| Johns Hopkins Fetal Skull Collection (1918–1951) - | | | | | Specimen | Schultz Number | Schultz Number (Old) | Sex | Race | Ted Combs Age 1 | Ted Combs Age 2 | Ted Combs Notes | | JH 001 | 6 | Blank | | B | 5-6 | IU | Left Occipital Condyle Missing 7/01 JR | | JH 002 | 15 | 253 | | B | 7 | IU | | | JH 003 | 18 | Blank | | B | 11 | PN | LEFT GREATER WING MAY HAVE BEEN BROKEN | | JH 004 | 34 | 394 | | B | 12 | PN | ENTIRE BASICRANIUM FUSED | | JH 005 | 35 | 361 | | B | 10 | IU | | | JH 006 | 36 | 258 | | B | 7 | IU | ADOLF H SCHULTZ DRAWING INCLUDED | | JH 007 | 38 | 269 | | B | 10-11 | IU | IMPROPER OSSIFICATION OF DORSUM STELLA | | JH 008 | 51 | Blank | | B | 5 | IU | NOT ALL BONES BELONG HERE | | JH 009 | 56 | 271 | | B | 10 | IU | | | JH 010 | 58 | 340 | | B | 9-10 | IU | | | JH 011 | 62 | Blank | | B | 0 | Newborn | | | JH 012 | 67 | 322 | | B | 0 | Newborn | MOLAR BUDS INCLUDED | | JH 013 | 69 | 299 | ? | B | 9 | IU | CHECK SEX | | JH 014 | 71 | 323 | | B | 0 | Newborn | | | JH 015 | 78 | 298 | | B | 8 | IU | IMPROPER OSSIFICATION OF THE STELLA TURCICA | | JH 016 | 83 | Blank | | B | 7 | IU | | | JH 017 | 91 | 334 | | B | 10 | IU | | | JH 018 | 96 | 310 | | B | 10 | IU | SQUAMOUS PORTION OF OCCIPITAL IN 2 PIECES | | JH 019 | 109 | 315 | | B | 10 | IU | EXTRA BROKEN MALLEUS INCLUDED | | JH 020 | 110 | 257 | | B | 6 | IU | TEMPORALS POORLY OSSIFIED | | JH 021 | 111 | 342 | | B | 3 | PN | | | JH 022 | 126 | 367 | | B | 10 | IU | | | JH 023 | 135 | 250 | | B | 8 | IU | VERY YOUNG | | JH 024 | 137 | 285 | | B | 8 | IU | | | JH 025 | 139 | 400 | | B | 0 | Newborn | | | JH 026 | 144 | Blank | | B | 10 | IU | "Two right lateral occipital bones and no left JR 7/12/2001" | | JH 027 | 147 | 391 | | B | 2 | PN | LEFT FRONTAL IS THE ONLY BONE PRESENT. | | JH 028 | 155 | 355 | | B | 0 | Newborn | | | JH 029 | 159 | 273 | | B | 9 | IU | | | JH 030 | 161 | 367 | | B | 0 | Newborn | | | JH 031 | 164 | 359 | | B | 2 | PN | MANDIBLE ONCE FUSED, NOW BROKEN" | | JH 032 | 178 | 483 | | B | 15 | PN | OST OF BASICRANIUM FUSED | | JH 033 | 184 | 365 | | B | 2 | PN | | | JH 034 | 189 | 377 | | B | 3 | PN | | | JH 035 | 2 | 306 | | B | 0 | Newborn | MANDIBLE WAS FUSED: NOW BROKEN | | JH 036 | 8 | Blank | | B | 9 | IU | | | JH 037 | 14 | 236 | | B | 5 | IU | | | JH 038 | 17 | Blank | | B | 14 | PN | ADOLF H SCHULTZ DRAWING INCLUDED | | JH 039 | 44 | 298 | | B | 8 | IU | EXTRA MALLEUS | | JH 040 | 45 | Blank | | B | 0 | Newborn | POOR OSSIFICATION OF THE CALVARIA | | JH 041 | 53 | 440 | | B | 12 | PN | WHOLE SKULL BADLY OSSIFIED | | JH 042 | 57 | 366 | | B | 2 | PN | | | JH 043 | 59 | Blank | | B | 8 | IU | | | JH 044 | 61 | 340 | | B | 9 | IU | INCOMPLETE | | JH 045 | 63 | 340BUG!!! | | B | 12 | PN | TEETH BELONG TO JH 05. BAD BONE. | | JH 046 | 70 | 345 | | B | 3 | PN | | | JH 047 | 75 | 364 | | B | 0 | Newborn | | | JH 048 | 84 | Blank | | B | 8 | IU | | | JH 049 | 86 | 341 | | B | 2 | PN | | | JH 050 | 88 | 294 | | B | 8 | IU | | | JH 051 | 101 | 290 | | B | 8 | IU | | | JH 052 | 107 | Blank | | B | 8 | IU | | | JH 053 | 118 | 311 | | B | 9 | IU | NASAL BONES FUSED | | JH 054 | 120 | 252 | | B | 8 | IU | | | JH 055 | 121 | 276 | | B | 6 | IU | | | JH 056 | 122 | 313 | | B | ? | ? | TWO FRONTALS FROM TWO SPECIMENS (SIDES IN DISPUTE) EAR OSSICLES WITH SMALL....(?) | | JH 057 | 127 | 307 | | B | 10 | IU | | | JH 058 | 132 | 354 | | B | 4 | PN | | | JH 059 | 149 | 290 | | B | 8 | IU | | | JH 060 | 150 | 2825 | | B | See Note | See Note | Age estimated as 8 months to Newborn | | JH 061 | 169 | 340 | | B | 0 | Newborn | | | JH 062 | 172 | 283 | | B | 7 | IU | | | JH 063 | 185 | 345 | | B | 10 | IU | | | JH 064 | 190 | 331 | | B | 2 | PN | | | JH 065 | 191 | 256 | | B | 5-6 | IU | | | JH 066 | 10 | 240 | | W | 5 | IU | | | JH 067 | 20 | Blank | | W | 0 | Newborn | Reported missing by JR 7/001 | | JH 068 | 40 | Blank | | W | 2 | PN | | | JH 069 | 48 | 340 | | W | 7 | IU | | | JH 070 | 49 | 274 | | W | 6-7 | IU | | | JH 071 | 74 | 332 | | W | 10 | IU | | | JH 072 | 77 | 336 | | W | 10 | IU | | | JH 073 | 89 | 344 | | W | 9 | IU | | | JH 074 | 92 | 279 | | W | 6 | IU | | | JH 075 | 105 | Blank | | W | 6 | IU | | | JH 076 | 108 | 280 | | W | 9 | IU | | | JH 077 | 129 | 340 | | W | 1 | PN | | | JH 078 | 131 | 364 | | W | 9 | IU | | | JH 079 | 136 | 363 | | W | 9 | IU | | | JH 080 | 138 | 355 | | W | 3 | PN | KERKRING'S CENTER OBSERVED | | JH 081 | 141 | 347 | | W | 2 | PN | MANDIBLE ONCE FUSED NOW BROKEN | | JH 082 | 143 | 326 | | W | 0 | Newborn | EXTRA MALLEUS INCLUDED | | JH 083 | 146 | 320 | | W | 9 | IU | THREE PARIETAL FRAGMENTS | | JH 084 | 151 | 353 | | W | 3 | PN | | | JH 085 | 156 | 364 | | W | 2 | PN | | | JH 086 | 157 | 288 | | W | 8 | IU | | | JH 087 | 162 | 374 | | W | 9 | IU | | | JH 088 | 166 | 382 | | W | 4 | PN | MANY TOOTH FRAGMENTS | | JH 089 | 171 | 380 | | W | 10 | IU | NASAL BONES FUSED | | JH 090 | 179 | Blank | | W | 3 | PN | | | JH 091 | 186 | 373 | | W | 9 | IU | | | JH 092 | 188 | Blank | | W | 8 | IU | | | JH 093 | 192 | 328 | | W | 7 | IU | KERKRING'S CENTER OBSERVED | | JH 094 | 13 | Blank | | W | 0 | Newborn | TEETH FRAGMENTS | | JH 095 | 23 | 352 | | W | 4 | PN | TYMPANIC MEMBRANE INTACT | | JH 096 | 43 | 268 | | W | 5 | IU | ADOLF H SCHULTZ DRAWING INCLUDED | | JH 097 | 47 | 313 | | W | 8 | IU | ONE BONE FRAGMENT - SQUAMOUS TYPE | | JH 098 | 64 | 364 | | W | 3 | PN | | | JH 099 | 95 | 350 | | W | 4 | PN | HYDROCEPHALIC | | JH 100 | 100 | 365 | | W | 0 | Newborn | | | JH 101 | 114 | 396 | | W | 5 | PN | MANDIBLE ONCE FUSED NOW BROKEN | | JH 102 | 116 | 400 | | W | 2 | PN | TEETH NOT COUNTED | | JH 103 | 117 | 290 | | W | 7 | IU | TWO TOOTH BUDS | | JH 104 | 128 | 368 | | W | 5 | PN | TOOTH FRAGMENTS | | JH 105 | 134 | Blank | | W | 9 | IU | EAR OSSICLES PRESENT - NO COUNT | | JH 106 | 148 | 290 | | W | 8 | IU | EAR OSSICLES PRESENT - NO COUNT | | JH 107 | 160 | 60 | | W | 2 | PN | EAR OSSICLES PRESENT - NO COUNT | | JH 108 | 167 | 372 | | W | 1 | PN | EAR OSSICLES PRESENT - NO COUNT | | JH 109 | 168 | 316 | | W | 8 | IU | EAR OSSICLES PRESENT - NO COUNT | | JH 110 | 170 | 331 | | W | 0 | Newborn | EAR OSSICLES PRESENT - NO COUNT | | JH 111 | 175 | 342 | | W | 10 | IU | EAR OSSICLES PRESENT - NO COUNT | | JH 112 | 194 | 317 | | W | 8 | IU | | | (1918–1951) - The collection was begun by Adolph Hans Schultz (1891–1976) - fetal, stillbirths, newborns, and infants up to approximately one year of age. Collection of 112 specimens was transferred to the on a permanent loan in 1973. | | | | Macklin CC. . (1914) 16(3): 317-386. Macklin CC. . (1914) 16(3): 387-426. | - anterior fontanel - developing skull region that closes by about 20 months postnatally.
