National Archives News

The Flu Pandemic of 1918

Red Cross workers make anti-influenza masks for soldiers, Boston, Massachusetts. (National Archives Identifier 45499341 )
Before COVID-19, the most severe pandemic in recent history was the 1918 influenza virus, often called “the Spanish Flu.” The virus infected roughly 500 million people—one-third of the world’s population—and caused 50 million deaths worldwide (double the number of deaths in World War I). In the United States, a quarter of the population caught the virus, 675,000 died, and life expectancy dropped by 12 years. With no vaccine to protect against the virus, people were urged to isolate, quarantine, practice good personal hygiene, and limit social interaction. Until February 2020, the 1918 epidemic was largely overlooked in the teaching of American history, despite the ample documentation at the National Archives and elsewhere of the disease and its devastation. The 100-year-old pictures from 1918 that just months ago seemed quaint and dated now seem oddly prescient. We make these records more widely available in hopes that they contain lessons about what to expect over the coming months and ideas about ways to avoid a repeat and prepare for what may follow.
Online Exhibit
A selection of photographs and documents from the National Archives' nationwide holdings tell the story of the 1918 influenza pandemic.
Photographs
(Click image to view gallery)

Images from the 1918 Flu Pandemic
Female clerks in New York City wear masks at work. (National Archives Identifier 45499337 )
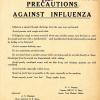
Department of the Navy: Precautions Against Influenza. (National Archives Identifier 6861947 )
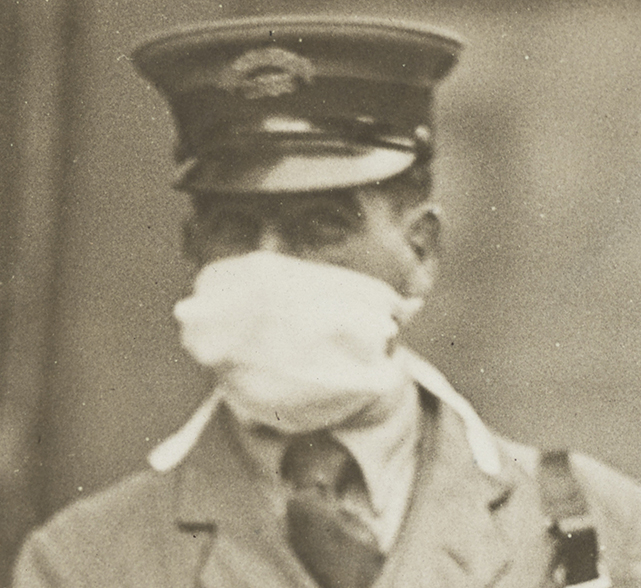
Traffic "cop" in New York City wearing gauze mask. (National Archives Identifier 45499301 )
New York City "conductorettes" wearing masks. (National Archives Identifier 45499323 )
Letter carrier in New York City wearing mask. (National Archives Identifier 45499319 )
To prevent the spread of Spanish Influenza, Cincinnati barbers are wearing masks. (National Archives Identifier 45499317 )
Additional Photographs
- Red Cross volunteer nurses in Eureka, CA
- Red Cross Women’s Motor Corps aids injured patients
- Red Cross workers in Seattle
- Street cleaner in mask
- Boston Red Cross workers making masks for soldiers
- Female elevator operator in New York City
- Eberts Field, Lonoke, AR: Convalescent influenza patients in hospital overflow space
- Emergency hospital, Brookline, MA, to care for influenza cases
- Fighting influenza in Seattle: Flu serum injection
- A nurse wearing a mask fills water from a pitcher
- Mother and daughter work on a quilt for soldiers
- Red Cross Motor Corps on duty
- San Francisco police court meets in open air for influenza prevention
Author Lecture
Dr. Jeremy Brown, Director of Emergency Care Research, National Institutes of Health, spoke about his book Influenza: The Hundred-Year Hunt to Cure the Deadliest Disease in History, at the National Archives in Washington, DC, on March 5, 2019.
Archival Film
Nurses make bandages for flu epidemic (stock newsreel footage from CBS)
Blogs and Social Media Posts
Forward with Roosevelt: One of the Millions: FDR and the Flu Pandemic of 1918–1920
Text Message: The “Spanish Flu” Pandemic of 1918–1919: A Death in Philadelphia
Pieces of History: Pandemic Nursing: The 1918 Influenza Outbreak
Pieces of History: Influenza Epidemic 1918—“Wear a mask and save your life”
Pieces of History: Gesundheit!
Unwritten Record: The 1918 Influenza Pandemic
Today's Document: Precautions Against Influenza
Tumblr: 1918 to COVID-19
Tumblr: Influenza Epidemic 1918—“Wear a mask and save your life”
For Educators
Influenza Directive from DC re: treatment and procedures , 9/26/1918
Influenza Prophylaxis Memo from Third Naval District Medical Officer
Documents Related to the Flu Pandemic of 1918
Memo Re: Sanitary Precautions, 9/12/1918
Additional primary sources and educational resources from DocsTeach
At the Presidential Libraries
Truman Library: Letter from Harry to Bess , referencing the influenza epidemic, and expressing relief that Bess has recovered from it.
Ford Library: Remarks Upon the Signing of National Swine Flu Immunization Program of 1976
Ford Library: President Asks Congress for $135 Million for Swine Flu Vaccine Ford Library: Fact Sheet on Swine Influenza Immunization Program
George W. Bush Library: Pandemic Flu: Preparing and Protecting against Avian Influenza
Barack Obama Library: Declaration of Nat’l Emergency - 2009 H1N1 Influenza Pandemic
Barack Obama Library: Press Briefing On Swine Influenza
Posts Related to COVID-19
National Archives COVID-19 Updates
AOTUS Blog: National Archives Operations During COVID-19: Mission Critical Functions Continue
AOTUS Blog: National Archives Donates Protective Gear for COVID-19 Response
National Archives News: National Personnel Records Center Continues Serving Veterans During COVID-19 Pandemic
National Archives News: National Archives Donates Protective Gear for COVID-19 Response
Office of the Federal Register: COVID-19 Procedures
Press Release: Information on NHPRC and COVID-19
Records Management: Frequently Asked Questions (FAQs) About Records Management During the COVID-19 Pandemic

Sign Up Today
Start your 14 day free trial today

History Hit Story of England: Making of a Nation
- 20th Century
10 Facts About the Deadly 1918 Spanish Flu Epidemic

Léonie Chao-Fong
12 feb 2020.

The 1918 influenza pandemic, also known as the Spanish flu, was the deadliest epidemic in world history.
An estimated 500 million worldwide were infected, and the death toll was anywhere from between 20 to 100 million.
Influenza, or flu, is a virus that attacks the respiratory system. It is highly contagious: when an infected person coughs, sneezes or talks, droplets are transmitted into the air and can be inhaled by anyone nearby.
A person can also be infected by touching something with the flu virus on it, and then touching their mouth, eyes or nose.
Although a pandemic of the influenza virus had already killed thousands in 1889, it was not until 1918 that the world discovered how deadly the flu could be.
Here are 10 facts about the 1918 Spanish flu.
1. It struck in three waves across the world
Three pandemic waves: weekly combined influenza and pneumonia mortality, United Kingdom, 1918–1919 (Credit: Centers for Disease Control and Prevention ).
The first wave of the 1918 pandemic took place in the spring of that year, and was generally mild.
Those infected experienced typical flu symptoms – chills, fever, fatigue – and usually recovered after several days. The number of reported deaths was low.
In the autumn of 1918, the second wave appeared – and with a vengeance.
Victims died within hours or days of developing symptoms. Their skin would turn blue, and their lungs would fill with fluids, causing them to suffocate.
In the space of one year, the average life expectancy in the United States plummeted by a dozen years.
A third, more moderate, wave hit in the spring of 1919. By the summer it had subsided.
2. Its origins are unknown to this day

Demonstration at the Red Cross Emergency Ambulance Station in Washington, D.C. (Credit: Library of Congress ).
The 1918 flu was first observed in Europe, America and parts of Asia, before rapidly spreading across every part of the world within a matter of months.
It remains unknown where the particular strain of influence – the first pandemic involving the H1N1 influenza virus – came from.
There is some evidence to suggest that the virus came from a bird or farm animal in the American Midwest, travelling among the animal species before mutating into a version that took hold in the human population.
Some claimed the epicentre was a military camp in Kansas, and that it spread through the US and into Europe via the troops who travelled east to fight in the First World War.
Others believe it originated in China, and was transported by labourers heading for the western front.

3. It did not come from Spain (despite the nickname)
Despite its colloquial name, the 1918 flu did not originate from Spain.
The British Medical Journal referred to the virus as “Spanish flu” because Spain was hit hard by the disease. Even Spain’s king, Alfonso XIII, reportedly contracted the flu.
In addition, Spain was not subject to the wartime news censorship rules that affected other European countries.
In response, Spaniards named the illness the “Naples soldier”. The German army called it “ Blitzkatarrh ”, and British troops referred to it as “Flanders grippe” or the “Spanish lady”.

U.S. Army Camp Hospital No. 45, Aix-Les-Bains, France.
4. There were no drugs or vaccines to treat it
When the flu hit, doctors and scientists were unsure what caused it or how to treat it. At the time, there were no effective vaccines or antivirals to treat the deadly strain.
People were advised to wear masks, avoid shaking hands, and to stay indoors. Schools, churches, theatres and businesses were shuttered, libraries put a halt on lending books and quarantines were imposed across communities.
Bodies began to pile up in makeshift morgues, while hospitals quickly became overloaded with flu patients. Doctors, health staff and medical students became infected.

Demonstration at the Red Cross Emergency Ambulance Station in Washington, D.C (Credit: Library of Congress ).
To complicate things further, the Great War had left countries with a shortage of physicians and health workers.
It was not until the 1940s that the first licensed flu vaccine appeared in the US. By the following decade, vaccines were routinely produced to help control and prevent future pandemics.
5. It was particularly deadly for young and healthy people

Volunteer nurses from the American Red Cross tending influenza sufferers in the Oakland Auditorium, Oakland, California (Credit: Edward A. “Doc” Rogers ).
Most influenza outbreaks only claim as fatalities juveniles, the elderly, or people who are already weakened. Today, flu is especially dangerous for under 5-year-olds and those over 75.
The 1918 influenza pandemic, however, affected completely healthy and strong adults between 20 and 40 years of age – including millions of World War One soldiers.
Surprisingly, children and those with weaker immune systems were spared from death. Those aged 75 and above had the lowest death rate of all.
6. The medical profession tried to play down its severity
In the summer of 1918, the Royal College of Physicians claimed the flu was no more threatening than the “Russian flu” of 1189-94.
The British Medical Journal accepted that overcrowding on transport and in the workplace was necessary for the war effort, and implied that the “inconvenience” of the flu should be quietly borne.
Individual doctors also did not fully comprehend the severity of the disease, and tried to play it down to avoid spreading anxiety.
In Egremont, Cumbria, which saw an appalling death rate, the medical officer requested the rector stop ringing the church bells for each funeral because he wanted to “keep people cheerful”.
The press did likewise. ‘The Times’ suggested that it was probably a result of “the general weakness of nerve-power known as war-weariness”, while ‘The Manchester Guardian’ scorned protective measures saying:
Women are not going to wear ugly masks.

7. 25 million people died in the first 25 weeks
As the second wave of the autumn hit, the flu epidemic spiralled out of control. In most cases, haemorrhages in the nose and lungs killed victims within three days.
International ports – usually the first places in a country to be infected – reported serious problems. In Sierra Leone, 500 out of 600 dock workers fell too sick to work.
Epidemics were quickly seen in Africa, India and the Far East. In London, the spread of the virus became far more deadly and contagious as it mutated.

Chart showing mortality from the 1918 influenza pandemic in the US and Europe (Credit: National Museum of Health and Medicine ).
10% of the entire population of Tahiti died within three weeks. In Western Samoa, 20% of the population died.
Each division of the US armed services reported hundreds of deaths each week. After the Liberty Loan parade in Philadelphia on 28 September, thousands of people became infected.
By the summer of 1919, those who were infected had either died or developed immunity, and the epidemic finally came to an end.
8. It reached almost every single part of the world
The 1918 epidemic was of a truly global scale . It infected 500 million people across the world, including those on remote Pacific Islands and in the Arctic.
In Latin America, 10 out of every 1,000 people died; in Africa, it was 15 per 1,000. In Asia, the death toll reached as high as 35 in every 1,000.
In Europe and America, troops travelling by boat and train took the flu into cities, from where it spread to the countryside.
Only St Helena in the South Atlantic and a handful of South Pacific islands did not report an outbreak.
9. The exact death toll is impossible to know

Memorial to the thousands of victims of New Zealand’s 1918 epidemic (Credit: russellstreet / 1918 Influenza Epidemic Site ).
The estimated death toll attributed to the 1918 flu epidemic is usually at 20 million to 50 million victims worldwide. Other estimates run as high as 100 million victims – around 3% of the world’s population.
However it is impossible to know what the exact death toll was, due to the lack of accurate medical record-keeping in many infected places.
The epidemic wiped out entire families, destroyed whole communities and overwhelmed funeral parlours across the world.
10. It killed more people than World War One combined
More American soldiers died from the 1918 flu than were killed in battle during the First World War. In fact, the flu claimed more lives than all of the World War One battles combined .
The outbreak turned the previously strong, immune systems against them: 40% of the US navy were infected, while 36% of the army became ill.
Featured image: Emergency hospital during 1918 influenza epidemic, Camp Funston, Kansas ( National Museum of Health and Medicine )
You May Also Like

How a find in Scotland opens our eyes to an Iranian Empire

Do you know who built Petra?

The Dark History of Bearded Ladies

Did this Document Legitimise the Yorkists Claim to the Throne?

