164 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.

Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
August 13, 2024
Finding Happiness At Sea As A Yacht Captain After Overcoming Depression and Anxiety
“If a situation is making you unhappy – a marriage, a job, a family member – anything – change the situation. You can leave, you can stop speaking to someone (yes, even a parent or another family member), and you can do so free of guilt because you are in charge of your own happiness, and life is too short to choose anything different for yourself.”
Struggled with: Anxiety Depression Suicidal
Helped by: Medication Therapy
August 6, 2024
Overcoming Neglect, Childhood Trauma and Abuse Through Careful Self-Improvement
“When I was 12 years old, my parents moved into their own place, along with my brother and sister. They left me with my grandparents. I could only see my family on weekends, and on Sunday evenings I would go back home. I was not able to build a normal relationship with my brother and sister. I even thought at one point that I was adopted, which was against all logic.”
Struggled with: Abuse Childhood
Helped by: Journaling Self-improvement
July 30, 2024
Overcoming a Rare Autoimmune Disease With a Careful Diet and Self-Improvement
“There were weeks when I wouldn’t leave my house, feeling too overwhelmed and exhausted to face the world. I tend to isolate myself rather than reaching out to others, which only compounded my feelings of loneliness and despair. I had to repattern my behavior and learn to ask for help or talk about my feelings, but it wasn’t easy. I internalized a lot of my pain and frustration, which made me feel even more isolated.”
Struggled with: Anxiety Autoimmune disease
Helped by: Self-improvement
July 23, 2024
Surviving The Boston Marathon Bombings While Facing TBI and Medical Gaslighting
“As I literally lived on his couch, with my port-a-potty in his living room, my partner eventually applied for permanent disability status for me. But, even the doctor gaslighted me, told me I was physically able to work, and reported the same to the government. In reality, I was so dizzy with vertigo, this same doctor refused to let me walk to and from our car, by myself, fearing I’d fall and sue!”
Struggled with: CPTSD Traumatic Brain Injury
Helped by: Treatment
July 16, 2024
Somatic Therapy Helped Me Heal From CPTSD After Years of Childhood Abuse
“At 22 years old, I knew that I was dying of alcoholism. I accepted that. The trauma symptoms I experienced were too overwhelming to stop drinking. When I was sober, I would sometimes experience 30 to 40 body memories of being sexually assaulted–again and again in succession. I drank to feel numb.”
Struggled with: Abuse Addiction CPTSD Suicidal
Helped by: Social support Therapy
July 9, 2024
Learning To Live With Irritable Bowel Syndrome With Therapy And A Positive Mindset
“Raising four young children and battling a chronic illness with no cure was challenging for me. On the outside, I looked OK. But I wasn’t and in some ways today still have flare-ups and struggles, the difference is, I now know how to maintain it, especially knowing this will be the rest of my life regardless!”
Struggled with: Irritable Bowel Syndrome
Helped by: Therapy Treatment
July 4, 2024
How A Rescue Dog Helped Me Overcome TBI, Depression and Suicidal Ideation
“I sat on the summer-hot pavement, and no one stopped or asked me if I was okay. No one called the police. People walked around me as quickly as possible. When I was all cried out, I walked home to my empty house. I bought a set of knives, ostensibly for cooking, but that was not the reason. I had thought about pills, and every day I researched how many of each prescription drug I was on would I need to take to die. Using a sharp knife seemed so much easier.”
Struggled with: Depression Suicidal Traumatic Brain Injury
Helped by: Medication Pets Volunteering
July 2, 2024
Walking El Camino de Santiago Helped Me Reconnect With My Authentic Self
“Beneath the outward bravado, I battled with self-doubt and kept wondering why genuine connections seemed beyond my ability. Even though I put out valiant efforts to conceal it, my inner turmoil seeped out, leaving me feeling exposed and vulnerable. And, I knew they could tell.”
Struggled with: Feeling lost People-pleasing Self-doubt
Helped by: Self-acceptance Self-awareness
June 27, 2024
My Journey of Overcoming Heartbreak Thanks to Self-Care and The Support Of Friends
“I’ve learned that finding the right people to confide in, those who offer genuine support and empathy, can make a significant difference in navigating these challenges. It takes time and trust to build those connections, but they are invaluable.”
Struggled with: Breakup
Helped by: Self-Care Social support
June 19, 2024
How Therapy, Self-Help and Medication Help Me Live With Depression and Anxiety
“When the next depressive episode hit in 2018, I was devastated. How could this happen again when I thought I had it all figured out? I experienced some of the darkest moments of my life and a nearly complete loss of hope.”
Struggled with: Anxiety Bipolar Disorder Depression Suicidal