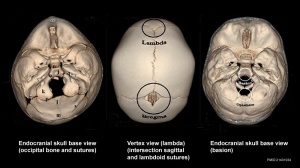
- basion - anatomical region on the basiocciput located at the midpoint between the anterior margin and posterior margin (opisthion) of the foramen magnum.
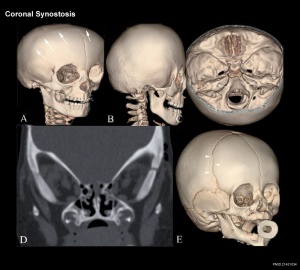
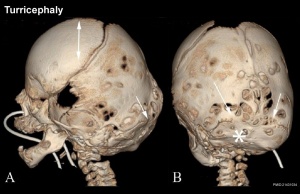
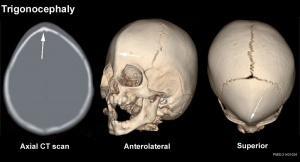
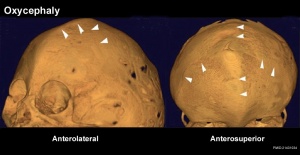
- compound craniosynostosis premature suture fusion involving two or more sutures.
- craniosynostosis - (craniostenosis) the premature fusion of cranial sutures.
- dermatocranium - (membranous) skull calvarial vault develops from intramembranous ossification.
- harlequin eye - a term used to describe the prominent bilateral elliptical orbits of the skull seen in brachycephaly.
- endochondral ossification - bone formation from a pre-existing cartilage template, such as the chondrocranium.
- intramembranous ossification - bone formation from a membrane where no pre-existing cartilage is found, such as the calvarial vault component.
- neurocranium - the portion of the skull that surrounds the brain. Ossification of bones in cranial base (endochondral) and vault (intramembranous).
- opisthion - anatomical region located on the occipital bone, located at the midpoint of the posterior margin of the foramen magnum.
- posterior fontanel - developing skull region that closes by about 3 months postnatally.
- primary craniosynostosis - an intrinsic defect in a suture.
- secondary craniosynostosis - premature closure of normal sutures due to systemic and metabolic (hyperthyroidism, hypercalcemia, hypophosphatasia, vitamin D deficiency, renal osteodystrophy, Hurler's Syndrome, sickle cell disease and thalassemia) and those that can affect brain growth.
- simple craniosynostosis - premature fusion involving only one suture.
- synostosis - premature fusion.
- viscerocranium - facial skeleton and some anterior neck structures.
External LinksExternal Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation. - PubMed Health Craniosynostosis
- Johns Hopkins Fetal Skull Collection (1918–1951) - collection was begun by Adolph Hans Schultz (1891–1976) - fetal, stillbirths, newborns, and infants up to approximately one year of age. Collection of 112 specimens was transferred to the Cleveland Museum of Natural History on a permanent loan in 1973.
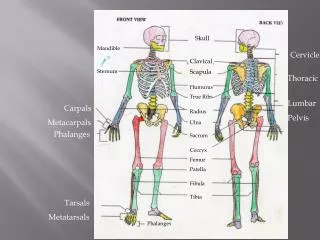
Glossary LinksCite this page: Hill, M.A. (2024, September 9) Embryology Musculoskeletal System - Skull Development . Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Musculoskeletal_System_-_Skull_Development - Musculoskeletal
- System Development
- Axial Skeleton
 - Success stories
- Spine and back
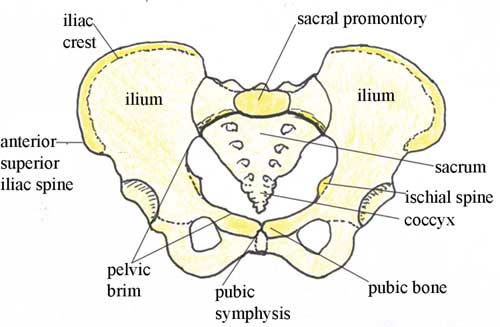
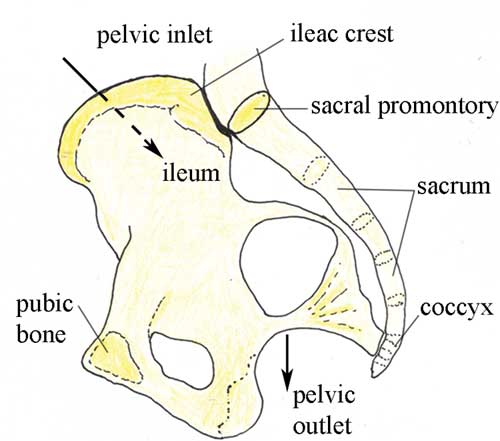
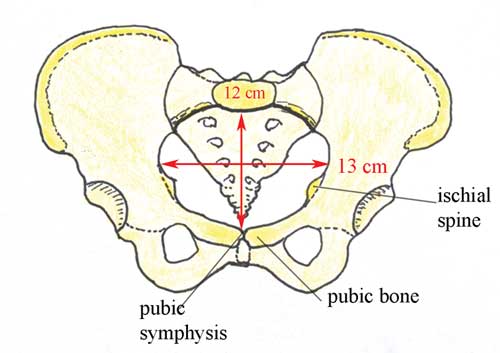
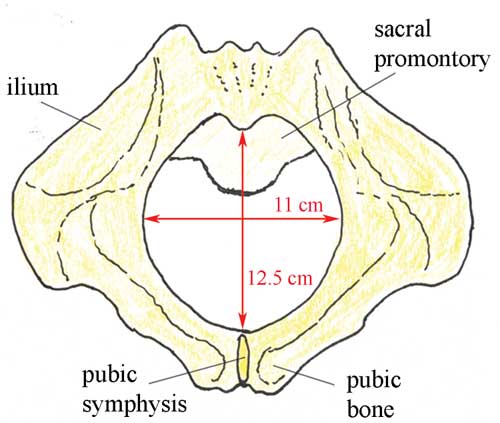
- Pelvis and perineum
- Head and neck
- Neuroanatomy
- Cross sections
- Radiological anatomy
- Types of tissues
- Body systems
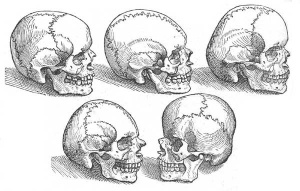
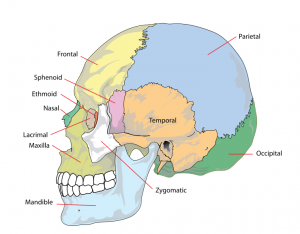
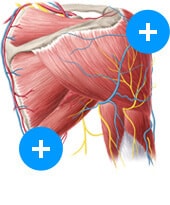
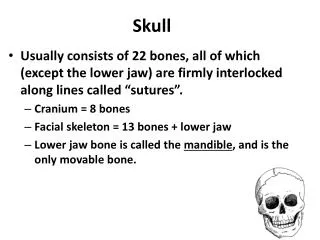
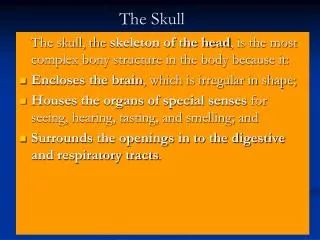
 Register now and grab your free ultimate anatomy study guide!  Development of the skullAuthor: Alexandra Sieroslawska, MD • Reviewer: Dimitrios Mytilinaios, MD, PhD Last reviewed: October 30, 2023 Reading time: 7 minutes /images/vimeo_thumbnails/258259549/TJabByIaQwCkhI4PujnhCQ_overlay.jpg) The skull is the most complex arrangement of bones within the body. It protects the central nervous system, the oral cavity and nasal cavity , the ears and the eyes within its inner, outer and directly related structures. Without this protective helmet, we humans would be ‘sitting ducks’, as the old phrase goes. This article will mention the most important aspects of the skull, taking into account its compilation of jigsaw like bones, its growth periods and their locations and its embryological derivatives. Embryological backgroundViscerocranium, fontanelles, neurocranium, clinical aspects. Lateral plate mesoderm found in the neck region, paraxial mesoderm and neural crest cells all contribute to the development and existence of the skull in its entirety. The bones of the skull are formed in two different ways; intramembranous ossification and endochondral ossification are responsible for creating compact cortical bone or spongy bone . During the maturation of the skull, it is categorically divided into two main parts: the viscerocranium and the neurocranium . These two terms account for the bones of the face and the bones of both the cranial base and the cranial vault respectively. The cranial vault is further divided into membranous neurocranium and cartilaginous neurocranium. :background_color(FFFFFF):format(jpeg)/images/library/7741/eEsfu70EOMx1TlBf5tYAiA_Go0bFvBvzClwSivuaiELg_head_01.png) The first part of the skull to be discussed is the viscerocranium or bones of the face. Below, they are grouped according to their derivative germ layer, their origins, their adult location and their way of ossifying. All the bones in this category are derived from cells of the neural crest . Also, all of the following structures emerge from the first and second pharyngeal arches . - The maxillary process from the first pharyngeal arch contributes to the formation of the maxilla , temporal bone , zygoma (zygomatic bone and arch) , the palatine bone , lacrimal bone , nasal bone , vomer and the inferior nasal concha. All of these bones ossify via intramembranous ossification , with exception of the inferior nasal concha , which uses endochondral ossification.