The Strange Sport of Pedestrianism Got Victorians Hooked on Coca

Puzzle Over These Ancient Greek Paradoxes

In Ancient Rome, Gladiators Rarely Fought to the Death

Archaeologists Uncover Two Roman Wells on a British Road

Young Stalin Made His Name as a Bank Robber

3 Things We Learned from Meet the Normans with Eleanor Janega

Reintroducing ‘Dan Snow’s History Hit’ Podcast with a Rebrand and Refresh

Don’t Try This Tudor Health Hack: Bathing in Distilled Puppy Juice
The 1918 Flu Pandemic: Why It Matters 100 Years Later

Here are 5 things you should know about the 1918 pandemic and why it matters 100 years later.
1. The 1918 Flu Virus Spread Quickly

In 1918, many people got very sick, very quickly. In March of that year, outbreaks of flu-like illness were first detected in the United States. More than 100 soldiers at Camp Funston in Fort Riley Kansas became ill with flu. Within a week, the number of flu cases quintupled. There were reports of some people dying within 24 hours or less. 1918 flu illness often progressed to organ failure and pneumonia, with pneumonia the cause of death for most of those who died. Young adults were hit hard. The average age of those who died during the pandemic was 28 years old.
2. No Prevention and No Treatment for the 1918 Pandemic Virus

3. Illness Overburdened the Health Care System
As the numbers of sick rose, the Red Cross put out desperate calls for trained nurses as well as untrained volunteers to help at emergency centers. In October of 1918, Congress approved a $1 million budget for the U. S. Public Health Service to recruit 1,000 medical doctors and more than 700 registered nurses.
At one point in Chicago, physicians were reporting a staggering number of new cases, reaching as high as 1,200 people each day. This in turn intensified the shortage of doctors and nurses. Additionally, hospitals in some areas were so overloaded with flu patients that schools, private homes and other buildings had to be converted into makeshift hospitals, some of which were staffed by medical students.
4. Major Advancements in Flu Prevention and Treatment since 1918

There is still much work to do to improve U.S. and global readiness for the next flu pandemic. More effective vaccines and antiviral drugs are needed in addition to better surveillance of influenza viruses in birds and pigs. CDC also is working to minimize the impact of future flu pandemics by supporting research that can enhance the use of community mitigation measures (i.e., temporarily closing schools, modifying, postponing, or canceling large public events, and creating physical distance between people in settings where they commonly come in contact with one another). These non-pharmaceutical interventions continue to be an integral component of efforts to control the spread of flu, and in the absence of flu vaccine, would be the first line of defense in a pandemic.
5. Risk of a Flu Pandemic is Ever-Present, but CDC is on the Frontlines Preparing to Protect Americans

CDC works tirelessly to protect Americans and the global community from the threat of a future flu pandemic. CDC works with domestic and global public health and animal health partners to monitor human and animal influenza viruses. This helps CDC know what viruses are spreading, where they are spreading, and what kind of illnesses they are causing. CDC also develops and distributes tests and materials to support influenza testing at state, local, territorial, and international laboratories so they can detect and characterize influenza viruses. In addition, CDC assists global and domestic experts in selecting candidate viruses to include in each year’s seasonal flu vaccine and guides prioritization of pandemic vaccine development. CDC routinely develops vaccine viruses used by manufacturers to make flu vaccines. CDC also supports state and local governments in preparing for the next flu pandemic, including planning and leading pandemic exercises across all levels of government. An effective response will diminish the potential for a repeat of the widespread devastation of the 1918 pandemic.
Visit CDC’s 1918 commemoration website for more information on the 1918 pandemic and CDC’s pandemic flu preparedness work.
63 comments on “The 1918 Flu Pandemic: Why It Matters 100 Years Later”
Comments listed below are posted by individuals not associated with CDC, unless otherwise stated. These comments do not represent the official views of CDC, and CDC does not guarantee that any information posted by individuals on this site is correct, and disclaims any liability for any loss or damage resulting from reliance on any such information. Read more about our comment policy » .
Hi, Thank you for this article. Very informative. Maybe the people that do not understand and do not accept the vaccination campaign will change their minds.
Excellent historical perspective on the 1918 incident. We have come a long way in treatment protocols and diagnostic advancements with respect to infectious diseases. The major concern,at this time, is an unknown pathogen which will be quickly spread worldwide my international jet travel. A few sick people on an aircraft entering the US could easy spread the disease from one end of the Country to the other. Depending on the conditions’ incubation period many more people will be affected before public health officials begin to see a problem. I guess the only thing we can be sure of is something similar will occur again , it’s just a matter of the right conditions and time.
This is a wonderful article on the influenza virus. I have extensively read about the pandemic, and its devastating effect on people. I must admit that I am appalled at the refusal to use trained nurses because they were Black Americans. That nonsense was part of the failure to help people in need of care at this crucial time . I must say it was hateful and ignorant of White Americans. White Americans are not reminded enough that they are immigrants to America just like any other race that came to this country from another country. America does not belong to white people. I don’t believe sick people care who is attending to them when they are on the brink of death.
Well done article. However. You could include a list of historical accounts for Further reading materials.
The possibility of another potential outbreak of any kind is a very scary and real test of how very little know. We indeed have come along way but still have a distance to go. .. Thank you for sharing this fascinating story.
Two of my grandparents were killed in their 30s by this epidemic, leaving my 1 year-old mother, my aunt, and my uncle orphaned. This is important stuff; people need to take influenza seriously.
My grandfather was a doctor in the Spokane Wa area and died from the flu in July of 1918 at age 46 . He was from the St Louis Missouri area and had been in the Spokane area for several years but could have visited or was visited by people from the St Louis area which is close to Kansas City to have caught the flu . Spokane was very isolated . This article gives no answer but gives some background to how he caught the flu in the middle of nowhere at the beginning of this pandemic
Would the mortality rate be as bad as the flu pandemic in 1918 where 675,000 people were killed? How would our economy be affected? Any thoughts?
The book “The Great Influenza” by John M. Barry has many historical references on this topic.
Good summary of the 1918 flu pandemic. But the sentence “The average age of those who died during the pandemic was 28 years old” (end of the first section) is inaccurate. Twenty-eight was the age at which mortality peaked among young adults, who were the hardest hit, along the very young and the very old. As for the average, variations in infant or old adult mortality could easily tip the balance away from 28 years.
In researching flu a few years ago, I read that one reason this flu killed people of supposedly optimum age for strength and resistance (~28 years), was for exactly that reason – their immune systems responded so quickly – with fluid in the lungs – that they drowned. People who responded more slowly, with less fluid produced less quickly – were more likely to survive.
By the way, if this thing posts (my first post ever on this site), I’m getting this message:
You are posting comments too quickly. Slow down.
(Please check your software)
I would agree with Tonya and Robert, there is an ever-present threat of a variant flu virus reeking havoc as many go unprepared for each flu season by not vaccinating, but also with a new, unknown pathogen. With the climate changing and the glacier ice melting to new low levels, bacteria, viruses and parasites previously encased in ice soon may be exposed to air, water, and humans. I am thankful for the diligent surveillance that the CDC and the WHO provides.
Thank you for that summary. The pandemic took my grandmother in the Spring of 1919. My father and his two sisters were orphans then. Their father had died in France, November 1918. It is always so sad for me to read about this.
Any plan to slow or stop a pandemic would include quickly identifying those who are contagious and minimizing their contact with others. However we do not have in place policies that would encourage that behavior, particularly in the low income and immigrant populations, including people who: * cannot afford to take time off work without pay * would lose their jobs if they did not show up * have no health insurance and can’t afford medical care * are afraid to seek care because of immigration status (their own or family member’s) And anyone who was quarantined would want to know that their basic needs would be met if they complied. I believe these issues would be best addressed in advance to overcome resistance. Once a potential pandemic starts, it will be difficult to get the necessary public and private buy-in, resources and authority until it is too late.
It’s surprising that to see that the first three items listed would apply to any similar pandemic of unknown origin today. Today’s air travel would spread an illness at previously unheard of rates. Couple that with an unknown origin and our health care systems would be over run just as they were in 1918.
Thank you so much for this article. I appreciate the information included and I pray that it convinces people with reservations to keep their own and their families health in mind for everyone’s sake but especially their own.
My grandmother was 11 years old in 1918. The family was from Philadelphia. I remember her telling me that she had to help load dead bodies into wagons. They would yell in the neighborhoods, “throw out your dead!” She never got the flu, but it must have been horrible! That is why we were always told never to spit on the streets. It can carry diseases, etc. People—Don’t think this cannot happen again. We live in an age where we can prevent the worst from happening when it comes to flu and other diseases. Get your flu shots!
Very educative write-up. A big lesson for us in Africa. The surveillance of influenza viruses must be sustained especially at animal-human interface to monitor possible new mutations. Thank you.
My grandfather was 15 years old. His parents and his two siblings were very ill with the flu so he ran to get help. By the time he got back to the house they were all dead. I am lying in bed with the H1N1 right now. Probably the sickest I’ve ever been. I personally believe facemasks should be mandatory and all public transportation. What a tragedy all the way around.
Great information on the flu pandemic. Very educative and sad.
History has taught us much about various past outbreaks. It’s the future unknown pathogens manmade or natural we need to worry about.
Great article on the flu pandemic. I have done a lot of studying on the issue. John Barry has written many books about the pandemic I find it incredible and riveting to learn about how people would wake up in the morning feeling fine and be dead in the evening. I have spoken to many people who experienced the flu through their families. I have always wondered if this can never happen again. Let’s hope not.
Great informative article thanks I`ve just been watching THE LATEST NEWS ON THE 2020 CORONAVIRUS! making me wonder ?? I also remember COLLAPSING as I was walking down the street with HONG KONG FLU in 1956 Woke up in hospital…..TOOK MANY WEEKS TO RECOVER!!
while air travel will spread the virus faster today than before, the news of such virus is traveling even faster today, as can be seen in the current outbreak of 2019CoV. People around the world are in a state of panic as soon as it is reported. China did a total lock down pretty quickly. Nowadays, we get more information about the characteristics of the virus, like the temperature and humidity condition that is favorable/unfavorable to it, Scientists can produce a vaccine much sooner than before. So yes, we should be vigilant, but we do not need to be too scared to live our life normally.
Reading this in 2020, and it looks like the U.S. has not learned much.
those who do not know history are doomed to repeat it.
Actually, if you read how fast the flu spread, and how many died, some within 24 hours, we have come a long way! It took over 30 years to develop a flu vaccine, and within 3 months of coronavirus hitting, we have already started the clinical trials of a vaccine. Amazing!!
It’s like you saw into the future. The very not so distant future. Thanks for writing this as it reinforces the steps and procedures being followed today. If only they had been implemented sooner.
Here we go all over again
From this article I think WHO and CDC have not learned much to be in preparation. After 100 year another virus is here to take million lives away. Poor nation like Africa is in trouble. America should have known better to be prepare after 100years. God save us all
Apparently, there was no national plan then either. The lack of leadership by politicians on national and local levels is appalling and the realization that many top officials refuse to accept and follow recommendations of the CDC and other experts is terrifying. We are following exactly the same recommendations as were suggested in 1918, and there is inconsistent use of the precautions that we know help. Please support those who are taking the Coronavirus seriously and working to help us all. Bless the CDC and Drs and nurses on the front lines trying to save us all.
Great information
Watching the overrun hospitals, lack of supplies and reliance on local and state authorities because the federal government cannot or will not help. Schools are canceled. All groups more than 10 people. Social distancing rules are in place. The economy is crashing. No possible vaccine. History is repeating itself. I am literally hiding in my home with my family, knowing it’s the only way to avoid it.
Thank you for this article. It certainly puts the current COVID-19 pandemic in perspective, as well as reinforcing the need for social distancing! We are fortunate to live in a time when significant advances have been made in medicine and technology.
The CDC dropped the ball on this one, we need to shut down the country to prevent a worst case scenario. (writing this on 3/30/20) The economy will tank no matter what, but we can prevent millions of deaths yet.
My mother’s cousin was 21 when the 1918 influenza epidemic hit. He had cerebral palsy and was at risk for disease and he died. It’s hard though to comprehend how the influenza reached his tiny town outside of Abilene, Texas. There was very little medicine for colds or pneumonia for anyone in that time period.
100 years later viruses are still a problem.
The history repeats itself, we can see USA as the richest country, powerful country, is so unprepared! Doctors and nurses are lacking of protective gears, yet they have to work with the patients who are infected with the virus! The States have to bid against one another for ventilators etc. So many people are infected and die from this neglected, unguided way ! So sad!
Very informative information and thanks to all those people that put this information together. It seems to be working for this coronavirus we are currently experiencing. Keep up the good work and lets try to do our best to improve what we have learned from this virus and make it better next time around as we can see …. there will be a next time …. just currently unknown as to when.
Sydney Daniels Looking back at the comments in 2018 it is haunting. The accuracy of concerns and predictions! The rapid spread through international travel , the less privileged forced to continue working ,not only to perish but spread it. The fear of an unknown pathogen and it’s economic impact. The parallels of past and present are too hard to ignore. The Spanish flu acting very similar to Coronavirus. There are several stories in the news of patients over 100, who were alive during the 1918 flu, surviving coronavirus. Is it a stretch to think whatever immunity they acquired back in 1918 could have given them an edge or are they just tough as nails!? Is it immunologically impossible being a different virus and the years past? Just a thought? Unfortunately the reassurance, given in this article, that we have multiple guardrails in place to prevent such a huge spread again was wishful thinking. God bless everyone and stay safe.
My grandfather died from the Spanish flu and struck both my father and uncle as children. My father suffered cardiomyopathy and succumbed to it decades later. Financial struggles where perhaps worse since women had less legal rights and job opportunities that had any semblance of equal pay. My grandmother supported her family through a variety of seamstress jobs and cleaning for those that could afford that luxury. History is a good teacher if we can learn from it.
Watching the BOSSA. 45 min documentary on the spanish flu of 1918 so enlightening also. The symptoms of severe cases were bizarre and freakish, fatal in less than 24 hrs. A second wave (fall 2020) of covid must be minimized if world wants to prevent millions of deaths. Unfortunately, so many spoiled americans are selfish and very impatient willing to risk and sacrifice many others lives for a day at the beach or a new tattoo. If only they all could have done a 6 month sentence in county jail they would see that they could stomach months of quarantine in their own homes standing on their head, provided ample food and necessities are avialable.Too bad history will be repeated and this will be a disaster for so many more that shall lose their lives
here we go again!
102 years later and the struggles that our ancestors dealt with daily are being resurfaced again. As an RN working in the frontlines with the current flu pandemic, the level of stress that is experienced among health care workers is almost unbearable. Just as the 1918 flu was fast to spread with no prevention or treatment plan in place, this new outbreak is fast to spread and hard to treat and prevent. Taking a lesson from the 1918 pandemic, our facility took to making the staff and the patients wear mask for all interactions during their stay at our facility in an effort to reduce the risk of spreading patient to nurse or nurse to patient. The most unnerving concern to me personally is the fact that unlike the 1918 flu, an estimated 50% of individuals who have the COVID-19 virus have experienced zero symptoms. This makes the task of identifying the positive patients from simple screening procedures much more difficult due to lack of testing ability to confirm actual positive patients. For example, we had an elderly man in our facility for more than two weeks for an unrelated health care issue, screening upon admission declared he was a zero risk for COVID-19 and he never exhibited a single symptom during his admission, however upon discharge and transfer to a rehab facility, he had a COVID-19 positive test result. He continues to have ZERO symptoms but has exposed multiple health care workers and family members to COVID-19. The risk of infecting health care workers who are already spread thin only increases the workload demand on those still able to work.
We are currently short staffed at our facility with most nurses working four to six 12 hour shifts per week to keep the work demand in our facility at a manageable level. With the re-opening of our surgical units and other outpatient services, the “extra” support we were receiving from their health care staff has diminished but the increased workload demand on the inpatient staff is ever growing as the community continues to open up and social distancing is not adhered to. Our COVID-19 related ER visits more than doubled over one weekend when beaches alone opened up. As with the 1918 pandemic, the call for help in many areas had been made even to the point of allowing current nursing students to perform duties as an RN.
Because health care facilities across our nation are short staffed and limited on PPE, the task of identifying positive flu patients is important to isolate the continued spread of the virus but to also protect the health care workers and reduce the waste of precious PPE. Just as our health care workers in the past, social distancing, hand washing and face covers are the best methods that we have available to help slow the spread of this virus.
A hard lesson learned in the 1918 pandemic was that the early shut down of large social events and gatherings could help slow the spread and decrease the the burden on the local healthcare facilities. The CDCs plans of closing down schools, shopping centers, social gatherings of large numbers, and bars/clubs was the outcome of that hard learned lesson from 1918. Our community seems to have fared well with the early closing as we have not had many local citizens hospitalized with COVID-19, we do have a many COVID-19 patients in our facilities due to hospital transfers however due to our location being near two other States, one of which is a well known hot zone. We are all in this together and just like our 1918 health care teams, we too have answered the call to aid our neighboring States.
Opening up the public with care and caution is going to have to occur as many small business owners have already had to close their doors to our community permanently due to the length of time they went with no income. The economical impact this virus had already had on our community is evident and will only be truly seen in the future as things begin to return to our “New” normal.
COVID19 will also last for years as compared to Spanish flu and we should take the precautionary measures seriously
That was hard to read , here we are again in 2020.
im postin just to post kepp up the good work guys
It was so good but it was only 100 years and we have a sickness that is killing the people.
My father and his younger sister both had the flu in Glasgow in 1919. He survived, his sister died. He never had the flu again, and I have never had it…I’m 81 now. I’ve been told I am immune and have never had the flu shot. There is an area south of Glasgow/northern England that has been studied because there is are a number of people there who are also immune. J. Wilson Saville
To keep this thread (article) in check and updated I’d like to add that there was hope of a slow down. However, the desire for normalcy has in turn resulted in a resurgence of the virus. Hospitals are now getting brunt of the aged ill. Some retirement homes are nearly at 75% plus positive to the virus, whereas; the nurses are infected as well and even though now overtaken by the virus are capable of working. In my opinion, this will continue for another year. I hope the timeframe is less, but the end result will likely be another depression. Our country needs to prepare and seek aid from other countries to prepare for this. The USA are the worlds leading consumers and I dint believe the rest of the world could take a financial hit like a US collapse.
Well, vaccines are on the way. Half of America is still crazy. I guess you could say we started “rounding the corner” on Nov. 3rd. Hopefully things back to normal this time next year.
Very good and informative article. Thank you
The Spanish fly and the COVID -19 are are bit similar
When roll out to massive vaccinate happens worldwide we will heal. It reminds me of the World War 2 armament. Once we got the ball rolling we were successful.
I was always strong never in the hospital because of illness. October 2020 came , and despite all my efforts to avoid COVID-19 I landed in the local hospital, and spent the month of October in the covid unit. The infectious disease specialists went to work with what was available, and saved my life. I was on oxygen until March, or April, and I was doing rehab at home until I could walk again. Thank God my wife and I were able to get our COVID-19 shots. Please get yours, everyone!!!
History have already repeating it self In a bad way and we did not learn anything at all ! .
The covid -19 or coronavirus in 2020
Life expectancy dropped by 12 years during the Spanish flu. The virus continued until 1957. Some believe a lack of nutrition played a part in the mortality rate at the time Life expectancy for COVID 19 is the same as normal life expectancy (around 78). Like the Spanish flu our body should adapt to the coming variations. Like the Spanish flu it may last decades.
Why was there a 37 year absence of flu pandemic between 1920 & 1957; yet subsequent to 1957 they have appeared more frequently?
@Sumeyo, I think you mean “The Spanish Flu” 😉
people did not learn about the requirements for this😑. I mean really!
Good info and everything but could had added more info
The article was worded very well and fairly informative. And that leads me to bring up a part of the Article that most people tend to over look. The flu started in the military and spread rapidly. When i was six years old i had very similar symptoms of the Spanish flue and I compared the symptoms of covid 19 and what I had when it was six was actually worse. Im 55 yrs old now and I haven’t had a flu shot in 36 years now and I have no intentions of getting another one with all the Chemical war fair going on in the world.
Post a Comment
Your email address will not be published. Required fields are marked *
To receive email updates about this page, enter your email address:

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center

- What is the difference between influenza epidemics and influenza pandemics?
- What is pandemic influenza preparedness?
- What are the symptoms of influenza?
- What have been some of the world’s deadliest pandemics?
- How do pandemics end?

influenza pandemic of 1918–19
Our editors will review what you’ve submitted and determine whether to revise the article.
- Cleveland Clinic - Spanish Flu
- PNAS - Genesis and pathogenesis of the 1918 pandemic H1N1 influenza A virus
- New Zealand History Online - The 1918 influenza pandemic
- National Archives - The Flu Pandemic of 1918
- Ohio State University - Origins - The 1918 Flu Pandemic
- Live Science - 1918 influenza: The deadliest pandemic in history
- National Center for Biotechnology Information - PubMed Central - 1918 Influenza: the Mother of All Pandemics
- Pan American Health Organization - Purple Death: The Great Flu of 1918
- Newfoundland and Labrador Heritage - The 1918 Spanish Flu
- influenza pandemic of 1918–19 - Student Encyclopedia (Ages 11 and up)

What was the influenza pandemic of 1918–1919?
The influenza pandemic of 1918–1919 was the most severe influenza outbreak of the 20th century. The disease that caused this devastating pandemic has also been called the Spanish flu.
What caused the influenza pandemic of 1918–1919?
A virus called influenza type A subtype H1N1 is now known to have been the cause of the extreme mortality of the influenza pandemic of 1918–1919.
Which countries were affected by the influenza pandemic of 1918-1919?
Outbreaks of the influenza pandemic of 1918-1919 occurred in nearly every inhabited part of the world. Although it remains uncertain where the virus first emerged, it quickly spread through western Europe and around the world—first in ports, then from city to city along main transportation routes.
How many people died as a result of the influenza pandemic of 1918–1919?
The influenza pandemic of 1918–1919 resulted in an estimated 25 million deaths, though some researchers have projected that it caused as many as 40–50 million deaths.
influenza pandemic of 1918–19 , the most severe influenza outbreak of the 20th century and, in terms of total numbers of deaths, among the most devastating pandemics in human history.
- Read more about the impact of the COVID-19 pandemic .

Influenza is caused by a virus that is transmitted from person to person through airborne respiratory secretions. An outbreak can occur if a new strain of influenza virus emerges against which the population has no immunity. The influenza pandemic of 1918–19 resulted from such an occurrence and affected populations throughout the world. An influenza virus called influenza type A subtype H1N1 is now known to have been the cause of the extreme mortality of this pandemic, which resulted in an estimated 25 million deaths, though some researchers have projected that it caused as many as 40–50 million deaths.

The pandemic occurred in three waves. The first apparently originated in early March 1918, during World War I . Although it remains uncertain where the virus first emerged, it quickly spread through western Europe, and by July it had spread to Poland. The first wave of influenza was comparatively mild. However, during the summer a more lethal type of disease was recognized, and this form fully emerged in August 1918. Pneumonia often developed quickly, with death usually coming two days after the first indications of the flu. For example, at Camp Devens, Massachusetts, U.S., six days after the first case of influenza was reported, there were 6,674 cases. The third wave of the pandemic occurred in the following winter, and by the spring the virus had run its course. In the two later waves about half the deaths were among 20- to 40-year-olds, an unusual mortality age pattern for influenza.
Outbreaks of the flu occurred in nearly every inhabited part of the world, first in ports, then spreading from city to city along the main transportation routes. India is believed to have suffered at least 12.5 million deaths during the pandemic, and the disease reached distant islands in the South Pacific, including New Zealand and Samoa . In the United States about 550,000 people died. Most deaths worldwide occurred during the brutal second and third waves. Other outbreaks of Spanish influenza occurred in the 1920s but with declining virulence.
The Spanish flu: The global impact of the largest influenza pandemic in history
Parts of the article were revised in May 2023, and the chart on death tolls from flu pandemics was updated in April 2024.
In the last 150 years the world has seen an unprecedented improvement in health. The visualization shows that in many countries life expectancy, which measures the average age of death, doubled from around 40 years or less to more than 80 years. This was not just an achievement across the countries shown here; life expectancy has doubled in all regions of the world.
What also stands out is how abrupt and damning negative health events can be. Most striking is the large, sudden decline of life expectancy in 1918, caused by an unusually deadly influenza pandemic that became known as the ‘Spanish flu’.
To make sense of the fact life expectancy declined so abruptly, one has to keep in mind what it measures. Period life expectancy , which is the precise name for this measure, captures the mortality in one particular year . It summarizes the mortality in a particular year by calculating the average age of death of a hypothetical cohort of people for which that year’s mortality pattern would remain constant throughout their entire lifetimes.
This influenza outbreak wasn’t restricted to Spain and it didn’t even originate there. Recent genetic research suggests that the strain emerged a few years earlier, around 1915, but did not take off until later on. The earliest recorded outbreak was in Kansas in the United States in 1918. 1
But it was named as such because Spain was neutral in the First World War (1914-18), which meant it was free to report on the severity of the pandemic, while countries that were fighting tried to suppress reports on how the influenza impacted their population to maintain morale and not appear weakened in the eyes of the enemies. Since it is very valuable to speak openly about the threat of an infectious disease I think Spain should be proud that it was not like other countries at that time.
The virus spread rapidly and eventually reached all parts of the world: the epidemic became a pandemic. 2 Even in a much less-connected world the virus eventually reached extremely remote places such as the Alaskan wilderness and Samoa in the middle of the Pacific islands. In these remote places the mortality rate was often particularly high. 3
How many people died in the Spanish flu pandemic?
The global death count of the flu today:.
To have a context for the severity of influenza pandemics it might be helpful to know the death count of a typical flu season. Current estimates for the annual number of deaths from influenza are around 400,000 deaths per year. Paget et al (2019) suggest an average of 389,000 with an uncertainty range 294,000 from 518,000. 4 This means that in recent years the flu was responsible for the death of 0.005% of the world population. 5 Even in comparison to the low estimate for the death count of the Spanish flu (17.4 million) this pandemic, more than a century ago, caused a death rate that was 182-times higher than today’s baseline.