Mental Health Case Study: Understanding Depression through a Real-life Example
Through the lens of a gripping real-life case study, we delve into the depths of depression, unraveling its complexities and shedding light on the power of understanding mental health through individual experiences. Mental health case studies serve as invaluable tools in our quest to comprehend the intricate workings of the human mind and the various conditions that can affect it. By examining real-life examples, we gain profound insights into the lived experiences of individuals grappling with mental health challenges, allowing us to develop more effective strategies for diagnosis, treatment, and support.
The Importance of Case Studies in Understanding Mental Health
Case studies play a crucial role in the field of mental health research and practice. They provide a unique window into the personal narratives of individuals facing mental health challenges, offering a level of detail and context that is often missing from broader statistical analyses. By focusing on specific cases, researchers and clinicians can gain a deeper understanding of the complex interplay between biological, psychological, and social factors that contribute to mental health conditions.
One of the primary benefits of using real-life examples in mental health case studies is the ability to humanize the experience of mental illness. These narratives help to break down stigma and misconceptions surrounding mental health conditions, fostering empathy and understanding among both professionals and the general public. By sharing the stories of individuals who have faced and overcome mental health challenges, case studies can also provide hope and inspiration to those currently struggling with similar issues.
Depression, in particular, is a common mental health condition that affects millions of people worldwide. Disability Function Report Example Answers for Depression and Bipolar: A Comprehensive Guide offers valuable insights into how depression can impact daily functioning and the importance of accurate reporting in disability assessments. By examining depression through the lens of a case study, we can gain a more nuanced understanding of its manifestations, challenges, and potential treatment approaches.
Understanding Depression
Before delving into our case study, it’s essential to establish a clear understanding of depression and its impact on individuals and society. Depression is a complex mental health disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities. It can affect a person’s thoughts, emotions, behaviors, and overall well-being.
Some common symptoms of depression include:
– Persistent sad, anxious, or “empty” mood – Feelings of hopelessness or pessimism – Irritability – Loss of interest or pleasure in hobbies and activities – Decreased energy or fatigue – Difficulty concentrating, remembering, or making decisions – Sleep disturbances (insomnia or oversleeping) – Appetite and weight changes – Physical aches or pains without clear physical causes – Thoughts of death or suicide
The prevalence of depression worldwide is staggering. According to the World Health Organization, more than 264 million people of all ages suffer from depression globally. It is a leading cause of disability and contributes significantly to the overall global burden of disease. The impact of depression extends far beyond the individual, affecting families, communities, and economies.
Depression can have profound consequences on an individual’s quality of life, relationships, and ability to function in daily activities. It can lead to decreased productivity at work or school, strained personal relationships, and increased risk of other health problems. The economic burden of depression is also substantial, with costs associated with healthcare, lost productivity, and disability.
The Significance of Case Studies in Mental Health Research
Case studies serve as powerful tools in mental health research, offering unique insights that complement broader statistical analyses and controlled experiments. They allow researchers and clinicians to explore the nuances of individual experiences, providing a rich tapestry of information that can inform our understanding of mental health conditions and guide the development of more effective treatment strategies.
One of the key advantages of case studies is their ability to capture the complexity of mental health conditions. Unlike standardized questionnaires or diagnostic criteria, case studies can reveal the intricate interplay between biological, psychological, and social factors that contribute to an individual’s mental health. This holistic approach is particularly valuable in understanding conditions like depression, which often have multifaceted causes and manifestations.
Case studies also play a crucial role in the development of treatment strategies. By examining the detailed accounts of individuals who have undergone various interventions, researchers and clinicians can identify patterns of effectiveness and potential barriers to treatment. This information can then be used to refine existing approaches or develop new, more targeted interventions.
Moreover, case studies contribute to the advancement of mental health research by generating hypotheses and identifying areas for further investigation. They can highlight unique aspects of a condition or treatment that may not be apparent in larger-scale studies, prompting researchers to explore new avenues of inquiry.
Examining a Real-life Case Study of Depression
To illustrate the power of case studies in understanding depression, let’s examine the story of Sarah, a 32-year-old marketing executive who sought help for persistent feelings of sadness and loss of interest in her once-beloved activities. Sarah’s case provides a compelling example of how depression can manifest in high-functioning individuals and the challenges they face in seeking and receiving appropriate treatment.
Background: Sarah had always been an ambitious and driven individual, excelling in her career and maintaining an active social life. However, over the past year, she began to experience a gradual decline in her mood and energy levels. Initially, she attributed these changes to work stress and the demands of her busy lifestyle. As time went on, Sarah found herself increasingly isolated, withdrawing from friends and family, and struggling to find joy in activities she once loved.
Presentation of Symptoms: When Sarah finally sought help from a mental health professional, she presented with the following symptoms:
– Persistent feelings of sadness and emptiness – Loss of interest in hobbies and social activities – Difficulty concentrating at work – Insomnia and daytime fatigue – Unexplained physical aches and pains – Feelings of worthlessness and guilt – Occasional thoughts of death, though no active suicidal ideation
Initial Diagnosis: Based on Sarah’s symptoms and their duration, her therapist diagnosed her with Major Depressive Disorder (MDD). This diagnosis was supported by the presence of multiple core symptoms of depression that had persisted for more than two weeks and significantly impacted her daily functioning.
The Treatment Journey
Sarah’s case study provides an opportunity to explore the various treatment options available for depression and examine their effectiveness in a real-world context. Supporting a Caseworker’s Client Who Struggles with Depression offers valuable insights into the role of support systems in managing depression, which can complement professional treatment approaches.