- The mandibular process which also emerges from the first pharyngeal arch produces the mandible via both intramembranous and endochondral ossification, the sphenomandibular ligament which is an exception as it is never ossified and finally the malleus and incus which are both ossified in an endochondral manner.
Meanwhile, the second pharyngeal arch produces the styloid process, the stapes and the hyoid bone, all of which are ossified endochondrally. The final structure is not ossified at all and is known as the stylohyoid ligament. The second and last item worth mentioning about the viscerocranium is the skull fontanelles . These are the growth areas of the skull that are present since before birth up until certain ages in young children. Here is a list of the location of these areas and the time period in a child’s life in which they close: - The anterior fontanelle known as bregma closes between four and twenty six months. It is a diamond-shaped space located between the paired frontal and parietal bones of the fetal/neonatal skull (also described as the junction of the coronal and sagittal sutures).
- The posterior fontanelle known as lambda closes much earlier than the anterior, at only one to two months after birth. It is located where the two parietal bones meet the occipital bone (also described as the junction of the sagittal and lambdoid sutures ).
- The sphenoidal fontanelle (also known as the anterolateral fontanelle) closes between two and three months and is called pterion. It is located at the junction of the sphenoid, parietal, temporal, and frontal bones.
- The final fontanelle, which closes at twelve to eighteen months, takes its name from the area in which it is situated, the mastoid fontanelle , otherwise known as the asterion fontanelle. It is located at the junciton of the temporal, occipital, and parietal bones.
:background_color(FFFFFF):format(jpeg)/images/library/7739/Yw9DFAjpeIjZu3iUn7UFxQ_RpHn9yFnfaSTgwdrVROMJQ_head_02.png) As previously mentioned, the neurocranium is further separated into the membranous neurocranium and the cartilaginous neurocranium . The structures within these subgroups are arranged according to the germ layer from which they arose, the area of the neurocranium in which they are situated, the adult structure they eventually become and finally the way in which they were ossified. - The membranous neurocranium consists of neural crest cells and paraxial mesoderm which form the main portion of the roof and lateral sides of the neurocranium. The neural crest cells create the adult frontal bone and squamous portion of the temporal bone . The paraxial mesoderm produces the intraparietal portion of the occipital bone and the parietal bone itself. All the structures undergo intramembranous ossification .
- The cartilaginous neurocranium is also made up of paraxial mesoderm and the cells of the neural crest . The neural crest maintains the development of the prechordal neurocranium anterior to the sella turcica. Meanwhile, the paraxial mesoderm is responsible for the growth of the chordal neurocranium, behind the sella turcica. The prechordal and chordal neurocranium mature into the ethmoid and sphenoid bones as well as the petrous and mastoid portion of the temporal bone and the occipital bone respectively. They all ossify via endochondral means.
Fractures of the skull occur at any age and are usually related to trauma by car crash, sports injuries and physical violence. However, the most dangerous age in which to be inflicted with such an ailment is between birth and twenty six months . It is a surprising discovery for many, due to the fact that babies have extremely flexible and soft bones compared to adults and one would think hitting their head wouldn’t crack the skeletal components. The reason for this increased risk is due to the fontanelles and the fact that they are open within this specific age gap. If one of the fontanelles is hit, brain trauma and internally bleeding can be almost certain. The layers of the fontanelles are that thin that a forceful trauma to that particular area would easily cause the object of contact to penetrate the open skull. References: - Neil S. Norton, Ph.D. and Frank H. Netter, MD, Netter’s Head and Neck Anatomy for Dentistry, 2nd Edition, Elsevier Saunders, Chapter 1 Development of the Head and Neck, Pages 10 to 12.
- T.W. Sadler, Langman’s Medical Embryology, 12th Edition, Wolters Kluwer: Lippincott, Williams and Wilkins, Part 2, Chapter 17 Head and Neck, Pages.
Illustrators: - Skull (ventral view) - Yousun Koh
- Skull (lateral view) - Yousun Koh
Development of the skull: want to learn more about it? Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster. What do you prefer to learn with? “I would honestly say that Kenhub cut my study time in half.” – Read more.  Learning anatomy isn't impossible. We're here to help. Learning anatomy is a massive undertaking, and we're here to help you pass with flying colours.  Want access to this video?- Curated learning paths created by our anatomy experts
- 1000s of high quality anatomy illustrations and articles
- Free 60 minute trial of Kenhub Premium!