Global deaths of the Spanish flu
Several research teams have worked on the difficult problem of reconstructing the global health impact of the Spanish flu.
The visualization here shows the available estimates from the different research publications discussed in the following. The range of published estimates for the Spanish flu is particularly wide.
The widely cited study by Johnson and Mueller (2002) arrives at a very high estimate of at least 50 million global deaths. But the authors suggest that this could be an underestimation and that the true death toll was as high as 100 million. 6
Patterson and Pyle (1991) estimated that between 24.7 and 39.3 million died from the pandemic. 7
The more recent study by Spreeuwenberg et al. (2018) concluded that earlier estimates have been too high. Their own estimate is 17.4 million deaths. 8
The global death rate of the Spanish flu
How do these estimates compare with the size of the world population at the time? How large was the share who died in the pandemic?
Estimates suggest that the world population in 1918 was 1.8 billion.
Based on this, the low estimate of 17.4 million deaths by Spreeuwenberg et al. (2018) implies that the Spanish flu killed almost 1% of the world population. 9
The estimate of 50 million deaths published by Johnson and Mueller implies that the Spanish flu killed 2.7% of the world population. And if it was in fact higher – 100 million as these authors suggest – then the global death rate would have been 5.4%. 10
The world population was growing by around 13 million every year in this period which suggests that the period of the Spanish flu was likely the last time in history when the world population was declining. 11
Other large influenza pandemics
The Spanish flu pandemic was the largest, but not the only large recent influenza pandemic.
Two decades before the Spanish flu the Russian flu pandemic (1889-1894) is believed to have killed 1 million people. 12
Estimates for the death toll of the “Asian Flu” (1957-1958) range from 1.7 to 2.7 million according to Spreeuwenberg et al. (2018). 13
The same authors estimate that the “Hong Kong Flu” (1968-1969) killed between 2 and 3.8 million people. 13
The “Russian Flu” pandemic of 1889-1890 is believed to be caused by an H3 pandemic virus. 14 According to Spreeuwenberg et al. (2018) around 3.7 to 5.1 million people died worldwide. 13
The “Swine flu” pandemic of 2009-2010 was caused by a new H1N1 pandemic virus. Several research groups have made estimates of the global death toll, which ranges from 130,000 to 1.87 million people worldwide. 15
What becomes clear from this overview are two things: influenza pandemics are not rare, but the Spanish flu of 1918 was by far the most devastating influenza pandemic in recorded history.
The impact of the Spanish flu on different age groups
This last visualization here shows the life expectancy in England and Wales by age.
The red line shows the life expectancy for a newborn, with the rainbow-colored lines above showing how long a person could expect to live once they had reached that given, older, age. The light green line, for example, represents the life expectancy for children who have reached age 10.
It shows that life expectancy increased at all ages, which means that the often-heard assertion that life expectancy ‘only’ increased because child mortality declined is not true .
With respect to the impact of the Spanish flu it is striking that the visualization shows that the pandemic had little impact on older people. While the life expectancy at birth and at young ages declined by more than ten years, the life expectancy of 60- and 70-year olds saw no change. This is at odds with what one would reasonably expect: older populations tend to be most vulnerable to influenza outbreaks and respiratory infections. If we look at mortality for both lower respiratory infections (pneumonia) and upper respiratory infections today, death rates are highest for those who are 70 years and older.
This data tells us that young people accounted for a large share of the deaths, this made this pandemic especially devastating.
Why were older people so resilient to the 1918 pandemic? The research literature suggests that this was the case because older people had lived through an earlier flu outbreak – the already discussed ‘Russian flu pandemic’ of 1889–90 – which gave those who lived through it some immunity for the later outbreak of the Spanish flu. 16
The earlier 1889-90 pandemic might have given the older population some immunity, but was a destructive event in itself. According to Smith 132,000 people died in England, Wales, and Ireland alone. 17
How the Spanish flu differs from the Coronavirus outbreak in 2020
Writing in early March 2020 it is an obvious question to ask how the ongoing outbreak of Covid-19 compares. There are a number of important differences that should be considered.
They are not the same disease and the virus causing these diseases are very different. The virus that causes Covid-19 is a coronavirus, not an influenza virus that caused the Spanish flu and the other influenza pandemics listed above.
The age-specific mortality seems to be very different. As we’ve seen above, the Spanish flu in 1918 was especially dangerous to infants and younger people. The new coronavirus that causes Covid-19 appears to be most lethal to the elderly, based on early evidence in China. 18
We’ve also seen above that during the Spanish flu many countries tried to suppress any information about the influenza outbreak. Today the sharing of data, research, and news is certainly not perfect, but very different and much more open than in the past.
But it is true that the world today is much better connected. In 1918 it was railroads and steamships that connected the world. Today planes can carry people and viruses to many corners of the world in a very short time.
Differences in health systems and infrastructure also matter. The Spanish flu hit the world in the days before antibiotics were invented; and many deaths, perhaps most, were not caused by the influenza virus itself, but by secondary bacterial infections. Morens et al (2008) found that during the Spanish flu “the majority of deaths … likely resulted directly from secondary bacterial pneumonia caused by common upper respiratory–tract bacteria.” 19
And not just health systems were different, but also the health and living conditions of the global population. The 1918 flu hit a world population of which a very large share was extremely poor – large shares of the population were undernourished, in most parts of the world the populations lived in very poor health , and overcrowding, poor sanitation and low hygiene standards were common. Additionally the populations in many parts of the world were weakened by a global war. Public resources were small and many countries had just spent large shares of their resources on the war.
While most of the world is much richer and healthier now , the concern today too is that it is the poorest people that are going to be hit hardest by the Covid-19 outbreak. 20
These differences suggest that one should be cautious in drawing lessons from the outbreak a century ago.
But the Spanish flu reminds us just how large the impact of a pandemic can be, even in countries that had already been successful in improving population health. A new pathogen can cause terrible devastation and lead to the death of millions. For this reason the Spanish flu has been cited as a warning and as a motivation to prepare well for large pandemic outbreaks, which have been considered likely by many researchers. 21
Worobey, M., Han, G.-Z., & Rambaut, A. (2014). Genesis and pathogenesis of the 1918 pandemic H1N1 influenza A virus. Proceedings of the National Academy of Sciences, 111(22), 8107–8112. https://doi.org/10.1073/pnas.1324197111
Barry, J. M. (2004). The site of origin of the 1918 influenza pandemic and its public health implications. Journal of Translational Medicine, 2(1), 3. https://doi.org/10.1186/1479-5876-2-3
For the definitions of epidemic and pandemic see the CDC here .
Burnet F. M., Clark E. (1942) – Influenza: A Survey of the Last 50 Years in the Light of Modern Work on the Virus of Epidemic Influenza. London: Macmillan. Partly online on Google books.
The mortality rate in some populations like Alaska and Samoa were said to be 90% and 25% respectively. See the following two publications:
McLane, J. R. (2013). Paradise locked: The 1918 influenza pandemic in American Samoa. Sites: a journal of social anthropology and cultural studies , 10(2), 30-51.
Mamelund, S. E. (2017). Profiling a Pandemic. Who were the victims of the Spanish flu?{ref} While peak mortality was reached in 1918 the pandemic did not wane until two years later in late 1920.
Paget et al (2019) suggest an “average of 389 000 (uncertainty range 294 000-518 000) respiratory deaths were associated with influenza globally each year”.
John Paget, Peter Spreeuwenberg, Vivek Charu Robert J Taylor, A Danielle Iuliano, Joseph Bresee, Lone Simonsen, Cecile Viboud,3 and for the Global Seasonal Influenza-associated Mortality Collaborator Network and GLaMOR Collaborating Teams (2019) – Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. In J Glob Health. 2019 Dec; 9(2): 020421. Published online 2019 Oct 22. doi: 10.7189/jogh.09.020421 PMCID: PMC6815659 PMID: 31673337 Online here .
This is (389,000/7,500,000,000)*100=0.0052%
From the paper: Further research has seen the consistent upward revision of the estimated global mortality of the pandemic, which a 1920s calculation put in the vicinity of 21.5 million. A 1991 paper revised the mortality as being in the range 24.7-39.3 million. This paper suggests that it was of the order of 50 million. However, it must be acknowledged that even this vast figure may be substantially lower than the real toll, perhaps as much as 100 percent understated.
Johnson, N.P. and Mueller, J. (2002) – Updating the accounts: global mortality of the 1918-1920 “Spanish" influenza pandemic. In Bulletin of the History of Medicine, 76(1), pp.105-115. Online here .
The paper includes detailed breakdowns of mortality estimates by world region and country.
Patterson and Pyle (1991) wrote 'we believe that approximately 30 million is the best estimate for the terrible demographic toll of the influenza pandemic of 1918' and published a range from 24.7-39.3 million deaths.
Patterson, K.D. and Pyle, G.F. (1991) – The geography and mortality of the 1918 influenza pandemic. Bulletin of the History of Medicine, 65(1), p.4. Online here .
P. Spreeuwenberg; et al. (1 December 2018). "Reassessing the Global Mortality Burden of the 1918 Influenza Pandemic". American Journal of Epidemiology. 187 (12): 2561–2567. doi:10.1093/aje/kwy191. PMID 30202996. Online here .
The calculation is (17,400,000/1,832,196,157)*100=0.95
50,000,000 deaths / 1,832,196,157 people = 0.02729 And with a death count twice is high: 0.05458.
In available historical reconstructions (like this one ) this decline is not shown. The reason for this is that precise annual counts of the world population are not available for the past.
Instead historians try to reconstruct the population figures for 5-year or 10-year intervals and the annual estimates are interpolations between these estimates.
In other words, if we had precise annual counts they would likely show a decline of the world population in 1918.
Nickol, M.E., Kindrachuk, J. (2019) – A year of terror and a century of reflection: perspectives on the great influenza pandemic of 1918–1919. BMC Infect Dis 19, 117 (2019). https://doi.org/10.1186/s12879-019-3750-8
According to Smith (1995) 132,000 died in England, Wales, and Ireland alone.
Smith F. B. (1995) – The Russian influenza in the United Kingdom, 1889-1894. Soc. Hist. Med. 8 55–73. Online here .
Spreeuwenberg, P., Kroneman, M., & Paget, J. (2018). Reassessing the Global Mortality Burden of the 1918 Influenza Pandemic. American Journal of Epidemiology, 187(12), 2561–2567. https://doi.org/10.1093/aje/kwy191
Dawood, F. S., Iuliano, A. D., Reed, C., Meltzer, M. I., Shay, D. K., Cheng, P.-Y., Bandaranayake, D., Breiman, R. F., Brooks, W. A., Buchy, P., Feikin, D. R., Fowler, K. B., Gordon, A., Hien, N. T., Horby, P., Huang, Q. S., Katz, M. A., Krishnan, A., Lal, R., … Widdowson, M.-A. (2012). Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: A modelling study. The Lancet Infectious Diseases, 12(9), 687–695. https://doi.org/10.1016/S1473-3099(12)70121-4
Simonsen, L., Spreeuwenberg, P., Lustig, R., Taylor, R. J., Fleming, D. M., Kroneman, M., Van Kerkhove, M. D., Mounts, A. W., Paget, W. J., & the GLaMOR Collaborating Teams. (2013). Global Mortality Estimates for the 2009 Influenza Pandemic from the GLaMOR Project: A Modeling Study. PLoS Medicine, 10(11), e1001558. https://doi.org/10.1371/journal.pmed.1001558
Gagnon et al. (2013) – Age-Specific Mortality During the 1918 Influenza Pandemic: Unravelling the Mystery of High Young Adult Mortality.PLoS One. 2013; 8(8): e69586. Published online 2013 Aug 5. doi: 10.1371/journal.pone.0069586. Online here .
The Russian flu pandemic was a devastating event in itself. Smith (1995) estimates that the Russian flu killed 132,000 in England, Wales, and Ireland.
Zhonghua Liu Xing Bing Xue Za Zhi (2020) – The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Feb 17;41(2):145-151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. Online here .
Morens D. M., Taubenberger J. K., Fauci A. S. (2008) – Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J. Infect. Dis. 198 962–970. 10.1086/591708. Online here .
Gilbert, Marius, Giulia Pullano, Francesco Pinotti, Eugenio Valdano, Chiara Poletto, Pierre-Yves Boëlle, Eric D’Ortenzio, et al. (2020) – “Preparedness and Vulnerability of African Countries against Importations of COVID-19: A Modelling Study.” The Lancet (February 20, 2020). https://doi.org/10.1016/S0140-6736(20)30411-6 .
Alyssa S. Parpia, Martial L. Ndeffo-Mbah, Natasha S. Wenzel, and Alison P. Galvani (2016) – Effects of Response to 2014–2015 Ebola Outbreak on Deaths from Malaria, HIV/AIDS, and Tuberculosis, West Africa. In Emerg Infect Dis. 2016 Mar; 22(3): 433–441. doi: 10.3201/eid2203.150977 PMCID: PMC4766886 PMID: 26886846 Online here .
See for example: Pandemic influenza preparedness and response – WHO guidance document. Published in 2009 by the WHO. Online here .Roman Duda (2016) – Problem profile: Biorisk reduction. Published by 80,000 hours. Online here .
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
BibTeX citation
Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license . You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.
Our World in Data is free and accessible for everyone.
Help us do this work by making a donation.
- History Classics
- Your Profile
- Find History on Facebook (Opens in a new window)
- Find History on Twitter (Opens in a new window)
- Find History on YouTube (Opens in a new window)
- Find History on Instagram (Opens in a new window)
- Find History on TikTok (Opens in a new window)
- This Day In History
- History Podcasts
- History Vault
As the 1918 Flu Emerged, Cover‑Up and Denial Helped It Spread
By: Becky Little
Updated: October 4, 2023 | Original: May 26, 2020

“ Spanish flu ” has been used to describe the flu pandemic of 1918 and 1919 and the name suggests the outbreak started in Spain. But the term is actually a misnomer and points to a key fact: nations involved in World War I didn’t accurately report their flu outbreaks.
Spain remained neutral throughout World War I and its press freely reported its flu cases, including when the Spanish king Alfonso XIII contracted it in the spring of 1918. This led to the misperception that the flu had originated or was at its worst in Spain.
“Basically, it gets called the ‘Spanish flu’ because the Spanish media did their job,” says Lora Vogt , curator of education at the National WWI Museum and Memorial in Kansas City, Missouri. In Great Britain and the United States—which has a long history of blaming other countries for disease —the outbreak was also known as the “Spanish grip” or “Spanish Lady.”
Historians aren’t actually sure where the 1918 flu strain began, but the first recorded cases were at a U.S. Army camp in Kansas in March 1918. By the end of 1919, it had infected up to a third of the world’s population and killed some 50 million people. It was the worst flu pandemic in recorded history, and it was likely exacerbated by a combination of censorship, skepticism and denial among warring nations.
“The viruses don’t care where they come from, they just love taking advantage of wartime censorship,” says Carol R. Byerly, author of Fever of War: The Influenza Epidemic in the U.S. Army during World War I . “Censorship is very dangerous during a pandemic.”
The Flu in Europe

When the flu broke out in 1918, wartime press censorship was more entrenched in European countries because Europe had been fighting since 1914 , while the United States had only entered the war in 1917 . It’s hard to know the scope of this censorship, since the most effective way to cover something up is to not leave publicly-accessible records of its suppression. Discovering the impact of censorship is also complicated by the fact that when governments pass censorship laws, people often censor themselves out of fear of breaking the law.
In Great Britain, which fought for the Allied Powers, “the Defense of the Realm Act was used to a certain extent to suppress…news stories that might be a threat to national morale,” says Catharine Arnold , author of Pandemic 1918: Eyewitness Accounts from the Greatest Medical Holocaust in Modern History . “The government can slam what’s called a D-Notice on [a news story]—‘D’ for Defense—and it means it can’t be published because it’s not in the national interest.”
Both newspapers and public officials claimed during the flu’s first wave in the spring and early summer of 1918 that it wasn’t a serious threat. The Illustrated London News wrote that the 1918 flu was “so mild as to show that the original virus is becoming attenuated by frequent transmission.” Sir Arthur Newsholme, chief medical officer of the British Local Government Board, suggested it was unpatriotic to be concerned with the flu rather than the war, Arnold says.
The flu’s second wave, which began in late summer and worsened that fall, was far deadlier . Even so, warring nations continued to try to hide it. In August, the interior minister of Italy—another Allied Power— denied reports of the flu’s spread. In September, British officials and newspaper barons suppressed news that the prime minister had caught the flu while on a morale-boosting trip to Manchester. Instead, the Manchester Guardian explained his extended stay in the city by claiming he’d caught a “severe chill” in a rainstorm.
Warring nations covered up the flu to protect morale among their own citizens and soldiers, but also because they didn’t want enemy nations to know they were suffering an outbreak. The flu devastated General Erich Ludendorff’s German troops so badly that he had to put off his last offensive. The general, whose empire fought for the Central Powers, was anxious to hide his troops’ flu outbreaks from the opposing Allied Powers.
“Ludendorff is famous for observing [flu outbreaks among soldiers] and saying, oh my god this is the end of the war,” Byerly says. “His soldiers are getting influenza and he doesn’t want anybody to know, because then the French could attack him.”
The Pandemic in the United States

The United States entered WWI as an Allied Power in April 1917. A little over a year later, it passed the 1918 Sedition Act , which made it a crime to say anything the government perceived as harming the country or the war effort. Again, it’s difficult to know the extent to which the government may have used this to silence reports of the flu, or the extent to which newspapers self-censored for fear of retribution. Whatever the motivation, some U.S. newspapers downplayed the risk of the flu or the extent of its spread.
In anticipation of Philadelphia’s “Liberty Loan March” in September, doctors tried to use the press to warn citizens that it was unsafe. Yet city newspaper editors refused to run articles or print doctors’ letters about their concerns. In addition to trying to warn the public through the press, doctors had also unsuccessfully tried to convince Philadelphia’s public health director to cancel the march.
The war bonds fundraiser drew several thousand people, creating the perfect place for the virus to spread. Over the next four weeks, the flu killed 12,191 people in Philadelphia.

How U.S. Cities Tried to Halt the Spread of the 1918 Spanish Flu
How U.S. city officials responded to the 1918 pandemic played a critical role in how many residents lived—and died.
More People Died in the 1918 Flu Pandemic Than in WWI
See the heroes of the 1918 Spanish flu pandemic in color.
Why the Second Wave of the 1918 Flu Pandemic Was So Deadly
The first strain of the 1918 flu wasn’t particularly deadly. Then it came back in the fall with a vengeance.
Similarly, many U.S. military and government officials downplayed the flu or declined to implement health measures that would help slow its spread. Byerly says the Army’s medical department recognized the threat the flu posed to the troops and urged officials to stop troop transports, halt the draft and quarantine soldiers; but they faced resistance from the line command, the War Department and President Woodrow Wilson .
Wilson’s administration eventually responded to their pleas by suspending one draft and reducing the occupancy on troop ships by 15 percent, but other than that it didn’t take the extensive measures medical workers recommended. General Peyton March successfully convinced Wilson that the U.S. should not stop the transports, and as a result, soldiers continued to get sick. By the end of the year, about 45,000 U.S. Army soldiers had died from the flu.
The pandemic was so devastating among WWI nations that some historians have suggested the flu hastened the end of the war. The nations declared armistice on November 11 amid the pandemic’s worst wave.
In April 1919, the flu even disrupted the Paris Peace Conference when President Wilson came down with a debilitating case. As when the British prime minister had contracted the flu back in September, Wilson’s administration hid the news from the public. His personal doctor instead told the press the president had caught a cold from the Paris rain.