Overview of Treatment Options: There are several evidence-based treatments available for depression, including:
1. Psychotherapy: Various forms of talk therapy, such as Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), can help individuals identify and change negative thought patterns and behaviors associated with depression.
2. Medication: Antidepressants, such as Selective Serotonin Reuptake Inhibitors (SSRIs), can help regulate brain chemistry and alleviate symptoms of depression.
3. Combination Therapy: Many individuals benefit from a combination of psychotherapy and medication.
4. Lifestyle Changes: Exercise, improved sleep habits, and stress reduction techniques can complement other treatments.
5. Alternative Therapies: Some individuals find relief through approaches like mindfulness meditation, acupuncture, or light therapy.
Treatment Plan for Sarah: After careful consideration of Sarah’s symptoms, preferences, and lifestyle, her treatment team developed a comprehensive plan that included:
1. Weekly Cognitive Behavioral Therapy sessions to address negative thought patterns and develop coping strategies.
2. Prescription of an SSRI antidepressant to help alleviate her symptoms.
3. Recommendations for lifestyle changes, including regular exercise and improved sleep hygiene.
4. Gradual reintroduction of social activities and hobbies to combat isolation.
Effectiveness of the Treatment Approach: Sarah’s response to treatment was monitored closely over the following months. Initially, she experienced some side effects from the medication, including mild nausea and headaches, which subsided after a few weeks. As she continued with therapy and medication, Sarah began to notice gradual improvements in her mood and energy levels.
The CBT sessions proved particularly helpful in challenging Sarah’s negative self-perceptions and developing more balanced thinking patterns. She learned to recognize and reframe her automatic negative thoughts, which had been contributing to her feelings of worthlessness and guilt.
The combination of medication and therapy allowed Sarah to regain the motivation to engage in physical exercise and social activities. As she reintegrated these positive habits into her life, she experienced further improvements in her mood and overall well-being.
The Outcome and Lessons Learned
Sarah’s journey through depression and treatment offers valuable insights into the complexities of mental health and the effectiveness of various interventions. Understanding the Link Between Sapolsky and Depression provides additional context on the biological underpinnings of depression, which can complement the insights gained from individual case studies.
Progress and Challenges: Over the course of six months, Sarah made significant progress in managing her depression. Her mood stabilized, and she regained interest in her work and social life. She reported feeling more energetic and optimistic about the future. However, her journey was not without challenges. Sarah experienced setbacks during particularly stressful periods at work and struggled with the stigma associated with taking medication for mental health.
One of the most significant challenges Sarah faced was learning to prioritize her mental health in a high-pressure work environment. She had to develop new boundaries and communication strategies to manage her workload effectively without compromising her well-being.
Key Lessons Learned: Sarah’s case study highlights several important lessons about depression and its treatment:
1. Early intervention is crucial: Sarah’s initial reluctance to seek help led to a prolongation of her symptoms. Recognizing and addressing mental health concerns early can prevent the condition from worsening.
2. Treatment is often multifaceted: The combination of medication, therapy, and lifestyle changes proved most effective for Sarah, underscoring the importance of a comprehensive treatment approach.
3. Recovery is a process: Sarah’s improvement was gradual and non-linear, with setbacks along the way. This emphasizes the need for patience and persistence in mental health treatment.
4. Social support is vital: Reintegrating social activities and maintaining connections with friends and family played a crucial role in Sarah’s recovery.
5. Workplace mental health awareness is essential: Sarah’s experience highlights the need for greater understanding and support for mental health issues in professional settings.
6. Stigma remains a significant barrier: Despite her progress, Sarah struggled with feelings of shame and fear of judgment related to her depression diagnosis and treatment.
Sarah’s case study provides a vivid illustration of the complexities of depression and the power of comprehensive, individualized treatment approaches. By examining her journey, we gain valuable insights into the lived experience of depression, the challenges of seeking and maintaining treatment, and the potential for recovery.
The significance of case studies in understanding and treating mental health conditions cannot be overstated. They offer a level of detail and nuance that complements broader research methodologies, providing clinicians and researchers with invaluable insights into the diverse manifestations of mental health disorders and the effectiveness of various interventions.
As we continue to explore mental health through case studies, it’s important to recognize the diversity of experiences within conditions like depression. Personal Bipolar Psychosis Stories: Understanding Bipolar Disorder Through Real Experiences offers insights into another complex mental health condition, illustrating the range of experiences individuals may face.
Furthermore, it’s crucial to consider how mental health issues are portrayed in popular culture, as these representations can shape public perceptions. Understanding Mental Disorders in Winnie the Pooh: Exploring the Depiction of Depression provides an interesting perspective on how mental health themes can be embedded in seemingly lighthearted stories.
The field of mental health research and treatment continues to evolve, driven by the insights gained from individual experiences and comprehensive studies. By combining the rich, detailed narratives provided by case studies with broader research methodologies, we can develop more effective, personalized approaches to mental health care. As we move forward, it is essential to continue exploring and sharing these stories, fostering greater understanding, empathy, and support for those facing mental health challenges.
References:
1. World Health Organization. (2021). Depression. Retrieved from https://www.who.int/news-room/fact-sheets/detail/depression
2. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
3. Beck, A. T., & Alford, B. A. (2009). Depression: Causes and treatment. University of Pennsylvania Press.
4. Cuijpers, P., Quero, S., Dowrick, C., & Arroll, B. (2019). Psychological treatment of depression in primary care: Recent developments. Current Psychiatry Reports, 21(12), 129.
5. Malhi, G. S., & Mann, J. J. (2018). Depression. The Lancet, 392(10161), 2299-2312.
6. Otte, C., Gold, S. M., Penninx, B. W., Pariante, C. M., Etkin, A., Fava, M., … & Schatzberg, A. F. (2016). Major depressive disorder. Nature Reviews Disease Primers, 2(1), 1-20.
7. Sapolsky, R. M. (2004). Why zebras don’t get ulcers: The acclaimed guide to stress, stress-related diseases, and coping. Holt paperbacks.
8. Yin, R. K. (2017). Case study research and applications: Design and methods. Sage publications.
Similar Posts