...it takes less than 60 seconds!  Want access to this quiz?Want access to this gallery.  Anatomy of the Newborn Skull Although the skull appears to be 1 large bone, there are actually several major bones that are connected together. The major bones that compose the skull of a newborn include the following: 2 frontal bones 2 parietal bones 1 occipital bone These bony plates cover the brain and are held together by fibrous material called sutures. What are sutures?Sutures allow the bones to move during the birth process. They act like an expansion joint. This allows the bone to enlarge evenly as the brain grows and the skull expands. The result is a symmetrically shaped head. Some sutures extend to the forehead, while others extend to the sides and back of the skull. One suture in the middle of the skull extends from the front of the head to the back. The major sutures of the skull include the following: Metopic suture. This extends from the top of the head down the middle of the forehead, toward the nose. The 2 frontal bone plates meet at the metopic suture. Coronal suture. This extends from ear to ear. Each frontal bone plate meets with a parietal bone plate at the coronal suture. Sagittal suture. This extends from the front of the head to the back, down the middle of the top of the head. The 2 parietal bone plates meet at the sagittal suture. Lambdoid suture. This extends across the back of the head. Each parietal bone plate meets the occipital bone plate at the lambdoid suture. If any of the sutures close too early (fuse prematurely), there may be no growth in that area. This may force growth to happen in another area or direction. This results in an abnormal head shape (craniosynostosis). What are fontanelles?There are 2 fontanelles (the space between the bones of an infant's skull where the sutures intersect) that are covered by tough membranes that protect the underlying soft tissues and brain. The fontanelles include: Anterior fontanelle (also called soft spot). This is the junction where the 2 frontal and 2 parietal bones meet. The anterior fontanelle remains soft until about 18 months to 2 years of age. Doctors can assess if there is increased intracranial pressure by feeling the anterior fontanelle. Posterior fontanelle. This is the junction of the 2 parietal bones and the occipital bone. The posterior fontanelle usually closes first, before the anterior fontanelle, during the first several months of an infant's life. Related Links- Chiari Malformation Center
- Hydrocephalus Program
- Craniosynostosis (CRS): Overview
- Plagiocephaly
- Hydrocephalus
- Craniosynostosis
- Anatomy of the Skull Base
Related TopicsBasics About Your Newborn Baby's Body Assessments for Newborn Babies Connect with us: Download our App:  - Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health Warning: The NCBI web site requires JavaScript to function. more...  An official website of the United States government The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. - Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.  StatPearls [Internet].Delivery, face and brow presentation. Julija Makajeva ; Mohsina Ashraf . AffiliationsLast Update: January 9, 2023 . - Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the interprofessional team's role in safely managing delivery for both the mother and the baby. - Identify the mechanism of labor in the face and brow presentation.
- Differentiate potential maternal and fetal complications during the face and brow presentations.
- Evaluate different management approaches for the face and brow presentation.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference. Face presentation is an abnormal form of cephalic presentation where the presenting part is the mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3] In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation, with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3] Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, and black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, and polyhydramnios. [2] [4] [5] These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. Palpating orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation is possible. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, the anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse. Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] Ultrasound imaging can show a reduced angle between the occiput and the spine or the chin is separated from the chest. However, ultrasound does not provide much predictive value for the outcome of labor. [7] Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements. Planes and Diameters of the Pelvis The 3 most important planes in the female pelvis are the pelvic inlet, mid-pelvis, and pelvic outlet. Four diameters can describe the pelvic inlet: anteroposterior, transverse, and 2 obliques. Furthermore, based on the landmarks on the pelvic inlet, there are 3 different anteroposterior diameters named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these 3 diameters is obstetrical conjugate, which measures approximately 10.5 cm and is the distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5 cm and is the widest distance between the innominate line on both sides. The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm. Fetal Skull Diameters There are 6 distinguished longitudinal fetal skull diameters: - Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the diameter presented in the vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5 cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the diameter in the face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5 cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor - Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some key movements are impossible in the face or brow presentations. Based on the information provided above, it is obvious that labor be arrested in brow presentation unless it spontaneously changes to the face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery are explained in later sections. As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor. Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore, the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations. Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous. Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large. Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] External transducer devices are advised to prevent damage to the eyes. When internal monitoring is inevitable, monitoring devices on bony parts should be placed carefully. Consultations that are typically requested for patients with delivery of face/brow presentation include the following: - Experienced midwife, preferably looking after laboring women 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (eg, epidural)
- Theatre team - in case of failure to progress, an emergency cesarean section is required.
- Preparation
No specific preparation is required for face or brow presentation. However, discussing the labor options with the mother and birthing partner and informing members of the neonatal, anesthetic, and theatre co-ordinating teams is essential. Mechanism of Labor in Face Presentation During contractions, the pressure exerted by the fundus of the uterus on the fetus and the pressure of the amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery. If the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses. The pubis is described as mentum-anterior when the fetal chin is rotated towards the maternal symphysis. In these cases, further descent through the vaginal canal continues, with approximately 73% of cases delivering spontaneously. [9] The fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery. Mechanism of Labor in Brow Presentation As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot occur. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery. As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10] However, some complications are still associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor. Prolonged labor itself can provoke fetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications. Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation. During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5 cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head engages later, and labor progresses more slowly. Failure to progress in labor is also more common in both presentations compared to the vertex presentation. Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descending through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section. Manual attempts to change face presentation to vertex or manual or forceps rotation to mentum anterior are considered dangerous and discouraged. - Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12] - Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies. Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. - Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this PageBulk download. - Bulk download StatPearls data from FTP
Related informationSimilar articles in PubMed- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2024] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2024 Mar; 230(3S):S890-S900. Epub 2023 May 19.
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Intrapartum sonographic assessment of the fetal head flexion in protracted active phase of labor and association with labor outcome: a multicenter, prospective study. [Am J Obstet Gynecol. 2021] Intrapartum sonographic assessment of the fetal head flexion in protracted active phase of labor and association with labor outcome: a multicenter, prospective study. Dall'Asta A, Rizzo G, Masturzo B, Di Pasquo E, Schera GBL, Morganelli G, Ramirez Zegarra R, Maqina P, Mappa I, Parpinel G, et al. Am J Obstet Gynecol. 2021 Aug; 225(2):171.e1-171.e12. Epub 2021 Mar 4.
