 2023;159:106–15.
Futoma J, Simons M, Panch T, Doshi-Velez F, Celi LA. The myth of generalisability in clinical research and machine learning in health care. Lancet Digit Health. 2020;2(9):e489–92.
Steyerberg EW, Uno H, Ioannidis JPA, van Calster B, Collaborators. Poor performance of clinical prediction models: the harm of commonly applied methods. J Clin Epidemiol. 2018;98:133–43.
Download references
Acknowledgements
We would like to thank the participants who made time in their busy clinical schedules to speak to us and offer their support in recruitment.
This work was supported by the Digital Health Cooperative Research Centre (“DHCRC”). DHCRC is funded under the Commonwealth’s Cooperative Research Centres (CRC) Program. SMM was supported by an NHMRC-administered fellowships (#1181138).
Author information
Authors and affiliations.
Australian Centre for Health Services Innovation and Centre for Healthcare Transformation, School of Public Health and Social Work, Faculty of Health, Queensland University of Technology, 60 Musk Ave, Kelvin Grove, Brisbane, QLD, 4059, Australia
Robin Blythe, Sundresan Naicker, Nicole White & Steven M McPhail
Princess Alexandra Hospital, Metro South Health, Woolloongabba, QLD, Australia
Raelene Donovan & Andrew McKelliget
Queensland Digital Health Centre, Faculty of Medicine, University of Queensland, Brisbane, QLD, Australia
Ian A. Scott
Digital Health and Informatics Directorate, Metro South Health, Woolloongabba, QLD, Australia
Ian A. Scott & Steven M McPhail
You can also search for this author in PubMed Google Scholar
Contributions
RB: conceptualisation, data acquisition, analysis, interpretation, writing. SN: data acquisition, analysis, interpretation, writing. NW: interpretation, writing. RD: data acquisition, interpretation, writing. IS: data acquisition, analysis, interpretation, writing. AM: data acquisition, interpretation, writing. SM: conceptualisation, data acquisition, analysis, interpretation, writing. All authors have approved the submitted version and agree to be accountable for the integrity and accuracy of the work.
Corresponding author
Correspondence to Robin Blythe .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Metro South Human Research Ethics Committee (HREC/2022/QMS/84205). Informed consent was obtained prior to interview scheduling, with all participants filling out a participant information and consent form. Consent forms were approved by the ethics committee. Participation was entirely voluntary, and could be withdrawn at any time. All responses were explicitly deemed confidential, with only the first two study authors and the participant privy to the research data. Interviews were then conducted in accordance with Metro South Health and Queensland University of Technology qualitative research regulations. For further information, please contact the corresponding author.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Blythe, R., Naicker, S., White, N. et al. Clinician perspectives and recommendations regarding design of clinical prediction models for deteriorating patients in acute care. BMC Med Inform Decis Mak 24 , 241 (2024). https://doi.org/10.1186/s12911-024-02647-4
Download citation
Received : 06 September 2023
Accepted : 23 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12911-024-02647-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical prediction models
- Clinical decision support systems
- Early warning score
- Clinical deterioration
- Clinical decision-making
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Learn why critical thinking is essential for nurses and how to improve it with case-based learning, self-reflection, questioning, self-awareness, and a process. See examples of how nurses use critical thinking to make decisions, solve problems, and provide excellent care.
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills. The web page explains the elements, importance, and ways to develop and apply critical-thinking skills in nursing.
Critical thinking in nursing is the process of solving problems related to patient care using evidence and reasoning. Learn why critical thinking is important, what attributes make it excellent, and how to improve it with 18 tips and examples.
Critical thinking is a cognitive process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions. It is a vital skill for nurses, enabling them to provide safe and effective care to patients. Learn the key aspects, levels, and benefits of critical thinking in nursing practice.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
For nurses, critical thinking means being able to make sound clinical judgments that can significantly affect patient outcomes. The connection between critical thinking and patient safety. Patient safety is a fundamental aspect of healthcare quality. It involves preventing errors, reducing harm, and ensuring optimal outcomes for patients.
Learn how critical thinking enhances patient outcomes, improves decision-making, and fosters evidence-based practice in nursing. Find out the components, benefits, and tips of critical thinking in nursing, and how to overcome barriers to it.