Semaglutide and Depression: Understanding the Connection
As scientists unravel the complex interplay between weight-loss medications and mental health, a surprising connection between Semaglutide and depression has emerged, sparking both concern and curiosity in the medical community. This revelation has prompted researchers and healthcare professionals to delve deeper into the potential implications of this relationship, seeking to understand the mechanisms at play…

Is Depression Selfish? Understanding the Relationship Between Mental Health and Selfishness
Shattering the misconception that depression equates to selfishness, we delve into the intricate relationship between mental health and self-preservation, challenging societal stigmas along the way. Depression is a complex mental health condition that affects millions of people worldwide, yet it remains widely misunderstood and stigmatized. One of the most damaging misconceptions is the idea that…
Understanding Self-Loathing: Is it a Sign of Depression?
Self-loathing is a complex emotional state that can significantly impact an individual’s mental health and overall well-being. It’s a feeling that often goes hand in hand with depression, creating a challenging cycle that can be difficult to break. In this article, we’ll explore the intricate relationship between self-loathing and depression, examining their signs, symptoms, and…
Understanding Reciprocal Changes in ECG: A Comprehensive Guide to Horizontal ST Depression
Electrocardiography (ECG) is a fundamental diagnostic tool in cardiology, providing crucial insights into the heart’s electrical activity. Among the various patterns and changes observed in ECG readings, reciprocal changes play a significant role in identifying and understanding cardiac events. This comprehensive guide delves into the intricacies of reciprocal changes in ECG, with a particular focus…