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty. Activity recording is turned off. Turn recording back on Connect with NLM National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894 Web Policies FOIA HHS Vulnerability Disclosure Help Accessibility Careers   Antenatal Care Module: 6. Anatomy of the Female Pelvis and Fetal SkullStudy session 6 anatomy of the female pelvis and fetal skull, introduction. In this study session you will learn about the bony structures with the most importance for the pregnant woman and the baby she will give birth to. The bones of the skeleton have the main function of supporting our body weight and acting as attachment points for our muscles. The focus in this study session will be on the female pelvis, which supports the major load of the pregnant uterus, and the fetal skull, which has to pass through the woman’s pelvis when she gives birth. There are certain key landmarks in the anatomy of the female pelvis and the fetal skull that we will show you in this study session. Knowing these landmarks will enable you to estimate the progress of labour, by identifying changes in their relative positions as the baby passes down the birth canal. You will learn how to do this in the next Module in this curriculum, which is on Labour and Delivery Care . Learning Outcomes for Study Session 6When you have studied this session, you should be able to: 6.1 Define and use correctly all of the key words printed in bold . (SAQs 6.1, 6.2 and 6.3) 6.2 Describe the female pelvis and identify the important features for obstetric care. (SAQs 6.1, 6.2 and 6.3) 6.3 Describe the main features of the fetal skull, and their importance for labour and delivery. (SAQs 6.1, 6.2 and 6.3) 6.1 The female bony pelvisThe pelvis is a hard ring of bone (see Figure 6.1), which supports and protects the pelvic organs and the contents of the abdominal cavity. The muscles of the legs, back and abdomen are attached to the pelvis, and their strength and power keep the body upright and enable it to bend and twist at the waist, and to walk and run. 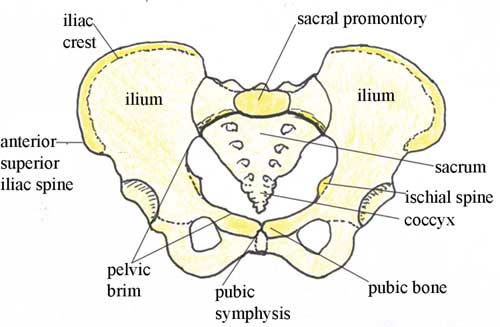 The woman’s pelvis is adapted for child bearing, and is a wider and flatter shape than the male pelvis. The pelvis is composed of pairs of bones, which are fused together so tightly that the joints are difficult to see. We will describe each of the bones in turn, and their major landmarks. It will help you to visualise the anatomy of the pelvis if you keep referring back to Figure 6.1. 6.1.1 IliumIlium is pronounced ‘ill ee umm’ and iliac is ‘ill ee ack’. The major portion of the pelvis is composed of two bones, each called the ilium — one on either side of the backbone (or spinal column) and curving towards the front of the body. When you place your hand on either hip, your hand rests on the iliac crest , which is the upper border of the ilium on that side. At the front of the iliac crest, you can feel the bony protuberance called the anterior superior iliac spine (a ‘protuberance’ is something that sticks out, like a little hill or knob). What do the directional terms ‘anterior superior’ tell you about the position of the iliac spines? (If you can’t remember, look back at Box 3.1 in Study Session 3.) Anterior tells you that the iliac spines are at the front of the body, and superior tells you that they are above the main portion of the ilium on each side. 6.1.2 IschiumThe ischium is the thick lower part of the pelvis, formed from two fused bones — one on either side. When a woman is in labour, the descent of the fetal head as it moves down the birth canal is estimated in relation to the ischial spines , which are inward projections of the ischium on each side. The ischial spines are smaller and rounder in shape in the woman’s pelvis than in that of the man. In the Module on Labour and Delivery Care , you will learn how to feel for the ischial spines to help you estimate how far down the birth canal the baby’s head has progressed. Ischium is pronounced ‘iss kee umm’ and ischial is ‘iss kee al’. 6.1.3 Pubic bones and the symphysis pubisThe pubic bones on either side form the front part of the pelvis. The two pubic bones meet in the middle at the pubi c symphysis . (A symphysis is a very strong bony joint.) The pubic symphysis is immediately below the hair-covered pubic mound that protects the woman’s external genitalia (as shown in Figure 3.2, if you want to look back at it now). When you examine the abdomen of a pregnant woman, feeling for the top of the pubic symphysis with your fingers is a very important landmark. In Study Session 10, you will learn how to measure the height of the uterus from the pubic symphysis to the fundus (top of the uterus — see Figure 3.3 if you need to remind yourself of the position of the fundus). This measurement enables you to estimate the gestational age of the fetus, i.e. how many weeks of the pregnancy have passed, and whether the fetus is growing at the normal rate. 6.1.4 SacrumSacrum is pronounced ‘say krum’. Coccyx is pronounced ‘kok six’. The sacrum is a tapered, wedge-shaped bone at the back of the pelvis, consisting of five fused vertebrae (the small bones that make up the spinal column or backbone). At the bottom of the sacrum is a tail-like bony projection called the coccyx . The upper border of the first vertebra in the sacrum sticks out, and points towards the front of the body; this protuberance is the sacral promontory — an important landmark for labour and delivery. 6.2 The pelvic canalThe roughly circular space enclosed by the pubic bones at the front, and the ischium on either side at the back, is called the pelvic canal — the bony passage through which the baby must pass. This canal has a curved shape because of the difference in size between the anterior (front) and posterior (back) borders of the space created by the pelvic bones. You can see it from the side view in Figure 6.2. 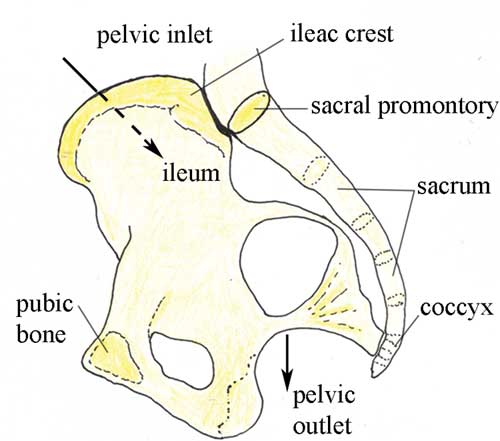 6.2.1 The size and shape of the pelvisThe size and shape of the pelvis is important for labour and delivery. Well-built healthy women, who had a good diet during their childhood growth period, usually have a broad pelvis that is well adapted for childbirth. It has a round pelvic brim and short, blunt ischial spines. (Doctors and midwives call this shape a ‘gynaecoid’ pelvis.) It gives the least difficulty during childbirth, provided the fetus is a normal size and the birth canal has no abnormal tissue growth causing an obstruction. There is considerable variation in pelvis shapes, some of which create problems in labour and delivery. A narrow pelvis can make it difficult for the baby to pass through the pelvic canal. A deficiency of important minerals like iodine in the diet during childhood may result in abnormal development of the pelvic bones. Stunting (being much shorter than average for age) due to malnutrition and/or infectious diseases can also result in a narrow pelvis. Next, we look at the shape of the pelvic canal in more detail, and distinguish between the pelvic inlet (the roughly circular space where the baby’s head enters the pelvis — Figure 6.3), and the pelvic outlet (the roughly circular space where the baby’s head emerges from the pelvis. As you will see in the next section, the inlet and the outlet of the pelvis are not the same size. 6.2.2 The pelvic inletThe pelvic inlet is formed by the pelvic brim, which you saw in Figure 6.1. The pelvic brim is rounded, except where the sacral promontory and the ischial spines project into it. The dimensions in centimetres (cm) of the pelvic inlet are shown in Figure 6.3 in both directions (top to bottom; and transverse or side to side). When you look at Figure 6.3, imagine that you are a baby in the head-down position, looking down on the pelvis from above, at the space you must squeeze through! It is just 13 cm wide (on average) and 12 cm from top to bottom. 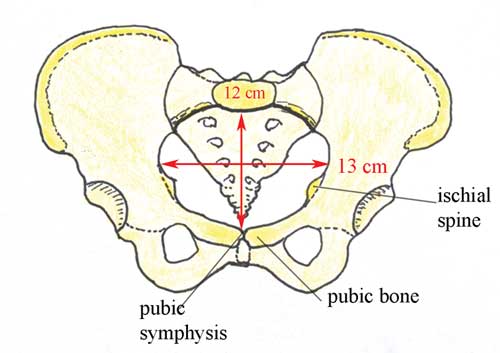 6.2.3 The pelvic outletThe pelvic outlet is formed by the lower border of the pubic bones at the front, and the lower border of the sacrum at the back. The ischial spines point into this space on both sides. Figure 6.4 shows the dimensions of the space that the fetus must pass through as it emerges from the mother’s pelvis. As you look at Figure 6.4, imagine that you are the birth attendant who is looking up the birth canal, waiting to see the fetal head emerging. 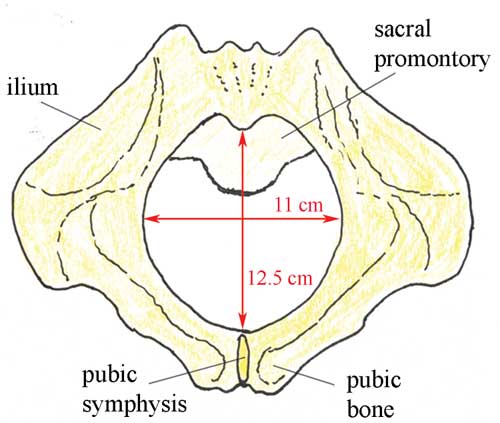 What do you notice when you compare the dimensions of the pelvic inlet (Figure 6.3) and the pelvic outlet (Figure 6.4)? Which is the narrowest? The narrowest diameter for the fetus to pass through is the pelvic outlet, which is only 11 cm wide in the average female pelvis. It is difficult to see from Figures 6.3 and 6.4, but the fetus has to rotate in order to get through the pelvic canal. This is because the pelvic inlet is 13 cm wide, whereas the pelvic outlet is only 11 cm wide. In order to fit through the pelvic outlet at its widest dimension (12.5 cm from top to bottom), the fetus must rotate so it ‘presents’ its head to the widest dimension of the pelvic cavity at every point as it passes through. The largest part of the fetus is the skull, so the baby’s head rotates first, and the shoulders and the rest of the body follow. You will learn all about this in the Labour and Delivery Care Module. First, we have to look more closely at the structure of the fetal skull. 6.3 The fetal skullThe fetal skull is the most difficult part of the baby to pass through the mother’s pelvic canal, due to the hard bony nature of the skull. Understanding the anatomy of the fetal skull and its diameter will help you recognise how a labour is progressing, and whether the baby’s head is ‘presenting’ correctly as it comes down the birth canal. This will give you a better understanding of whether a normal vaginal delivery is likely, or if the mother needs referral because the descent of the baby’s head is not making sufficient progress. 6.3.1 Fetal skull bonesThe skull bones encase and protect the brain, which is very delicate and subjected to pressure when the fetal head passes down the birth canal. Correct presentation of the smallest diameter of the fetal skull to the largest diameter of the mother’s bony pelvis is essential if delivery is to proceed normally. But if the presenting diameter of the fetal skull is larger than the maternal pelvic diameter, it needs very close attention for the baby to go through a normal vaginal delivery. You can locate the main skull bones in Figure 6.5. 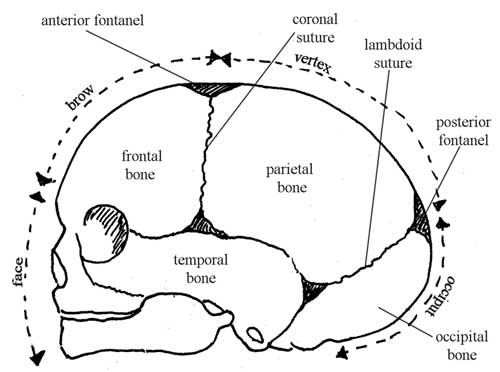 The fetal skull bones are as follows: - The frontal bone , which forms the forehead. In the fetus, the frontal bone is in two halves, which fuse (join) into a single bone after the age of eight years.