HISTORY Vault: World War I Documentaries
Stream World War I videos commercial-free in HISTORY Vault.

Sign up for Inside History
Get HISTORY’s most fascinating stories delivered to your inbox three times a week.
By submitting your information, you agree to receive emails from HISTORY and A+E Networks. You can opt out at any time. You must be 16 years or older and a resident of the United States.
More details : Privacy Notice | Terms of Use | Contact Us
Social and Economic Impacts of the 1918 Influenza Epidemic
India lost 16.7 million people. Five hundred and fifty thousand died in the US. Spain’s death rate was low, but the disease was called “Spanish flu” because the press there was first to report it.
A n estimated 40 million people, or 2.1 percent of the global population, died in the Great Influenza Pandemic of 1918–20. If a similar pandemic occurred today, it would result in 150 million deaths worldwide. In The Coronavirus and the Great Influenza Pandemic: Lessons from the “Spanish Flu” for the Coronavirus’s Potential Effects on Mortality and Economic Activity (NBER Working Paper 26866 ), Robert J. Barro , José F. Ursúa , and Joanna Weng study the cross-country differences in the death rate associated with the virus outbreak, and the associated impacts on economic activity.
The flu spread in three waves: the first in the spring of 1918, the second and most deadly from September 1918 to January 1919, and the third from February 1919 through the end of the year. The first two waves were intensified by the final years of World War I; the authors work to distinguish the effect of the flu on the death rate from the effect of the war. The flu was particularly deadly for young adults without pre-existing conditions, which increased its economic impact relative to a disease that mostly affects the very young and the very old.
The researchers analyze mortality data from more than 40 countries, accounting for 92 percent of the world’s population in 1918 and an even larger share of its GDP. The mortality rate varied from 0.3 percent in Australia, which imposed a quarantine in 1918, to 5.8 percent in Kenya and 5.2 percent in India, which lost 16.7 million people over the three years of the pandemic. The flu killed 550,000 in the United States, or 0.5 percent of the population. In Spain, 300,000 died for a death rate of 1.4 percent, around average. There is no consensus as to where the flu originated; it became associated with Spain because the press there was first to report it.
There is little reliable data on how many people were infected by the virus. The most common estimate, one third of the population, is based on a 1919 study of 11 US cities; it may not be representative of the US population, let alone the global population.
The researchers estimate that in the typical country, the pandemic reduced real per capita GDP by 6 percent and private consumption by 8 percent, declines comparable to those seen in the Great Recession of 2008–2009. In the United States, the flu’s toll was much lower: a 1.5 percent decline in GDP and a 2.1 percent drop in consumption.
The decline in economic activity combined with elevated inflation resulted in large declines in the real returns on stocks and short-term government bonds. For example, countries experiencing the average death rate of 2 percent saw real stock returns drop by 26 percentage points. The estimated drop in the United States was much smaller, 7 percentage points.
The researchers note that “the probability that COVID-19 reaches anything close to the Great Influenza Pandemic seems remote, given advances in public health care and measures that are being taken to mitigate propagation.” They note, however, that some of the mitigation efforts that are currently underway, particularly those affecting commerce and travel, are likely to amplify the virus’s impact on economic activity.
In a related study, Non-Pharmaceutical Interventions and Mortality in US Cities during the Great Influenza Pandemic, 1918–19 (NBER Working Paper 27049 ), Robert Barro analyzes data on the mitigation policies pursued by US cities as they confronted the flu epidemic. There were substantial cross-sectional differences in the policies that were adopted. Relative to the average number of flu deaths per week over the course of the epidemic, the number of flu deaths at the peak was lower in cities that pursued more aggressive policies, such as school closing and prohibition of public gatherings. However, the estimated effect of these policies on the total number of deaths was modest and statistically indistinguishable from zero. One potential explanation of this finding is that the interventions had a mean duration of only around one month.
— Steve Maas
Researchers
NBER periodicals and newsletters may be reproduced freely with appropriate attribution.
More from NBER
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .
© 2023 National Bureau of Economic Research. Periodical content may be reproduced freely with appropriate attribution.
- Share full article
Advertisement
Supported by
The Single Most Important Lesson From the 1918 Influenza
Tell the truth. At its core, society is based on trust.