Understanding Obdurate Depression: Causes, Symptoms, and Treatment Options
Locked in an unyielding grip, obdurate depression challenges millions worldwide, defying conventional treatments and leaving sufferers desperately searching for a glimmer of hope. This persistent and treatment-resistant form of depression can be a formidable adversary, often leaving individuals feeling trapped in a seemingly endless cycle of despair. However, understanding the nature of obdurate depression, its…

Understanding the Link Between COVID-19, Depression, and Anxiety
As the world grappled with an invisible enemy, a silent epidemic of depression and anxiety surged alongside COVID-19, intertwining physical and mental health in unprecedented ways. The global pandemic not only threatened our physical well-being but also took a significant toll on our mental health, creating a complex web of challenges that affected millions of…
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Mental health case studies
Driving up quality in mental health care.
Mental health care across the NHS in England is changing to improve the experiences of the people who use them. In many areas, a transformation is already under way, offering people better and earlier access as well as more personalised care, whilst building partnerships which reach beyond the NHS to create integrated and innovative approaches to mental health care and support.
Find out more through our case studies and films about how mental health care across the NHS is changing and developing to better meet people’s needs.
- Children and young people (CYP)
- Community mental health
- Crisis mental health
- Early intervention in psychosis (EIP)
- Improving access to psychological therapies (IAPT)
- Perinatal mental health
- Severe mental illness (SMI)
- Staff mental health and wellbeing
- Other mental health case studies
- Archived mental health case studies

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

Evaluating the Efficacy of Lumateperone for MDD and Bipolar Depression With Mixed Features

Blue Light, Depression, and Bipolar Disorder

Efficacy of Modafinil for Treatment of Neurocognitive Impairment in Bipolar Disorder

Four Myths About Lamotrigine

Securing the Future of Lithium Research

An Update on Early Intervention in Psychotic Disorders
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

- Children's mental health case studies
- Parenting and caregiving
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Part 2 Lucy’s Story
2.4 Lucy case study 3: Mental illness diagnosis
Nicole Graham
Introduction to case study