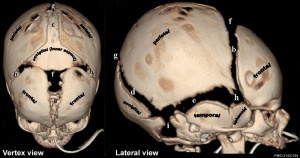
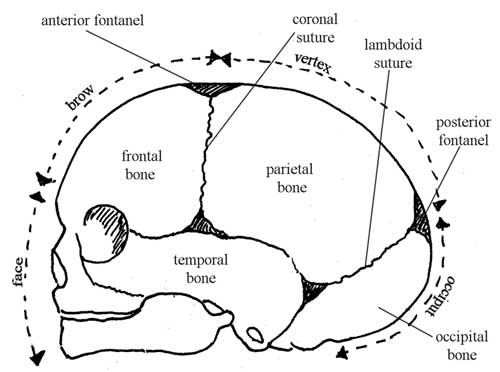
Parietal is pronounced ‘parr eye ett al’. Occipital is pronounced ‘ox ipp itt al’. - The occipital bone , which forms the back of the skull and part of its base. It joins with the cervical vertebrae (neck bones in the spinal column, or backbone).
- The two temporal bones, one on each side of the head, closest to the ear.
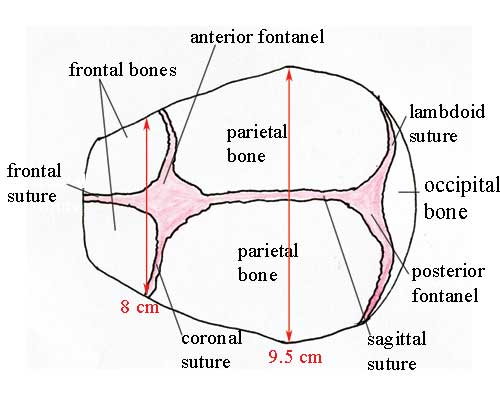
Understanding the landmarks and measurements of the fetal skull will help you to recognise normal and abnormal presentations of the fetus during antenatal examinations, labour and delivery. 6.3.2 SuturesSutures are joints between the bones of the skull. In the fetus they can ‘give’ a little under the pressure on the baby’s head as it passes down the birth canal. During early childhood, these sutures harden and the skull bones can no longer move relative to one another, as they can to a small extent in the fetus and newborn. It is traditional for their names and locations to be taught in midwifery courses. You may be able to tell the angle of the baby’s head as it ‘presents’ in the birth canal by feeling for the position of the main sutures with your examining fingers. You can see the position of the sutures in the fetal skull in Figure 6.6, and also the diameters at two points. Suture is pronounced ‘soo tyor’. 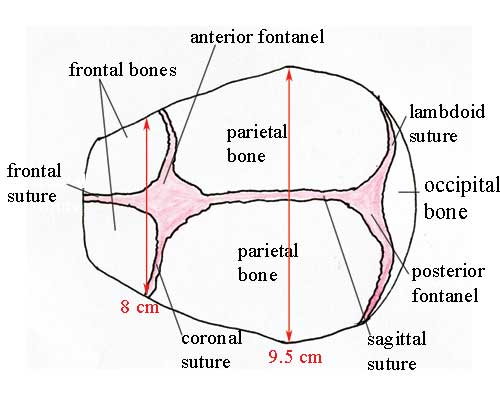 Lambdoid is pronounced ‘lamm doyd’. Sagittal is ‘saj itt al’ and coronal is ‘korr oh nal’. - The sagittal suture joins the two parietal bones together.
- The coronal suture joins the frontal bone to the two parietal bones.
- The frontal suture joins the two frontal bones together.
What do you notice about the diameters given in Figure 6.6, relative to the dimensions of the pelvic canal (Figures 6.3 and 6.4)? At its widest part, the fetal skull is (on average) 9.5 cm wide. This is 3.5 cm less than the widest diameter of the pelvic inlet, and 1.5 cm less than the widest diameter of the pelvic outlet. Thus, if the mother’s pelvis and the fetal skull are the average size, there is just sufficient room for the baby’s head to pass through the pelvic canal if the head rotates to present to the widest dimension of the pelvis. 6.3.3 FontanelsA fontanel is the space created by the joining of two or more sutures. It is covered by thick membranes and the skin on the baby’s head, protecting the brain underneath the fontanel from contact with the outside world. Identification of the two large fontanels on the top of the fetal skull helps you to locate the angle at which the baby’s head is presenting during labour and delivery. The fontanels are shown in Figures 6.5 and 6.6. They are: - The anterior fontanel (also known as the bregma) is a diamond-shaped space towards the front of the baby’s head, at the junction of the sagittal, coronal and frontal sutures. It is very soft and you can feel the fetal heart beat by placing your fingers gently on the fontanel. The skin over the fontanel can be seen ‘pulsing’ in a newborn or young baby.
- The posterior fontanel (or lambda) has a triangular shape, and is found towards the back of the fetal skull. It is formed by the junction of the lambdoid and sagittal sutures.
6.3.4 Regions and landmarks in the fetal skullFigures 6.5 and 6.6 allow you to identify certain regions and landmarks in the fetal skull, which have particular importance for obstetric care because they may form the so-called presenting part of the fetus — that is, the part leading the way down the birth canal. - The vertex is the area midway between the anterior fontanel, the two parietal bones and the posterior fontanel. A vertex presentation occurs when this part of the fetal skull is leading the way. This is the normal and the safest presentation for a vaginal delivery.
- The brow is the area of skull which extends from the anterior fontanel to the upper border of the eye. A brow presentation is a significant risk for the mother and the baby.
- The face extends from the upper ridge of the eye to the nose and chin (lower jaw). A face presentation is also a significant risk for the mother and baby.
- The occiput is the area between the base of the skull and the posterior fontanel. It is unusual and very risky for the occiput to be the presenting part.
When you study the next Module on Labour and Delivery Care , you will learn about other presentations, including ‘breech’ (the baby is head-up and its feet or bottom is the presenting part), and ‘shoulder’ first. Now that you know all the major anatomical features of the female reproductive system, the female pelvis and the fetal skull, we move on in Study Session 7 to consider the major physiological changes that take place in a woman’s body during pregnancy. Summary of Study Session 6In Study Session 6, you have learned that: - The bony pelvis is composed of the ilium, ischium, pubic bones and sacrum.
- The size and shape of the bony pelvis can affect the ease or difficulty of labour and delivery; a broad pelvis gives less difficulty than a narrow one, which may obstruct the descent of the baby down the birth canal.
- Certain landmarks in the anatomy of the pelvis are commonly used to estimate the descent of the baby during labour and delivery. The two most important landmarks are the ischial spines and the sacral promontory, which can be felt with the fingers during a vaginal examination.
- The pelvic inlet is the space where the baby’s head enters the pelvis; it is larger than the pelvic outlet, where the baby’s head emerges from the pelvis. In order to get through the widest diameter of the inlet and the outlet, the baby has to rotate as it passes through the pelvic canal.
- The skull is formed by several bones joined tightly together by joints called sutures. In the fetus and newborn, spaces called fontanels exist between some of the skull bones on the top of the baby’s head. The position of the sutures and the fontanels can tell you about the angle at which the baby’s head is presenting during labour and delivery.
- The vertex presentation (where the top of the baby’s head is the presenting part) is the most common and the safest presentation for a normal vaginal delivery. Other presentations carry a much higher risk for the mother and baby.