By John M. Barry
Mr. Barry is the author of “The Great Influenza: The Story of the Deadliest Pandemic in History.”
In 1918, a new respiratory virus invaded the human population and killed between 50 million and 100 million people — adjusted for population, that would equal 220 million to 430 million people today. Late last year another new respiratory virus invaded the human population, and the reality of a pandemic is now upon us. Although clearly a serious threat to human health, it does not appear to be as deadly as the 1918 influenza pandemic. But it is far more lethal than 2009’s H1N1 (swine flu) pandemic, and the coronavirus does not resemble SARS, MERS or Ebola, all of which can be easily contained.
About 15 years ago, after yet another global contagion — the so-called bird flu — emerged in Asia, killing about 60 percent of the people it infected and threatening a catastrophic influenza pandemic, governments worldwide began to prepare for the worst. This effort included analyzing what happened in 1918 to identify public-health strategies to mitigate the impact of an outbreak. Since I had a historian’s knowledge of 1918 events, I was asked to serve on the initial working groups that recommended what became known as non-pharmaceutical interventions, that is, things to do when you don’t have drugs.
They involve only advice constantly reiterated today: social distancing, washing hands, coughing into elbows, staying home when sick. None alone provides great protection, but the hope was that if most people followed most of the advice most of the time, the interventions could significantly reduce the spread of the disease, or “flatten the curve,” a phrase now all too familiar. This may sound simple, but it is not. As with a diet, people know what to eat but often stray; here straying can kill.
As we begin employing these interventions now, we need to recognize what they can and cannot accomplish. Containment — the attempt to limit spread of a virus and even eliminate it — has failed. China has achieved far more than the most optimistic models predicted, but its initial slowness in responding allowed the virus to spread globally. Once that happened, the virus could not be stopped. Right now it is circulating invisibly in developed countries as well as in developing ones with little public-health infrastructure. That means it is here to stay and will constantly threaten to reinfect even countries that initially control it.
The United States is now in a phase of intervention labeled “suppression” by the infectious-disease expert Michael Osterholm: identifying infected people, isolating them, tracing contacts and asking contacts to self-quarantine. Because its incubation period is longer than influenza’s, Covid-19, caused by the coronavirus, allows that time. Whether we use that time well will determine whether a month from now the United States looks like Italy, where the virus seems out of control, or South Korea, which seems to have gained control by testing more than 270,000 of its 51 million people.
Right now virtually every state in America is in suppression mode, but suppression has no chance of succeeding unless cases are identified. With the United States having tested only about 40,000 of its nearly 330 million people — the worst record in the developed world — we are struggling to catch up, which will take weeks, all while the virus spreads, possibly so widely that it becomes entrenched and impossible to suppress. Nonetheless, suppression is worth trying because even partial success will slow the virus, giving us precious time to develop therapeutic drugs and vaccines.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
- Library of Congress
- Research Guides
- Newspapers & Current Periodicals
Influenza Epidemic of 1918 (Spanish Flu): Topics in Chronicling America
Search strategies & selected articles.
- Introduction
The links below provide access to a sampling of articles from historic newspapers that can be found in Chronicling America . You can further explore the topic of the "Influenza Epidemic of 1918 (Spanish Flu)" using the following search strategies:
- Use the following terms in combination, proximity, or as a phrase: Spanish influenza , Spanish flu , grip , la grippe , plague , epidemic , pandemic , Pfeiffer’s bacillus ( Pfelffer’s bacillus will also reveal results)
- It is important to use a specific date range if looking for articles for a particular event in order to narrow your results. The date range from 1918 to 1920 will yield the best results.
Selected Articles from Chronicling America
- "Epidemic of Grip and Pneumonia" The Ogden Standard (Ogden City, UT), May 8, 1918, 3:30 P.M. City Edition, Page 4, Image 4, col. 1.
- "Camp Dodge Leads in Health" The Tomahawk (White Earth, MN), June 27, 1918, Page 2, Image 2, col. 3.
- "Today: the Kaiser is Ill" The Washington Times (Washington, DC), July 11, 1918, Final Edition, Page 1, Image 1, col. 1.
- "Phipps Institute Identifies Germ of Spanish Grip" Evening Public Ledger (Philadelphia, PA), September 20, 1918, Page 1, Image 1, col. 1.
- "Influenza Claims Victim in Capital" The Washington Times (Washington, DC), September 21, 1918, Final Edition, Page 1, Image 1, col. 2.
- "Influenza Will Spread West, Is Belief" El Paso Herald (El Paso, TX), September 27, 1918, Home Edition, Page 1, Image 1, col. 6.
- "Medical Science's Newest Discoveries about the 'Spanish Influenza'" The Washington Times (Washington, DC), October 6, 1918, National Edition, Page 22, Image 22, col. 1.
- "'Spanish Influenza,' 'Three-Day-Fever,' and 'The Flu'" The Coconino Sun (Flagstaff, AZ), October 11, 1918, Page 1, Image 1, col. 3.
- "Uncle Sam's Advice on Flu" Nassau County Leader (Fernandina, FL), October 18, 1918, Page 1, Image 1, col. 1.
- "Influenza Still Holds Sway Here" The Evening Herald (Klamath Falls, OR), November 7, 1918, Page 1, Image 1, col. 2.
- "Quarantine is Lifted" Pullman Herald (Pullman, WA), November 15, 1918, Page 1, Image 1, col 3.
- "Influenza and the Mask" The Logan Republican (Logan, UT), December 21, 1918, Page 1, Image 1, col. 3.
- "Spanish Influenza" The Ogden Standard (Ogden City, UT), February 9, 1920, Last Edition--4 pm, Page 9, Image 9, col. 5.
- << Previous: Introduction
- Last Updated: Aug 1, 2024 8:38 PM
- URL: https://guides.loc.gov/chronicling-america-spanish-flu
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- The Spanish influenza...
- The Spanish influenza pandemic seen through the BMJ’s eyes: observations and unanswered questions
The Spanish influenza pandemic seen through the BMJ ’s eyes: observations and unanswered questions
- Related content
- Peer review
- Tom Jefferson , researcher ,
- Eliana Ferroni , researcher
- 1 Acute Respiratory Infections Group, Cochrane Collaboration, Rome, Italy
- Correspondence to: T Jefferson jefferson.tom{at}gmail.com
Does the “Spanish flu” of 1918-9 have anything new to teach us about future pandemics? Tom Jefferson and Eliana Ferroni have investigated contemporary accounts in the BMJ archives to find out
Introduction
The great Spanish influenza of 1918-9 is perhaps the best known of all pandemics. A vast number of books have been written on the topic, and “Spanish flu” still represents a rich topic of discussion and research. 1 Although many scientific questions posed at the time have been answered by nearly a century of subsequent discoveries, some puzzles remain—such as the reason for the high case fatality rate (>2.5% according to some estimates), 2 the high incidence in young adults, 3 and the role played by the first world war and its aftermath. 4 At the time, the aetiology was not known and the disease’s mode of transmission could only be hypothesised by careful observation. In addition the effects of preventive measures remained largely unevaluated. A high number of descriptions of the event seem to be based on secondary sources—that is, they are not direct eyewitness accounts—although recently efforts to go back to primary sources have been made. 4
Reliance on secondary sources is a potential source of selection bias: the reader gets a selected view of events, and some of the contemporary observations and explanations are lost. Interpretation of events and actions of a bygone era from a modern perspective is another perilous activity.
We exploited the opportunity to consult the newly digitised BMJ archives to carry out a review of what was published at the time. We tried to look at the pandemic through the eyes of contemporary BMJ contributors and readers and give them their voice back. We chose the Spanish influenza pandemic because we believed some of the observations and issues raised at the time …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
Economic Synopses
What can we learn from the spanish flu pandemic of 1918-19 for covid-19.
The COVID-19 pandemic has spurred intense efforts among researchers to estimate the likely course of the pandemic and its economic effects. Several studies have sought insights from global pandemics of the past, including the Spanish flu pandemic of 1918-19, which is thought to have infected some 500 million persons, or about one-third of the world's population, and killed anywhere from 50 to 100 million people. 1 Lessons from the Spanish flu pandemic are relevant and informative. Like COVID-19, the Spanish flu was highly contagious; it was also unusually lethal compared with a typical seasonal flu. As the flu became more widespread and its dangers apparent, many cities sought to contain the virus by imposing restrictions on social and economic interactions. These efforts can provide insights about the economic and public health impacts of government efforts to limit the spread of pandemic diseases. This essay discusses some recent research findings on the effects of the Spanish flu pandemic and measures that cities took to control it.
The Spanish flu pandemic came in three waves beginning in the spring of 1918. The second wave, in the fall of 1918, was the largest by far in terms of total infections and deaths. A third wave occurred in the spring of 1919. Overall, the pandemic is estimated to have infected about 25 percent of the U.S. population, or about 25 million people, and killed 675,000 for roughly a 3 percent mortality rate. 2 The pandemic began during World War I, and the virus is thought to have been introduced and spread throughout the United States by soldiers returning from Europe. By the end of 1918, some 45,000 U.S. soldiers had contracted and died from the disease, a number only modestly smaller than the 53,000 American combat deaths. 3 As with typical seasonal flu, young children and the elderly were particularly susceptible to the Spanish flu. However, the Spanish flu was especially lethal for young, "prime-age" adults, especially men. In 1918, the mortality rate from the flu and pneumonia among men 15 to 34 years of age was more than 20 times higher than in previous years, and throughout the pandemic, half of all flu deaths were among adults between 20 and 40 years of age. Furthermore, the absolute risk of death from the flu was higher among those younger than 65 years of age than those 65 or older, with those younger than 65 accounting for 99 percent of excess flu deaths in 1918-19. 4 The high fatality rate among young adults, especially young adult men, is striking in comparison with both typical seasonal flu and COVID-19, where the case fatality rate has been far higher among the elderly than among the young. These differences in age-related fatality rates are one reason the economic impacts of the COVID-19 and Spanish flu pandemics might differ. The high fatality rate among prime-age males during the Spanish flu pandemic reduced labor supply and boosted real wage rates in locations where the incidence of the disease was high (Garret, 2009, and Correia et al., 2020). Such an effect seems unlikely from the COVID-19 pandemic. 5
As the COVID-19 pandemic spread across the United States, most state and local governments imposed restrictions on economic activity, such as requiring certain non-essential businesses to close or reduce their in-store services. Many firms have voluntarily reduced their operations to protect the health of their employees or because of weaker demand for their products. At the same time, many households have refrained from non-essential purchases and travel in an effort to protect themselves and to help limit the spread of the virus. To date these measures appear to have helped slow the pandemic and avoid overwhelming the health care system in most locations. However, aggregate economic activity and employment have declined sharply, leading many states and cities to ease restrictions even as COVID-19 cases and fatalities continue to rise.
A similar pattern played out during the Spanish flu pandemic. In an effort to stem the pandemic, many cities adopted measures such as closing schools and churches, prohibiting large gatherings of people, shutting down theaters and other entertainment venues, and temporarily closing non-essential businesses. 6 Several studies examine the effects of such non-pharmaceutical interventions (NPIs) on flu incidence and mortality rates. A general finding is that cities that put NPIs in place earlier or took more aggressive action had lower excess mortality rates, later peaks in caseloads and mortality, and, to a lesser extent, fewer total fatalities than cities that moved slowly or adopted fewer measures. 7 The experiences of Philadelphia and St. Louis are often compared. Philadelphia was slow to implement measures to stem the pandemic and experienced a surge in cases following a large parade in support of a Liberty Loan drive. St. Louis, by contrast, canceled a similar parade and took other measures soon after the first cases were reported. Philadelphia had among the highest mortality rates of any of the U.S. cities, with a peak weekly excess mortality rate of 250 deaths per 100,000 persons and a total pandemic mortality rate of 748 deaths per 100,000 persons. St. Louis had among the lowest rates of all major cities, with a peak weekly excess mortality rate of just 30 deaths per 100,000 persons and a total mortality rate of 358 deaths per 100,000 persons (Markel et al., 2007).
Most cities relaxed their measures after just a few weeks when flu deaths began to recede. However, many cities faced a surge in cases when measures were eased, which resulted in a second peak—often higher than the first—that led to reactivation of some NPIs (Bootsma and Ferguson, 2007, and Markel et al., 2007). The experience of St. Louis is a case in point. St. Louis's authorities moved quickly to close schools, churches, saloons, theaters, and other entertainment venues when the city's first cases appeared in early October. Businesses and factories were permitted to remain open, but business hours were reduced and police were dispatched to keep shoppers from lingering in stores. On November 9, the health commissioner ordered all non-essential stores and factories closed for four days, and cases peaked within days. Businesses were permitted to reopen on November 13 and schools opened on November 14. Flu cases continued to decline for the next two weeks but then began to climb sharply. The city closed schools again and reinstated a ban on all public gatherings. The second peak in cases—with a higher excess mortality rate than the first peak—was reached in December. Cases then began to decline and the city lifted all restrictions on businesses on December 28 and reopened schools on January 2. 8
The economic impacts of the flu pandemic and NPIs implemented to contain it are somewhat less clear than the epidemiological effects. Perhaps surprisingly, given the widespread incidence of illness and many deaths, the pandemic did not trigger a major contraction in aggregate economic activity. A mild recession began in September 1918 and continued to March 1919. Federal spending on the war effort might explain why the aggregate economy did not slow appreciably: "[T]he never-ending demand for coal, steel, machinery, textiles, and other products needed for the war effort largely offset the effects of such a severe pandemic on aggregate economic activity" (Benmelech and Frydman, 2020). Industrial production did fall sharply but recovered quickly. Retail sales appear to have been little affected by the pandemic, perhaps because of a surge in consumer purchases after Armistice on November 11, and neither business failures nor other forms of financial distress increased significantly. 9 The pandemic did have a large impact on some sectors, however—notably manufacturing. Correia et al. (2020) estimate that the pandemic caused an 18 percent decline in manufacturing output and a 23 percent decline in manufacturing employment, in part because several cities with large manufacturing industries were among those with the highest flu fatality rates.
Some NPIs, such as temporary closures of non-essential businesses, clearly impose direct economic costs on affected firms and households. However, widespread illness or deaths can also be economically costly, suggesting that, conceivably, the economic benefits of containing a pandemic might outweigh the direct costs imposed on owners and employees of firms that are required to close. During the Spanish flu pandemic, cities with lower excess flu mortality rates had smaller declines in some measures of economic activity, suggesting that the direct cost of NPIs might have been offset at least to some extent by stronger economies. Moreover, there is evidence that cities that imposed NPIs earlier and more rigorously during the pandemic had higher growth in manufacturing output and employment for up to four years after the pandemic. Correia et al. (2020) use a dynamic difference-in-difference regression approach to examine the impact of NPIs on manufacturing across cities. Their model controls for various pre-crisis state and local characteristics, such as total population, urbanization, manufacturing share of employment, and growth of manufacturing output and employment from 1909 to 1914. The study finds that implementing NPIs earlier in the pandemic and using them more intensely produced significantly higher rates of growth in manufacturing output and employment from 1919 to 1923 than did slower activation or less intense use of NPIs. Estimates from the study's base model indicate that a one standard deviation increase in the speed of adopting NPIs (8 days) is associated with 4 percent higher growth of employment after the pandemic, while a one standard deviation increase in NPI intensity leads to 6 percent higher employment growth. The authors estimate several models with different sets of controls, and though not all show a statistically significant impact of NPIs on growth or employment, none indicate that NPIs reduced economic activity. 10
Clearly, there are limits to the applicability of the Spanish flu episode to the COVID-19 pandemic. In particular, the unusually high fatality rate among young, working-age men suggests that the flu pandemic might have had a larger economic impact, particularly on labor-intensive industries, than will COVID-19. The structure of the U.S. economy and distribution of the population are also very different today than in 1918, which could affect how either a pandemic or the NPIs imposed to contain it affect public health or the economy. For example, because pandemic mortality is strongly associated with population density, increased urbanization suggests that NPIs might have more public health benefit today than in 1918. On the other hand, the substantial increase over time in employment in the service sector suggests that the direct costs of mandatory business closures, which tend to fall more heavily on retail establishments and other service industries, could be higher today than in 1918. 11 Still, insights from the Spanish flu and other pandemics should not be dismissed entirely. So long as we remain cognizant of the environmental features in which they occurred, the pandemics of the past can provide useful data points for helping to forecast how the COVID-19 and future pandemics are likely to play out, and in particular for addressing such questions as whether NPIs are likely to be the sole source of economic disruptions in a pandemic, or whether a pandemic would cause an economic downturn in the absence of interventions to slow its spread.
1 Johnson and Mueller (2002) estimate 50 million deaths worldwide and provide estimates for several countries. Jorda et al. (2020) report an estimate of 100 million deaths, as well as mortality estimates for other pandemics since the fourteenth century with at least 100,000 deaths.
2 Taubenberger and Morens (2006). See also Garrett (2008) and references therein for data and other information about the origins and spread of the pandemic in the United States.
3 Eric Durr, "Worldwide Flu Outbreak Killed 45,000 American Soldiers During World War I"; https://www.army.mil/article/210420/worldwide_flu_outbreak_killed_45000_american_soldiers_during_world_war_i .
4 Taubenberger and Morens (2006).
5 In a study of 15 major pandemics since the fourteenth century, Jorda, Singh, and Taylor (2020) find that real wages are typically elevated for several years after pandemics, while the returns to capital are low, likely because of widespread deaths among the working-age population.
6 Detailed information about the use of NPIs by 50 cities during the pandemic is available from the University of Michigan Center for the History of Medicine; http://chm.med.umich.edu/research/1918-influenza-digital-archive/ .
7 See Barro (2020), Correia et al. (2020), Bootsma and Ferguson (2007), Hatchett et al. (2007), and Markel et al. (2007). Barro (2020) notes that the mean duration of NPIs across 43 cities was 4-6 weeks and suggests that a duration of 12 weeks would have produced a substantially lower total death rate.
8 University of Michigan Center for the History of Medicine; https://www.influenzaarchive.org/cities/city-stlouis.html.
9 Velde (2020) examines a variety of high-frequency economic time series data during the pandemic and concludes that the pandemic had only modest impact on economic activity. Barro et al. (2020) examine the impact of the pandemic across countries and attempt to control for differences in war intensity using data on combat deaths. The study finds that the flu pandemic caused a 6.2 percent decline in GDP in a typical country and a decline of about 1.5 percent in the United States.
10 The base specification controls include measures of urbanization, pre-crisis population, manufacturing employment share, and flu mortality in 1917, as well as state-level agricultural employment share. Additional control variables in other specifications include the growth in manufacturing output and employment from 1909 to 1914, census region fixed effects, longitude, WWI servicemen mortality rate, and health and total public spending per capita in 1917.
11 In 1918, the U.S. population was split evenly between urban and rural areas in 1918, whereas today the urban population is five times the rural population. Moreover, in 1918, 33 percent of the labor force was employed in agriculture and 28 percent was employed in manufacturing, compared with 2 percent and 8 percent, respectively, today (Velde 2020). As of 2018, some 80 percent of the U.S. labor force was employed in service industries. See https://www.bls.gov/emp/tables/employment-by-major-industry-sector.htm.
Barro, Robert J. "Non-Pharmaceutical Interventions and Mortality in U.S. Cities During the Great Influenza Pandemic, 1918-1919." NBER Working Paper 27049, April 2020.
Barro, Robert J.; Ursua, Jose F. and Weng, Joanna. "The Coronavirus and the Great Influenza Pandemic—Lessons from the 'Spanish Flu' for the Coronavirus's Potential Effects on Mortality and Economic Activity." NBER Working Paper 26866, March 2020.
Benmelech, Efraim and Frydman, Carola. "The 1918 Influenza Did Not Kill the US Economy." VOX CEPR Policy Portal, April 29, 2020.
Bootsma, Martin C.J. and Ferguson, Neil M. "The Effect of Public Health Measures on the 1918 Influenza Pandemic in U.S. Cities." Proceedings of the National Academy of Sciences , May 2007, 104 (18), pp. 7588-93.
Correia, Sergio; Luck, Stephan and Verner, Emil. "Pandemics Depress the Economy, Public Heath Interventions Do Not: Evidence from the 1918 Flu." SSRN Working Paper No. 3561560, April 10, 2020.
Garrett, Thomas A. "Pandemic Economics: The 1918 Influenza and Its Modern-Day Implications." Federal Reserve Bank of St. Louis Review , March/April 2008, pp. 75-93.
Garrett, Thomas A. "War and Pestilence as Labor Market Shocks: U.S. Manufacturing Wage Growth 1914-1919." Economic Inquiry , October 2009, 47 (4), pp. 711-25.
Hatchett, Richard J.; Mecher, Carter E. and Lipsitch, Marc. "Public Health Interventions and Epidemic Intensity during the 1918 Influenza Pandemic." Proceedings of the National Academy of Sciences , May 2007, 104 (18), pp. 7582-87.
Johnson, Niall P.A.S. and Mueller, Juergen. "Updating the Accounts: Global Mortality of the 1918-1920 'Spanish' Influenza Pandemic." Bulletin of the History of Medicine , Spring 2002, 76 (1), pp. 105-15.
Jorda, Oscar; Singh, Sanjay R. and Taylor, Alan M. "Longer-Run Economic Consequences of Pandemics." Federal Reserve Bank of San Francisco Working Paper 2020-09, March 2020.
Markel, Howard; Lipman, Harvey B.; Navarro, J. Alexander; Sloan, Alexandra; Michalsen, Joseph R.; Stern, Alexandra Minna and Cetron, Martin S. "Nonpharmaceutical Interventions Implemented by U.S. Cities During the 1918-1919 Influenza Pandemic." Journal of the American Medical Association , 2007, 298 (6), pp. 644-54.
Taubenberger, Jeffery K. and Morens, David M. "1918 Influenza: the Mother of All Pandemics." Emerging Infectious Diseases , January 2006, 12 (1), pp. 15-22.
Velde, Francois R. "What Happened to the U.S. Economy During the 1918 Influenza Pandemic? A View Through High-Frequency Data." Federal Reserve Bank of Chicago Working Paper 2020-11, April 2020.
© 2020, Federal Reserve Bank of St. Louis. The views expressed are those of the author(s) and do not necessarily reflect official positions of the Federal Reserve Bank of St. Louis or the Federal Reserve System.
Cite this article
Subscribe to Our Newsletter
Stay current with brief essays, scholarly articles, data news, and other information about the economy from the Research Division of the St. Louis Fed.
SUBSCRIBE TO THE RESEARCH DIVISION NEWSLETTER
Research division.
- Legal and Privacy

One Federal Reserve Bank Plaza St. Louis, MO 63102
Information for Visitors

Influenza (“Spanish Flu” Pandemic, 1918-19)
By Thomas Wirth | Reader-Nominated Topic
As World War I drew to a close in November 1918, the influenza virus that took the lives of an estimated 50 million people worldwide in 1918 and 1919 began its deadly ascent. The United States had faced flu pandemic before, in 1889-90 for example, but the 1918 strain represented an altogether new and aggressive mutation that proved unusually resistant to human attempts to curb its lethality. The devastating effects of the virus, known today as H1N1, were first felt in late summer 1918 along the eastern seaboard in a military encampment outside of Boston. From there, influenza propagated ruthlessly across the country, claiming nearly 700,000 lives before running its course in the spring and summer of 1919.
The pandemic hit Philadelphia exceptionally hard after sailors, carrying the virus from Boston, arrived at the Philadelphia Navy Yard in early September 1918. In a city of almost two million people, a half a million or more contracted influenza over the next six months. Equally as startling, over 16,000 perished during this period, with an estimated 12,000 deaths occurring in little more than five weeks between late September and early November 1918. Historians and epidemiologists have identified several critical factors that shaped Philadelphia’s experience with influenza and help explain the peculiarly rapid and catastrophic spread of disease.
First, a severe shortage of medical personnel rendered the city partially defenseless against the pandemic. More than 25 percent of Philadelphia’s doctors, some 850 total, and an even greater share of its nurses were occupied with the war effort. In 1917 and 1918, three-quarters of the staff of Pennsylvania Hospital at Eighth and Spruce Streets was stationed at the Red Cross Base Hospital 10 in Le Tréport, France. Over two dozen physicians, fifty nurses, and nearly 200 aid workers with hospital training were called overseas, depriving the city of a skilled group of men and women on the eve of the pandemic. The absence of vital medical support made the difficult task of containing the flu and healing the sick even more challenging once the virus migrated from the military camps—including the Navy Yard, Camp Dix in New Jersey, and Camp Meade in Maryland—to the civilian population in late September.
Overcrowding’s Toll
The increased demand for labor during the war also compounded matters. While Philadelphia enjoyed a fantastic boom in employment in its shipbuilding, munitions, and steel industries, overcrowding turned the city’s well-documented but often ignored housing deficiencies into a legitimate public health crisis. As African American migrants from the Jim Crow South and immigrants from eastern and southern Europe fled their miserable circumstances in search of a better life, many found the opportunities gained in Philadelphia came at the price of their health and safety. Cramped, dilapidated, and unsanitary living quarters in places like the Seventh Ward —home to a third of the city’s African Americans in 1918—made the slums and tenement districts a fertile source for influenza.
If the city’s execrable living conditions and depleted medical corps made suppressing influenza difficult, its unabated proliferation in the fall of 1918 likely had its origins in the response of city health officials who drastically underestimated the flu’s potency. On September 21, just days after 600 sailors at the Navy Yard fell ill and the first civilian flu cases were confirmed, Philadelphia’s major newspapers reported that Dr. Paul A. Lewis of the Henry Phipps Institute at the University of Pennsylvania had determined the cause of the disease—a bacteria known as Pfeiffer’s B. influenzae. The Philadelphia Inquirer wrote that Lewis’s findings had now “armed the medical profession with absolute knowledge on which to base its campaign against the disease.”