Lucy has experienced the symptoms of mental illness during her lifespan; however, it was not until her early twenties that she was formally diagnosed with bipolar affective disorder. In the case study below, we explore the symptomology that Lucy experienced in the lead up to and post diagnosis. Lucy needs to consider her mental illness in relation to her work as a Registered Nurse and as she continues to move through the various stages of adulthood.
Learning Objectives
By the end of this case study, you should be able to:
- Identify and consider the symptoms of mental illness.
- Develop an understanding of contributing biopsychosocial stressors that may exacerbate the symptoms of mental illness as experienced by Lucy.
- Critically analyse the professional, ethical, and legal requirements and considerations for a registered health professional living with chronic illness.
Lucy’s small group of friends describe her as energetic and ‘a party person’. Although she sometimes disappears from her social group for periods of time, her friends are not aware that Lucy experiences periods of intense depression. At times Lucy cannot find the energy to get out of bed or even get dressed, sometimes for extended periods. As she gets older, these feelings and moods, as she describes them, get more intense. She loves feeling high on life. This is when she has an abundance of energy, is not worried about what people think of her and often does not need to sleep. These are the times when she feels she can achieve her goals. One of these times is when she decides to become a nurse. She excels at university, loves the intensity of study, practice and the party lifestyle. Emergency Nursing is her calling. The fast pace, the quick turnaround matches her endless energy. The fact that she struggles to stay focused for extended periods of time is something she needs to consider in her nursing career, to ensure it does not impact negatively on her care.
Unfortunately, Lucy has experienced challenges in her career. For example, her manager often comments on her mental illness after she had openly disclosed her diagnosis. It is challenging for her to hear her colleagues speak badly about a person who presents with mental illness. The stigma she hears directed at others challenges her. She is also very aware that it could be her presenting to the Emergency Department when she is unwell and in need of further support. Lucy is constantly worried that her colleagues will read her medical chart and think she is unsafe to practice.
While the symptoms that cause significant distress and disruption to her life began in her late teens, they intensified after she commenced antidepressant medication after the loss of her child. She subsequently ceased taking them due to side effects. These medications particularly impact on her ability to be creative and reduce her libido and energy. By the time she turns 18, she notices more frequent, intense mood swings, often accompanied by intense feelings of anxiety. During her high periods, Lucy enjoys the energy, the feeling of euphoria, the increased desire to exercise, her engagement with people, and being impulsive and creative. Lucas appreciates her increased libido. However, during these periods of high mood, Lucy also has impaired boundaries and is often flirtatious in her behaviour towards both friends and people she doesn’t know. She also increases her spending and has limited sleep. Lucas is often frustrated by this behaviour, leading to fights. On occasion Lucas slaps her and gets into fights with the people she is flirting with. These periods can last days and sometimes weeks, always followed by depressive episodes.
When she is in the low phases of her mood, Lucy experiences an overwhelming sense of hopelessness and emptiness. She is unable to find the energy to get out of bed, shower or take interest in simple daily activities. Lucas gets frustrated and dismisses Lucy’s statements of wanting to end her life as ‘attention seeking’. Lucy often expresses the desire to leave this world when she feels this way. When Lucas seeks support from the local general practitioner, nothing really gets resolved. The GP prescribes the medication; Lucy regains her desire to participate in life; then stops the medication due to side effects which extend to gastrointestinal upsets, on top of the decrease in libido and not feeling like herself. When Lucy is referred to a psychologist, she does not engage for more than one session, saying that she doesn’t like the person and feels they judge her lifestyle. When the psychologist attempts to explore a family history of mental illness, Lucy says no- one in her family has it and dismisses the concept.
The intense ups and downs are briefly interrupted with periods of lower intensity. During these times, Lucy feels worried about various aspects of her life and finds it challenging to let go of her anxious thoughts. There are times when Lucy has symptoms like racing heart, gastrointestinal update and shortness of breath. She spends a great deal of time wanting her life to be better. Her desire to move on from Lucas and to start a new life becomes more intense. Lucy is confident this is not a symptom of depression; it is just that she is unhappy in her relationship. Lucy starts to consider career options, feeling that not working affects her lifestyle, freedom and health. As she explores different options on the internet, Lucy comes across a chat room. Using the chat name ‘Foxy Lady 20’, she develops new friendships. She finds herself talking a lot with a man named Lincoln who lives on the Gold Coast.