Self-Assessment Questions (SAQs) for Study Session 6Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module. SAQ 6.1 (tests Learning Outcomes 6.1, 6.2 and 6.3)Match each anatomical name with the correct description. Hip bone in the pelvis Paired bones forming the front of the skull Frontal bones Joint between the parietal bones in the fetal skull Sagittal suture Fused vertebrae at the back of the bony pelivs The top of the fetal skull between the two fontanels Using the following two lists, match each numbered item with the correct letter. b. Sagittal suture e. Frontal bones SAQ 6.2 (tests Learning Outcomes 6.1, 6.2 and 6.3)Which of the following statements is false ? In each case, say why it is incorrect. A The female bony pelvis is broader and flatter than the male pelvis. B The pelvic inlet is narrower than the pelvic outlet. C The iliac crest is an important landmark in measuring the progress of the fetus down the birth canal. D The sutures in the fetal skull are strong hard joints that hold the skull bones rigidly in place. E A newborn baby’s pulse can be seen beating in the anterior fontanel. A is true. The female bony pelvis is broader and flatter than the male pelvis. B is false . The pelvic inlet is wider (not narrower) than the pelvic outlet. C is false . The iliac crest is the protuberance at the front of each hip bone; it is not important in measuring the progress of the fetus down the birth canal. D is false . The sutures in the fetal skull ‘give’ a little under the pressure in the birth canal, allowing the skull bones to move to a small extent. This makes it easier for the baby’s head to pass through the mother’s bony pelvis. E is true. A newborn baby’s pulse can be seen beating in the anterior fontanel. SAQ 6.3 (tests Learning Outcomes 6.1, 6.2 and 6.3)List four possible features of the maternal bony pelvis and/or the fetal skull that may result in a difficult labour and delivery. The possible features of the maternal bony pelvis and/or the fetal skull that may result in a difficult labour and delivery include (you only had to suggest four): - A narrow or deformed pelvis
- Abnormal growth of tissue in the pelvic cavity
- A large fetal skull
- A brow, face, breech or shoulder presentation of the fetus
- A fetus that does not present the widest part of its skull to the widest part of the pelvic inlet, and then rotate to do the same in the pelvic outlet.
Except for third party materials and/or otherwise stated (see terms and conditions ) the content in OpenLearn is released for use under the terms of the Creative Commons Attribution-NonCommercial-Sharealike 2.0 licence . In short this allows you to use the content throughout the world without payment for non-commercial purposes in accordance with the Creative Commons non commercial sharealike licence. Please read this licence in full along with OpenLearn terms and conditions before making use of the content. When using the content you must attribute us (The Open University) (the OU) and any identified author in accordance with the terms of the Creative Commons Licence. The Acknowledgements section is used to list, amongst other things, third party (Proprietary), licensed content which is not subject to Creative Commons licensing. Proprietary content must be used (retained) intact and in context to the content at all times. The Acknowledgements section is also used to bring to your attention any other Special Restrictions which may apply to the content. For example there may be times when the Creative Commons Non-Commercial Sharealike licence does not apply to any of the content even if owned by us (the OU). In these stances, unless stated otherwise, the content may be used for personal and non-commercial use. We have also identified as Proprietary other material included in the content which is not subject to Creative Commons Licence. These are: OU logos, trading names and may extend to certain photographic and video images and sound recordings and any other material as may be brought to your attention. Unauthorised use of any of the content may constitute a breach of the terms and conditions and/or intellectual property laws. We reserve the right to alter, amend or bring to an end any terms and conditions provided here without notice. All rights falling outside the terms of the Creative Commons licence are retained or controlled by The Open University. Head of Intellectual Property, The Open University  fetal skullJul 31, 2022 150 likes | 480 Views nursing education Share Presentation Presentation TranscriptPRESENTED BY:ABHILASHA VERMAM.Sc. Prev. PRESENTATION ON FETAL SKULL FETAL SKULL SHAPE - OVAL AREAS OF FETAL SKULL BONES OF FETAL SKULL • FRONT SIDE • BACK SIDE SUTURE OF FETAL SKULL “Space between skull bones” • Frontal suture • Saggital suture • Coronal suture • Lambdoid suture FONTANELLS “ Wide gap between suture line where 2 or more suture are meet” LANDMARKS OF FETAL SKULL • Occiput • Lambda • Vertex • Parietal eminance • Bregma • Siniciput • Glabella • Nasion • Mentum TRANSVERSE DIAMETERS 1) Biparietal Dm [9.5 cm]: • Distance between parietal eminances. 2) Bitemporal Dm [ 8.5 cm] • Distance between lateral side of temporal bone or coronal suture. ANTERIOR- POSTERIOR DIAMETER • SUB-OCCIPUTO BREGMATIC DIAMETER [9.5 CM] • From below occipital protuberance to center of anterior fontanelle. 2. SUB-OCCIPUTO FRONTAL DIAMETER [10 CM] • From below occipital protuberance to center of frontal suture. 3. OCCIPUTO FRONTAL DIAMETER [ 11.5 CM] • From occipital protuberance to glabella. 4. MENTO-VERTICLE DIAMETER [ 14 CM] • From chin to vertical point. 5. SUBMENTO VERTICAL DIAMETER [ 11.5 CM] • From junction of mouth and neck to highest point of vertex. • SUBMENTO BREGMATIC [ 9.5 CM] • From junction of neck and lower jaw to bregma. PRESENTING DIAMETER OF FETAL HEAD MOULDING “ It is reduction in the diameter of fetal skull which encourage progress of delivery to rigid maternal pelvis without harming fetal brain.” • Skull bones are over ride each other and reduce head circumference.  Bony pelvis and fetal skull Dr Malleswar Rao KBony pelvis and fetal skull Dr Malleswar Rao K. Objects. Fetal head Pelvic anatomy Pelvic shapes. Passenger. Fetal head. Landmarks Sutures Fontanelles Diameters. Fetal head. From an obstetrical point of view it ’ s the most important part: largest 2.96k views • 23 slides  Infant Skull vs. Adult SkullInfant Skull vs. Adult Skull. Pg. 143 Figure 7.15. A Lateral & superior View of the infant skull Fontanels : fibrous membranes that permit some movement between the bones so that the growing skull can change shape& aid in labor through the birth canal. 4.95k views • 5 slides  2. . TECHNICAL ASPECTS. Sitting erect positions are preferred to exclude any air-fluid levels within the cranial cavities or sinuses. Patient comfort and skull immobilization are necessary. Exposure factors range between 75 kVp and 85 kVp. A small focus is to be used with short 824 views • 32 slides  Skull StudiesSkeleton. Framework of an animal's bodyGives shape, support, and protectionVertebrates, endoskeletonMuscle attachment allowing for movementSkull portion includes teeth and bone plates. Skeleton is a result of evolutionary changeAnimal adaptation to their environmentRole or nicheAnalyzing an 328 views • 17 slides  The skull. Forensic anthropology. The Skull. Total # - 22 8 paired, 6 unpaired Cranium – skull without mandible Calvarium – cranium without face Sutures: serrated and interdigitated The only moveable (synovial) joints Occipital condyles and C1 TMJ. The Frontal Bone. Unpaired 618 views • 33 slides  Skull. Usually consists of 22 bones, all of which (except the lower jaw) are firmly interlocked along lines called “sutures”. Cranium = 8 bones Facial skeleton = 13 bones + lower jaw Lower jaw bone is called the mandible , and is the only movable bone. Cranium. Functions: 818 views • 16 slides  skull. Some pots and a mask. Likeness of me. Tollund man actual. Tollund man face. Tollund man likeness. Tollund man likeness. Tollund man likeness, face. Drawings. More drawings. One more drawing…. 1345 williamson st. Mantel. Entertainment center. Williamson st stairs. 426 views • 20 slides  The Skull. The skull, the skeleton of the head , is the most complex bony structure in the body because it: Encloses the brain , which is irregular in shape; Houses the organs of special senses for seeing, hearing, tasting, and smelling; and 620 views • 29 slides  Skull. Objectives. Identify the different bones forming the skull with important foramina . Differentiate between the bony features of the skull of an adult and infant. The Skull. It consists of flat and irregular bones Divides into: Cranial bones which encase the brain 917 views • 19 slides  Hominoid Skull:Hominoid Skull:. Lab Investigation:. Lab Report Format:. 1. Title 2. Objectives 3. Introduction/background 4. Procedure 5. Data 6. Results 7. Conclusion. 1. Title. Hominoid Skulls: Name(s) Period. 2. Objectives. Found on pg. S1 of student handout. 3. Intoduction /Background. 224 views • 9 slides  SKULL. 29.November.2011 Tuesday. Kaan Yücel M.D.,Ph.D. The cranium (skull) is the skeleton of the head. A series of bones form its two parts: Neurocranium Viscerocranium (Facial bones ). 1.63k views • 88 slides  The Skull. Things to know. 3 views AP AP axial Lateral. AP. 10 X 12 lengthwise 80 @ 18 Shield Marker Hold breath. Positioning. Patient Supine on table Flex neck until the OML is perpendicular to IR Mid line to Mid line No rotation or tilt. CR perpendicular. Enter at Glabella. 