The city’s top health administrators concurred and yet promptly contradicted their own best advice for staving off the grippe: avoid crowds. With virtually no resistance from the city’s leading public health officials at the Department of Public Health and Charities, a rally for the Fourth Liberty Loan Campaign brought 200,000 Philadelphians together into the city’s streets on September 28. A concert at Willow Grove Park featured the music of John Philip Sousa, stoking patriotic fire. Philadelphia raised $600 million in war bonds as a result, but this success immediately revealed a Faustian bargain. Within three days of the event, 635 new civilian cases of influenza signaled the beginning of the single most deadly period of pestilence ever recorded in the city’s history.
Influenza tore through Philadelphia at a ferocious pace in October and early November. During the second week of October 2,600 people succumbed to the flu, and the following week saw that number nearly double. Though the disease knew no gender, racial, or ethnic boundaries, infecting black and white men and women at an equally high rate, the city’s immigrant poor suffered hard. Those born of foreign parents in the Russian, Hungarian, and Italian communities, among others, died at a higher rate, with some 1,500 more total deaths than those born to American mothers. In a war time atmosphere on the eve of the Red Scare, immigrants were the primary target of inflamed nativist sentiment. Public health officials and private citizens alike scrutinized the personal hygiene habits of the foreign born and often linked insalubrious tendencies to the supposedly questionable morals associated with “alien” cultures. One “disgusted woman” wrote to the Public Ledger in October 1918 demanding that “don’t-spit signs be placed in our post-office building in all languages necessary, to reach all foreign men, and with fines for violations.” The city set fines for spitting at $2.50 and in one day, October 23, the Evening Bulletin reported 114 arrests.
Deluge of Corpses
As death stalked the city, unembalmed bodies piled up by the dozens in a lone morgue at Thirteenth and Wood Streets. The extreme circumstances of the pandemic also meant, however, that many bodies simply rotted for days in the streets. Eventually five makeshift morgues, including one at a cold-storage facility on Cambridge and Twentieth Streets, were established to meet the deluge of corpses. Cemeteries lacked the space and manpower to adequately bury the dead, too. At Holy Cross Cemetery in Lansdowne seminarians turned grave-diggers took in an average of 200 bodies a day in October and deposited hundreds of coffins into a large common grave. “On one occasion,” recalled Reverend Thomas C. Brennan of St. Charles Borromeo Seminary, “the students worked on this task until 10:30 p.m. by the light of the October full moon, the long rows of coffins in the trench presenting a weird and impressive picture in the moonlight.”
Those attempting to care for the living at Philadelphia General Hospital on Thirty-Fourth Street faced similarly overwhelming circumstances. Already at its capacity of 2,000 patients when the virus struck, the hospital had to find room for 1,400 more people as it peaked in mid-October. With hospitals inundated and facing a shortage of medical staff, volunteers were culled from religious organizations, civic associations, and, most prominently, the city’s medical and nursing schools. Across Philadelphia these men and women turned parish houses and armories into temporary emergency hospitals, but on the whole extra assistance remained scarce. As one volunteer recalled, “if you asked a neighbor for help, they wouldn’t do so because they weren’t taking any chances…It was a horror-stricken time.” And yet just as quickly did the horror arrive did it also depart. When 10,000 dosages of a flu vaccine finally arrived in Philadelphia on October 19, the virus was already in the beginning stages of a rapid decline. By the second week of November, deaths caused by influenza and pneumonia were less than a quarter of what they were the week prior, and by the end of the month the death toll had dipped under 100 for the week for the first time since early September. Still, the city’s death rate from influenza, at approximately 407 per 100,000 people, exceeded that of all other American cities in 1918.
Statistics such as these provide a tangible sense of the staggering loss of life that occurred in Philadelphia during this short period, though tell us next to nothing about how influenza inflicted widespread fear and distress across the city. For an instant in the fall of 1918 it was as if Philadelphia had been transported back to the fourteenth century to that grisly time when victims stricken with plague were often found dead within twenty four hours of contracting it. Perhaps the words of the renowned cardiologist Isaac Starr, a third-year medical student at the University of Pennsylvania at the time of the outbreak, came closest to encapsulating the ordeal of late 1918 when he noted simply that it was as if “the life of the city had almost stopped.”
Copyright 2011, University of Pennsylvania Press

Philadelphia Fights Back Against the Epidemic
Special Collections Research Center, Temple University Libraries
To combat the influenza epidemic, Philadelphia enacted an extensive anti-spitting ordinance. Practitioners were unclear about the cause of the flu, but they knew that it was an airborne disease and therefore instituted a public campaign against coughing, sneezing, and spitting in public. The Philadelphia Board of Health posted signs like this one in public places and inside public transport vehicles toward the end of 1918 and distributed pamphlets instructing citizens to use handkerchiefs while coughing. Several public places like churches, shops, and libraries closed, but most that remained open displayed such signs. The city’s ordinance made spitting a criminal offense – those found spitting without covering their mouths were fined $2.50 and sometimes even arrested.

Related Topics
- City of Medicine
- Greater Philadelphia
- Philadelphia and the World
Time Periods
- Twentieth Century to 1945
- South Philadelphia
- Children’s Aid Society of Pennsylvania
- Typhoid Fever and Filtered Water
- World War I
- Board of Health (Philadelphia)
- Philadelphia Navy Yard
- Infectious Diseases and Epidemics
- Coronaviruses
Related Reading
Barry, John M. The Great Influenza: The Epic Story of the Deadliest Plague in History . New York: Viking, 2004.
Brennan, Thomas C. “The Story of the Seminarians and their Relief Work during the Influenza Epidemic.” Records of the American Catholic Historical Society of Philadelphia 30 (2) (June, 1919): 115-177.
Crosby, Alfred W. America’s Forgotten Pandemic: The Influenza of 1918 . New York: Cambridge University Press, 1989.
Hardy, Charles. “ I Remember When: What Became of the Influenza Pandemic of 1918 .” Audio recording, January 18, 1983.
Starr, Isaac. “Influenza in 1918: Recollections of the Epidemic in Philadelphia.” Annals of Internal Medicine 85 (4) (October 1, 1976): 516-518.
Wirth, Thomas. “Urban Neglect: The Environment, Public Health, and Influenza in Philadelphia, 1915-1919,” Pennsylvania History 73 (Summer 2006): 316-42.
Related Collections
- Philadelphia Inquirer, North American, and Public Ledger Newspaper Collections Free Library of Philadelphia 1901 Vine Street, Philadelphia.
- Philadelphia Evening Bulletin newsclipping collection and the Housing Association of the Delaware Valley Records, 1908-1975 Urban Archives, Temple University Libraries 1900 N. Thirteenth Street, Philadelphia.
Related Places
Pennsylvania Hospital , 800 Spruce Street, Philadelphia.
Philadelphia Navy Yard , 5100 S. Broad Street, Philadelphia.
Backgrounders
Connecting Headlines with History
- Fear of the sick stranger (WHYY, November 4, 2014)
- Philadelphia News Coverage of the Epidemic (Influenza Encyclopedia, University of Michigan)
- Newspaper clipping, 1920: "Prohibition guards against influenza" (Drexel University College of Medicine Legacy Center)
- The Deadly Virus (National Archives Online Exhibit)
- American During the 1918 Influenza Epidemic (Exhibit, Digital Public Library of America)
Connecting the Past with the Present, Building Community, Creating a Legacy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.11(5); 2022 May
Comparison of public health measures taken during Spanish flu and COVID-19 pandemics: A Narrative Review
Sampada tambolkar.
1 Department of Pediatrics, Dr D.Y. Patil Medical College, Hospital and Research Center and Dr. D.Y. Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India
Manas Pustake
2 Department of Internal Medicine, Grant Government Medical College and Sir J. J Group of Hospitals, Mumbai, Maharashtra, India
Purushottam Giri
3 Department of Community Medicine, IIMSR Medical College, Badnapur Dist. Jalna, Maharashtra, India
Isha Tambolkar
4 Department of Community Medicine, Byramjee Jeejeebhoy Government Medical College and Sassoon General Hospital, Pune, Maharashtra, India
The similarity of the consequences of COVID-19 reminded us of the destruction caused by the Spanish flu over a century ago and led us to find similarities in the way the two pandemics were handled. PRISMA Guideline was followed for a systematic search to identify eligible published articles. Information about the public health measures adopted during both the pandemics was taken from literature. It was found that there are parallels between the two pandemics in terms of general unpreparedness, attitudes of the community and government, and various policy issues. All the measures implemented in 2020 were the same as those implemented in 1918–1919, with the same trend, uncertainty, early relaxing, and rapid reversals. Even from a scientific standpoint, all the elements were already known. All the issues such as social isolation, intra-family spread, personal protective equipment, medicine types (quinine, aspirin, anti-inflammatories, etc.), immunization requirements, and so on had already been addressed. No doubt, we do have technology today at our disposal for managing the spread of the disease and even spread awareness among people much easily. We also have taken many steps forward in the world of globalization, which make the progression and spread of the pandemic very fast as well. Both factors tend to counter each other and hence make timely public health intervention as important (if not more) today as it was yesterday. When possible, approaches and goals should be found on scientific facts and include ethical input. Finally, we must take careful notice of past local and national lessons to avoid repeating the mistakes done in the past. The development of a strategy ahead of time that includes all levels of government health infrastructure and outlines clear lines of duties and functions is critical. The main objective of this article was to compare the public health measures undertaken during the pandemic of Spanish Flu and the pandemic of COVID-19, and assess the similarities and differences in the public health measures taken during these pandemics. The correlation of the public health measures and the outcomes was assessed and the implication of this article was to be pandemic-ready in the future.
Introduction
The world Health Organization (WHO) declared the COVID-19 outbreak as a public health emergency of worldwide concern on January 30, 2020, and began classifying it as a pandemic in March 2020 to highlight the seriousness of the situation and to urge all governments to take action in detecting illness and preventing spread. The announcement made by WHO on March 7, 2020, “Responding to community spread of COVID-19,” states that preventing COVID-19 from spreading is through the development of coordination mechanisms not only in health, but also in areas such as transportation, travel, commerce, finance, security, and other sectors that encompasses the entirety of society.[ 1 ] The consequences of the disease reminded us of the destruction caused by the Spanish flu over a century ago and led us to find similarities in the way the two pandemics were handled. The Spanish Flu of 1918–19 was the deadliest pandemic in history, killing more than 50 million people. Even as we deal with the current pandemic of COVID-19, the public health implications of the Spanish flu pandemic remain unclear.[ 2 ]
In the absence of a vaccine, public health interventions are the first line of protection against an outbreak. This can be attributed to the fact that globalization, urbanization, and the increase in the density of population have made controlling a pandemic difficult.[ 3 ] Every variant of the virus will not have a vaccine and public health interventions assume paramount importance in such conditions. Implementation of these interventions need to be done at grassroot levels. The role of primary health care centers, family physicians, and general practitioners is significant in these situations. This review article focuses on and compares the public health measures undertaken during the pandemics of Spanish Flu and COVID-19, and also discusses relevant updates in the pandemic preparedness strategy to attenuate the effects of pandemics in the future.
The following measures are currently being used to handle pandemics:
Social distancing
The goal of social distancing is to decrease interactions between people in a larger population where individuals may be contagious but haven’t been detected and hence not isolated, particularly important when the disease spreads due to close contact.[ 4 ] This is not limited to maintaining a safe distance while in public. It includes closing schools, colleges, offices, avoiding public gatherings, and measures like encouraging online shopping instead of physically going to the market.[ 5 ] Traffic restrictions, the cancellation of social events, and home quarantine have all been linked to a decrease in the degree of transmission.[ 6 ]
Quarantine is the restriction of activities or separation of persons who are not unwell, but may have been exposed to an infectious agent or disease, with the goal of monitoring their symptoms and guaranteeing early diagnosis of cases. Quarantine itself comes from the Italian word ‘Quaranta,’ which means forty. This is because, ships coming at the Venice port in fourteenth-century Italy from other plague-infected ports had to anchor and wait for 40 days before disembarking their surviving passengers, which was a common public health norm.[ 5 ] Prior research states that quarantine is the most efficient approach for reducing both the number of infected and the number of deceased.[ 6 , 7 ] To ensure success, quarantine should be implemented as soon as possible and combined with other public health initiatives.[ 8 ]
Isolation is the exclusion of sick people with infectious diseases from non-infected people to protect the latter group. It is most commonly seen in hospitals.[ 4 ] Isolation of the infected people helps in slowing down the transmission of the disease.
Use of face masks
The purpose of the face mask is to prevent transmission of the virus by containing the secretions of the people.[ 5 ] Face masks should be used in the community in addition to, not instead of, other prevention measures including physical separation, staying home while sick, respiratory etiquette, meticulous hand hygiene, and avoiding touching the face, nose, eyes, and mouth.[ 9 ]
If these steps are deemed inadequate, ‘community-wide containment’ might be necessary. Community-wide containment is a strategy for reducing personal interactions in a community, area, or country, except allowing limited contacts to ensure essential supplies.[ 4 ] This community-wide containment took place in India as the Janata Curfew and the Lockdown in India in the initial days of the spread of the disease. Mass quarantining of disease “hot spots” could be implemented to prevent the disease from spreading to other areas in future waves.[ 10 ] This was also implemented in India in the form of micro-containment zones and containment areas. Mass communication and community education through various media was promoted, which supplemented the aforementioned measures.[ 11 ]
Public Health Measures taken during Spanish Flu Pandemic
The 1918 influenza epidemic was a major social and health event that resulted in a high rate of morbidity and mortality in the general population. The fast onset of symptoms, the spread to large groups of people, and the lack of information about the causal agent were all factors that combined to make the flu a serious public health problem.[ 12 ] The importance of quarantine as a public health measure was strongly proven during the influenza pandemic of 1918.[ 13 ] The most prominent example comes from the United States, in Philadelphia, where the first case was discovered on September 17, but societal measures to limit the spread, such as restricting crowds in public locations, were implemented on October 3, when there were 40 deaths per 100,000 people. Unfortunately, the subsequent steps were ineffective, and by the middle of October, the number had risen to 250/100,000 persons. In St. Louis, Missouri, the first case was discovered on October 5, and social restrictions were imposed on October 7, and both the number of patients and the rate of mortality were kept low.[ 5 ] Another interesting example comes from Milan where the then Head Physician of the Municipality proposed some public health measures to prevent the spread of disease. In Milan, murmurs of Spanish influenza prompted Guido Bordoni Uffreduzzi (1859–1943), the Municipality’s chief physician, to intervene. On a collective basis, it was suggested to isolate the sick, to avoid overcrowding, especially in communities and the surroundings. Individually, it was suggested that people avoid unnecessary contact with the sick and convalescents, as well as unnecessary travel while attempting to maintain daily routines as much as possible. It was suggested that people wash their hands multiple times a day and use a moderately acting disinfectant mouthwash to safeguard their oropharynx.[ 14 ]
The simplest of treatments, such as the abundance of air in the environment where the sufferers are located, were thought to have a positive outcome and were implemented.[ 15 ] The study submitted by the Committee formed by the Paris Medical Academy for the prophylaxis of influenza was mentioned in the BMJ of November 2, 1918. They include personal hygiene measures such as mouth washing and gargling twice a day with a glass of warm water containing a solution of chlorine soda, as well as population-related measures such as overcrowding prevention, tramway and railway carriage washing and disinfection, and school closure.[ 16 ] Another unique measure was put in place at St Paul: Elevators were no longer authorized in buildings with fewer than six floors. Due to the close confines and lack of fresh air, elevators were deemed as areas where influenza may quickly spread.[ 17 ] Sanitation laws were enacted, which required restaurants and bars to sterilize their plates and cups, as well as prohibit roller towels and common drinking glasses in public restrooms. A health teaching campaign involving school teachers (who were out of work), postal workers, and Boy Scouts was also held.[ 18 ] Nurses too played a central role in the management of the pandemic. Retired nurses were called back to lend their help in the handling of the pandemic. New spaces were opened up for the sufferers of the disease.[ 19 ]
Finally, summing up the major public health measures, as analyzed by newspapers back in the day, we can say that measures such as the closure of schools and postponement of the start of the academic year, disinfection of facilities, quarantines, isolation, suspension of public celebrations, disinfection and hygiene, border control, suspension of railway communications, and the development and use of various vaccinations and serums to immunize the people were adopted; plasma was also termed to be an effective measure for the treatment of Spanish Flu-caused-pneumonia.[ 20 ] The spread of Spanish flu was slowed by identifying suspicious cases through surveillance and voluntary and/or enforced quarantine or isolation. Because no vaccinations or antivirals were available at the time, these public health initiatives were the only effective weapons against the disease.[ 21 ] Local health departments implemented public health interventions such as providing free soap and clean water to the poor; services for the removal of human waste, the inspection of milk and other food products; prohibiting spitting in the street, which slowed the spread of pocket spittoons; and newspaper and leaflet advertisements touting the therapeutic benefits of water.
Public Health Measures taken during COVID-19 Pandemic
In general, preventive measures in terms of community medicine consumed are voluntary or self-quarantine, mandatory quarantine, hand hygiene, isolation, personal protective equipment, school measures/closures, social distancing, workplace measures/closures.[ 5 ] After the implementation of multifaceted public health measures (including but not limited to intensive intracity and intercity traffic restriction, social distancing measures, home confinement and centralized quarantine, and improvement of medical care) in Wuhan, the number of incident COVID-19 cases were reduced, and the situation was under better control.[ 6 ] India also has put stringent measures such as a lockdown in place to manage the pandemic. India took a technological, social, and legislative approach, which was instrumental in flattening the curve of the disease in the early stages.[ 22 ] However, Sweden has adopted a surprising approach to the pandemic. It looks to be a significant outlier in its public health policy by imposing only very minimal mandates—closure of high schools and colleges alone and prescribing isolation for symptomatic persons and those over 70 years old.[ 23 ] Singapore adopted a resource-intensive containment effort based on the symptoms and travel history of suspicious patients. Despite this cost-containment effort, it was recognized that some COVID-19 individuals with little symptoms might be admitted to the general ward at first. As a result, our hospital prioritized social distancing initiatives across the board.[ 24 ] Some countries have had the best success because they adopted early restrictions and robust testing measures. For instance, New Zealand adopted a “go hard, go early” approach, in which the government responded quickly to signals of community spread.[ 25 ] Despite an early epidemic, South Korea was able to flatten the curve by thorough testing, contact tracing, and widespread mask use. Even in a single country, state policies have varied, which ultimately led to a variation in the number of cases. For instance, different states in the United States of America have responded differently to the pandemic. Outbreaks have been comparatively less in states like New York that have made greater attempts to contain the virus as compared to states like North Dakota, which did little to control the spread of the disease initially.[ 25 ] Although convalescent plasma has been shown to be effective in the treatment of several viral infections in the past, its application in the context of COVID-19 is still controversial.[ 20 ] In fact, the Indian Council of Medical Research has dropped plasma therapy from COVID-19 Management Guidelines.
What Changed and What did not Change: A Comparison of Approaches
There are parallels between the two pandemics in terms of general unpreparedness, attitudes of the community and government, and various methods. All the measures to be implemented in 2020 are the same as those implemented in 1918–1919, with the same trend, uncertainty, early relaxing, and rapid reversals. Even from a scientific standpoint, all the elements (such as social isolation, intra-family spread, personal protective equipment, etc) were already known.[ 14 ] No doubt, we do have the technology today at our disposal for managing the spread of the disease and even spread awareness among people much easier. We also have taken many steps forward in the world of globalization, which makes the progression and spread of the pandemic very fast as well. Both factors tend to counter each other and hence make timely public health intervention as important (if not more) today as it was yesterday. A difference in the testing facilities is also present between the two pandemics. Testing was not available during the deadly Spanish Flu pandemic because we didn’t know what caused it at the time.[ 26 ] The major difference between the two pandemics has been the development of vaccines. Researchers attempted to produce a vaccine during the 1918–1919 pandemic. A number of vaccinations were investigated against Bacillus influenzae (now known as Hemophilus influenzae), as well as pneumococcus, streptococcus, staphylococcus, and Moraxella catarrhalis bacteria. These bacterial vaccinations had little chance of preventing the pandemic, which was caused by a novel strain of the influenza A virus, as we now know.[ 27 ]
On the contrary, the development of a vaccine for the COVID-19 pandemic was in fact a race against time. Within a year and a half of the commencement of the pandemic, India fast-tracked the approval of three COVID-19 vaccinations: Covishield from the Serum Institute in Pune, Covaxin from Bharat Biotech, and Sputnik V, a Russian vaccine. Countries all over the world have started full-fledged vaccination drives. Israel was the first country to demonstrate that vaccines had a widespread impact. The U.S. has administered 89.3 doses for every 100 people.[ 28 ] Another major difference between the two pandemics was that the health education and awareness platforms have been enormous during the recent pandemic, considering that it is the age of social media. Press was the only source of widespread information dissemination during the Spanish flu pandemic. Today, the public health and hygiene measures can reach far and relatively inaccessible areas very easily; but the downside was, it also spread rumors and panic very fast. Another aspect of technology during this pandemic was that the development of Apps like the Arogya Setu App made contact tracing efficient and fast, greatly reducing disease transmission. Also, the App showed the availability of hospital beds and oxygen beds for patients to be admitted. In addition, this pandemic of 2020 had the boon of technology, when home-based care and treatment were possible without physical consultation due to telephonic and video consultation. Concepts of telemedicine and e-consultation have flourished and have had numerous benefits during these tough times. All of this technological assistance was certainly not in place during the Spanish-flu outbreak. Figure 1 compares the availability of health related resources during the COVID-19 pandemic and the Spanish Flu pandemic.