Clinical Reasoning, Decisionmaking, and Action: Thinking ...
Critical thinking in nursing is the deliberate process of collecting, interpreting, analyzing, and evaluating information to make clinical judgments. Learn why critical thinking is important, what skills are involved, and how nurses apply them in real-life scenarios.
Learn how to apply critical thinking in nursing to analyze, evaluate, and synthesize information to make informed decisions. Explore examples of critical thinking in nursing scenarios and supplement your nursing studies with SimpleNursing's interactive tools.
Learn how critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. Explore the definition, benefits, stages, and skills of critical thinking in nursing, and see examples and a word cloud of related terms.
Learn how to develop strong critical thinking skills for nursing practice with 24 strategies and examples. Explore techniques such as reflective journaling, concept mapping, Socratic questioning, clinical simulations, and more.
A rapid response article argues that nursing practice demands sound judgement and decision-making skills as critical thinking and clinical reasoning is an essential component of nursing practice. The article cites various sources to support the importance of critical thinking and clinical reasoning for nurses and suggests that education must begin at the undergraduate level to develop students ...
Learn what critical thinking in nursing is, why it is important, and what skills are involved. Critical thinking enables nurses to observe, analyze, and apply evidence-based information to support favorable patient outcomes.
Learn how to use critical thinking skills to make informed decisions, provide top-notch care, and untangle complex problems in nursing. Explore the 15 attitudes of critical thinking in nursing, such as independence, confidence, fair-mindedness, and more, with examples and strategies.
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Learn why critical thinking is essential for nurses to make sound decisions and provide quality care, and how to improve this skill in nursing school and on the job. Find out how the nursing process, the chain of command and leadership roles can help you think critically in different situations.
Critical thinking has become a buzz phrase in education and corporate environments in recent years. The definitions vary slightly, but most agree that thinking critically includes some form of judgement that thinkers generate after careful analysis of the perspectives, opinions, or experimental results present for a particular problem or situation.
Abstract Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. ... In this context, the ethics of virtue is a theoretical framework that becomes essential for analyse the critical thinking concept in nursing care and nursing science. Because the ethics ...
Learn the definition, components, levels, and importance of critical thinking in nursing. Explore strategies to improve your critical thinking skills and overcome barriers with case studies and exercises.
1 Introduction. Critical thinking in nursing is considered essential for delivering quality care and reflects the professional accountability of registered nurses (Chang et al., 2011). It is also a vital part of the clinical assignments and responsibilities nurses are expected to manage. Additionally, nurses' critical thinking has the ...
Critical thinking in nursing is the ability to assess, analyze, and make informed decisions quickly and efficiently. It involves logical reasoning, problem-solving, and the ability to evaluate evidence to make sound clinical judgments. This skill is essential for nurses, especially in emergency situations where time and accuracy are of the essence.
1. INTRODUCTION. Critical thinking is defined as the cognitive process of reasoning that involves trying to minimize errors and to maximize positive outcomes while attempting to make a decision during patient care (Zuriguel‐Pérez et al., 2015).The importance of critical thinking in nursing practice has been identified in the literature (Chang et al., 2011; Ludin, 2018; Mahmoud & Mohamed ...
Introduction. Key principles within Malcolm Knowles' andragogy theory (Knowles et al., 2012) include that adults learn best when they have a personal experience with the content and when learning is problem-centered.Although much of nursing education aligns didactic, simulation, and clinical learning in a way that students simultaneously gain knowledge and experience, some lessons involve ...
Despite the numerous advantages of the nursing process, nursing students often struggle with utilizing this model. Therefore, studies suggest innovative teaching methods to address this issue. Teaching based on real clinical cases is considered a collaborative learning method that enhances students' active learning for the development of critical thinking and problem-solving skills.
Background: Despite the numerous advantages of the nursing process, nursing students often struggle with utilizing this model. Therefore, studies suggest innovative teaching methods to address this issue. Teaching based on real clinical cases is considered a collaborative learning method that enhances students' active learning for the development of critical thinking and problem-solving skills.
Fifteen nurses (n = 8) and doctors (n = 7) were interviewed for a mean duration of 42 min. Participants emphasised the importance of using predictive tools for supporting rather than supplanting critical thinking, avoiding over-protocolising care, incorporating important contextual information and focusing on how clinicians generate, test, and ...