419 views • 14 slides  SKULL. SKULL & ORBIT see handouts. SKULL. ORBITAL REGION Fronto-Zygomatic suture – over outer canthus, palpate w/finger tips Superior Orbital Notch – located in sup. orbital rim, (highest point of curve. Supercilliary Ridge – palpated bilaterally @ the most medial aspect of the orbit. 2.33k views • 202 slides  SKULL. Dr. Nivin Sharaf MD LMCC. Objectives. Brain storm basic functions of the human skull To identify basic anatomical features of the skull To be able to recognize different bony landmarks of the skull To Identify outer bony features of bones of the skull 726 views • 30 slides 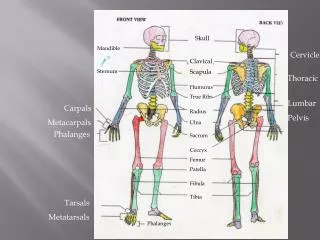 Skull. Mandible. Cervicle. Clavical. Sternum. Scapula. Thoracic. Humurus. True Ribs. Lumbar. Carpals. Radius. Pelvis. Metacarpals. Ulna. Phalanges. Sacrum. Coccyx. Femur. Patella. Fibula. Tibia. Tarsals. Metatarsals. Phalanges. Distal innerphalangeal Joint. 562 views • 10 slides  The Skull. Pages 120-126 in Textbook. Kyle Franklin Megan Gleason Emily Giannotti. Cranial Sutures. Sutures- lines at which 2 bones fuse together. These are the 4 on the cranium: Coronal Suture - fuses parietal bones to frontal bone. 409 views • 16 slides  Skull IllusionsSkull Illusions. 420 views • 31 slides  ANATOMY OF THE FEMALE BONY PELVIS and FETAL SKULLANATOMY OF THE FEMALE BONY PELVIS and FETAL SKULL. Quoted with modification from Dr. Salwa Neyazi King Saud University. THE BONY PELVIS. WHICH BONES COMPOSE THE BONY PELVIS? Ilium, Ischium, Pubis Sacrum Coccyx. THE BONY PELVIS. WHAT IS THE PELVIC BRIM? 3.15k views • 34 slides  SKULL. HUMAN SKULL. Consists of 22 bones 8 of these bones make up the cranium 14 form the facial skeleton. (also 6 tiny bones in the middle ear). The cranium encloses and protect the brain, and its surface provides attachments for muscles that make chewing and head movements possible. 1.01k views • 42 slides  Skull. Formed by two sets of bones:. Cranium. The cranium is composed of External Acoustic Meatus – Styloid process – Zygomatic process – Mastoid process –. Features of the Temporal Bones. C. A. D. B. Cranium Bone Information. 334 views • 14 slides  Skull WatchesSkull watches look unique and as well as stylish. At Nemesis Watch, we have a wide range of collection of skull watches and they are of extremely fine quality and affordable price. For its edgy effect, this watch could be a choice for those who loves to try all things new and wild. For more visit website: https://nemesiswatch.com/product-tag/skull-watch/ 111 views • 8 slides  Skull watches look unique and as well as stylish. At Nemesis Watch, we have a wide range of collection of skull watches and they are of extremely fine quality and affordable price. For its edgy effect, this watch could be a choice for those who loves to try all things new and wild. 59 views • 3 slides  Fetal Presentation, Position, and Lie (Including Breech Presentation)- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery. Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way. Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back). Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique). For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following: Head first (called vertex or cephalic presentation) Facing backward (occiput anterior position) Spine parallel to mother's spine (longitudinal lie) Neck bent forward with chin tucked Arms folded across the chest If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible. Variations in fetal presentation, position, or lie may occur when The fetus is too large for the mother's pelvis (fetopelvic disproportion). The uterus is abnormally shaped or contains growths such as fibroids . The fetus has a birth defect . There is more than one fetus (multiple gestation).  Position and Presentation of the FetusToward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder. Occiput posterior position (facing forward, toward the mother's pubic bone) is less common than occiput anterior position (facing backward, toward the mother's spine). |
Variations in Fetal Position and PresentationSome variations in position and presentation that make delivery difficult occur frequently. Occiput posterior positionIn occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back). When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary. Breech presentationIn breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head). When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first. The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first. In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery. Breech presentation is more likely to occur in the following circumstances: Labor starts too soon (preterm labor). The uterus is abnormally shaped or contains abnormal growths such as fibroids . Other presentationsIn face presentation, the baby's neck arches back so that the face presents first rather than the top of the head. In brow presentation, the neck is moderately arched so that the brow presents first. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended. In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.  Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.   | 

















/images/vimeo_thumbnails/258259549/TJabByIaQwCkhI4PujnhCQ_overlay.jpg)
:background_color(FFFFFF):format(jpeg)/images/library/7741/eEsfu70EOMx1TlBf5tYAiA_Go0bFvBvzClwSivuaiELg_head_01.png)
:background_color(FFFFFF):format(jpeg)/images/library/7739/Yw9DFAjpeIjZu3iUn7UFxQ_RpHn9yFnfaSTgwdrVROMJQ_head_02.png)









COMMENTS
Correct presentation of the smallest diameter of the fetal skull to the largest diameter of the mother's bony pelvis is essential if delivery is to proceed normally. But if the presenting diameter of the fetal skull is larger than the maternal pelvic diameter, it needs very close attention for the baby to go through a normal vaginal delivery.
Types of Fetal Skull Presentations. The fetal skull can present in several different ways during labor, depending on the position of the head in relation to the birth canal. The most common presentation is the vertex presentation, where the head is flexed and the occiput is the presenting part.
Fetal Head (12 weeks) showing cartilage (blue) and bone (red) The skull is a unique skeletal structure in several ways: embryonic cellular origin (neural crest and mesoderm), form of ossification (intramembranous and ) and flexibility (fibrous sutures). The cranial vault (which encloses the brain) bones are formed by intramembranous ossification.
In this video, we delve into the intricate details of the fetal skull, exploring its anatomy, developmental milestones, and clinical significance. From the f...
Development of the skull
Anatomy of the Newborn Skull
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
FETAL SKULL.ppt - Free download as Powerpoint Presentation (.ppt), PDF File (.pdf), Text File (.txt) or view presentation slides online. This document discusses the fetal skull, including its anatomy, diameters, and changes during labor. It is divided into sections on the vault, base, and face of the skull. Key points include: - The skull is large relative to the fetal body and must adapt ...
A vertex presentation occurs when this part of the fetal skull is leading the way. This is the normal and the safest presentation for a vaginal delivery. The brow is the area of skull which extends from the anterior fontanel to the upper border of the eye. A brow presentation is a significant risk for the mother and the baby.
The fetal head is the most significant component of the fetus because it is the most common presenting part: it is the largest and least compressible and, once born, generally facilitates a smooth delivery of the remainder of the body. The fetal skull is built on big, ossified, securely connected bones that are not easily compressed. Their roles are to protect the brain stem's essential centers.
6. Anatomy of the Female Pelvis and Fetal Skull: View as ...
Fetal Skull - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. This document discusses the anatomy of the fetal skull. It describes the three main parts of the skull - the vault, face, and base. It details the individual bones that make up each part, including sutures, fontanelles, and diameters.
PRESENTING DIAMETER OF FETAL HEAD. MOULDING " It is reduction in the diameter of fetal skull which encourage progress of delivery to rigid maternal pelvis without harming fetal brain.". • Skull bones are over ride each other and reduce head circumference. THANK YOU. nursing education Slideshow 11505739 by today5.
Fetal Skull - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. The fetal skull contains delicate brain tissue that is subjected to pressure during birth. The skull bones are separated by soft membranes called sutures and fontanelles which allow the skull to change shape during labor.
Fetal Presentation, Position, and Lie (Including Breech ...
FETAL SKULL PPT by Komal upreti - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. The document discusses the fetal skull, including its importance, divisions, bones, sutures and fontanelles. It describes the various diameters and circumferences of the fetal skull and their significance in assessing labor progression.