Comparison of availability of resources during the COVID-19 pandemic and the Spanish Flu pandemic.
Conclusions
The choice of strategy should be region-specific and factors like compliance of the population and awareness among the public are some factors that will influence the strategy chosen for a region. Periodic assessment and revision of the strategy will prove beneficial over a longer duration. Public health should be put above social and economic concerns. Finally, ‘such measures can be reduced’ is an issue that demands more research. Patterns in the timing and severity of second waves in 1918, however, appear to have significant implications. This means that till we have an effective vaccine in hand, we need to deploy efficient pharmaceutical interventions to keep the pandemic under control. Finally, every country and government should be ready for any medical emergency and be able to handle it efficiently by getting their priorities right. This is especially applicable to primary healthcare providers who are the first point of contact for many patients. Their role becomes even more significant and important when we aim to spread awareness and ensure the interventions reach the grassroot level. The general physicians are the link between the public health policy and the public. They should be made aware of the intricacies of pandemic management and interventions so that they can effectively disseminate the information. This will only strengthen our healthcare system as community medicine forms the core of any healthcare system.
Recommendations
When possible, approaches and goals should be founded on scientific facts and include ethical input. Finally, we must take careful notice of past local and national lessons in order to avoid repeating the mistakes done in the past. The development of a strategy ahead of time that includes all levels of government health infrastructure is critical. Stakeholders must be consulted on surge capacity and community containment plans, and an agreement must be reached. The healthcare systems are generally overwhelmed at the peak of a pandemic. Therefore, it is important to analyze as to what extent we would require a particular healthcare intervention and enhance its production in the nascent stages of the pandemic. It is also important to have an additional buffer of healthcare staff that could potentially reduce the burden on the frontline medical staff at the height of the pandemic. Family physicians having adequate medical knowledge can be trained in pandemic management per se , and they will be the best additional buffers. They could be trained to work in the hospitals or in special departments like the Emergency Department, Intensive Care Unit, and so on and will be a formidable buffer during pandemics. Thus, it will reduce the chances of having overburdened healthcare workers.
- There are parallels between the two pandemics in terms of general unpreparedness, attitudes of the community and government, and various methods.
- The major differences between the two pandemics has been the development of vaccines and availability of technology (apps like Arogya Setu app, e-consultation, etc).
- We do have the technology today at our disposal for managing the spread of the disease and spreading awareness among people much easier, but we also have taken many steps forward in the world of globalization, which makes the progression of the pandemic very fast as well. Both factors tend to counter each other and hence make timely public health intervention very important.
- The general physicians are the link between the public health policy and the public. They should be made aware of the intricacies of pandemic management and interventions so that they can effectively disseminate the information.
- It is also important to have an additional buffer of healthcare staff (trained family physicians) who could potentially reduce the burden on the frontline medical staff at the height of the pandemic.
Ethical considerations
No human or animal participants were involved in the study. Ethical approval was not required for this study.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

COMMENTS
Spanish Flu - Symptoms, How It Began & Ended
The Spanish Influenza Pandemic: a lesson from history ...
The Flu Pandemic of 1918
Here are 10 facts about the 1918 Spanish flu. 1. It struck in three waves across the world. Three pandemic waves: weekly combined influenza and pneumonia mortality, United Kingdom, 1918-1919 (Credit: Centers for Disease Control and Prevention).
The 1918 Flu Pandemic: Why It Matters 100 Years Later
Influenza pandemic of 1918-19 | Cause, Origin, & Spread
The Spanish flu: The global impact of the largest influenza ...
The 1918 "Spanish flu" pandemic was caused by a founder H1N1 influenza A virus. The three subsequent pandemics of 1957, 1968, and 2009 (black arrows) were caused by descendants of the 1918 virus, which acquired one or more genes through reassortment . Colored horizontal lines reflect the years of annual epidemics of seasonal influenza that ...
Abstract. 2018 marks the 100-year anniversary of the 1918 influenza pandemic, which killed ~50 million people worldwide. The severity of this pandemic resulted from a complex interplay between viral, host, and societal factors. Here, we review the viral, genetic and immune factors that contributed to the severity of the 1918 pandemic and ...
The Spanish Flu Was Deadlier Than WWI. Historians aren't actually sure where the 1918 flu strain began, but the first recorded cases were at a U.S. Army camp in Kansas in March 1918. By the end ...
1. INTRODUCTION. A century ago, an influenza‐A virus caused the greatest pandemic in human history, the "Spanish Flu." It infected about a third of the world population and caused an estimated 50-100 million victims (Johnson & Mueller, 2002; Taubenberger & Morens, 2006).The long‐term effects of the Spanish Flu went well beyond the immediate demographic losses that it caused.
Social and Economic Impacts of the 1918 Influenza Epidemic
The Single Most Important Lesson From the 1918 Influenza. Tell the truth. At its core, society is based on trust. Mr. Barry is the author of "The Great Influenza: The Story of the Deadliest ...
Influenza Epidemic of 1918 (Spanish Flu): Topics in ...
Decent Essays. 485 Words. 2 Pages. Open Document. To say that the flu of 1918 (The Spanish flu) was huge would be an understatement. Over the course of two years this flu killed millions of people not only in the United States but a total of five hundred million people worldwide. The flu is caused by the infectious types of the Influenza virus ...
Open Document. The Spanish Flu was a world wide epidemic that took the lives of an estimated 50 to 100 million lives between 1918 and 1920. It has been recorded as the most devastating outbreak in world history. The disease first appeared in Fort Riley Kansas on March 11, 1918 when an Army private reported to the camp hospital with complaints ...
Introduction. The great Spanish influenza of 1918-9 is perhaps the best known of all pandemics. A vast number of books have been written on the topic, and "Spanish flu" still represents a rich topic of discussion and research.1 Although many scientific questions posed at the time have been answered by nearly a century of subsequent discoveries, some puzzles remain—such as the reason for ...
While the 1918 influenza killed a disproportionate number of 25-40 year olds, COVID-19 mostly affects those over the age of 65, especially those also with comorbidities. 2 5 In particular, the mortality rate for the influenza rose to 8%-10% for younger people compared with a 2.5% overall mortality whereas the mortality rate for the 25-40 ...
The Spanish flu pandemic came in three waves beginning in the spring of 1918. The second wave, in the fall of 1918, was the largest by far in terms of total infections and deaths. A third wave occurred in the spring of 1919. Overall, the pandemic is estimated to have infected about 25 percent of the U.S. population, or about 25 million people ...
The essay below invites the reader to reflect back in time from a different perspective—from that of the artist and from those of us who behold and appreciate art—and to consider ways in which a terrible pandemic from a century ago foreshadows our current situation. ... Self-Portrait After the Spanish Flu. 1919-20. Oil on Canvas. 23 × 29 ...
Influenza ("Spanish Flu" Pandemic, 1918-19) As World War I drew to a close in November 1918, the influenza virus that took the lives of an estimated 50 million people worldwide in 1918 and 1919 began its deadly ascent. The United States had faced flu pandemic before, in 1889-90 for example, but the 1918 strain represented an altogether new ...
The Spanish Flu of 1918-19 was the deadliest pandemic in history, killing more than 50 million people. Even as we deal with the current pandemic of COVID-19, the public health implications of the Spanish flu pandemic remain unclear. In the absence of a vaccine, public health interventions are the first line of protection against an outbreak.