After a brief but intense period talking with Lincoln online, Lucy abruptly decides to leave Lucas and her life in Bundaberg to move in with Lincoln. Lincoln, aged 26, 5 years older than Lucy, owns a modest home on the Gold Coast and has stable employment at the local casino. Their relationship progresses quickly and within a month Lincoln has proposed to Lucy. They plan to marry within 12 months.
Lucy is now happy with her life and feels stable. She decides to pursue a degree in nursing at the local university. Lucy enrols and makes many new friends, enjoying the intensity of study and a new social scene. Her fiancé Lincoln also enjoys the social aspects of their relationship. During university examination periods, Lucy experiences strong emotions. At the suggestion of an academic she respects, she makes an appointment with the university counselling service. After the first 3 appointments, Lucy self-discovers, with the support of her counsellor, that she might benefit from a specialist consultation with a psychiatrist. She comes to recognise that her symptoms are not within the normal range experienced by her peers. Lincoln is incredibly supportive and attends the appointments with Lucy, extending on the information she provides. Lucy reveals information about her grandmother, who was considered eccentric, and known for her periods of elevated mood and manic behaviour. The treating psychiatrist suggests Lucy may be living with bipolar affective disorder and encourages her to trial the medication lithium.
Lucy does not enjoy the side effects of decreased energy, nausea and feeling dazed and ceases taking the lithium during the university break period. This causes Lucy to again experience an intense elevation of her mood, accompanied by risk-taking behaviours. Lucy goes out frequently, nightclubbing and being flirtatious with her friends. She becomes aggressive towards a woman who confronts Lucy about her behaviour with her boyfriend in the nightclub. This is the first time Lucy exhibits this type of response, along with very pressured speech, pacing and an inability to calm herself. The police are called. They recommend Lucy gets assessed at the hospital after hearing from Lincoln that she has ceased her medication. Lucy is admitted for a brief period in the acute mental health ward. After stabilising and recommencing lithium, Lucy returns to the care of her psychiatrist in the community. The discharge notes report that Lucy had been previously diagnosed with bipolar disorder, may also be experiencing anxiety related symptoms, and have personality vulnerabilities.
Lucy is in the final year of her university studies when she has a professional experience placement in the emergency ward. Lucy really enjoys the fast pace, as well as the variety of complex presentations. Lucy feels it matches her energy and her desire for frequent change. After she completes her studies, Lucy applies and is successful in obtaining a position at the local hospital. Throughout her initial graduate year, Lucy balances life with a diagnosis of mental illness as well as a program of her own self-care. She finds the roster patterns in particular incredibly challenging and again becomes unwell. She goes through a period of depression and is unable to work. During this period, Lucy experiences an overwhelming sense of hopelessness and considers ending her life. Again, she requires a higher level of engagement from her treating team. Lucy agrees she is not fit to work during this time and has a period of leave without pay to recover. She has disclosed to her manager that she has been diagnosed with a mental illness and later discusses how shift work impacts her sleep and her overall mental wellbeing.
Over time, Lucy develops strategies to maintain wellness. However, she describes her relationship with the Nursing Unit Manager as strained, due to her inability to work night shift as her medical certificate shows. Lucy says she is often reminded of the impact that her set roster has on her colleagues. Lucy also feels unheard and dismissed when she raises workplace concerns, as her manager attributes her feelings to her mental health deteriorating. Lucy has a further period when her mental health deteriorates. However, this time it is due to a change in her medication.
As Lucy and Lincoln have a desire to have a child, Lucy was advised that she cease lithium in favour of lamotrigine, to reduce the risk of harm to the baby. Lucy ceases work during the period when her mental health deteriorates during the initial phase of changing medication. Lucy recommences lithium after she ceases breastfeeding their son at 4 months, with good effect and returns to work.
Case study questions
- Consider the symptoms that Lucy experiences and indicate whether they align with the suggested diagnosis.
- Identify the biopsychosocial contributing factors that could impact mental health and wellness.
- Review and identify the professional disclosure requirements of a Registered Nurse who lives with mental illness in your local area.
- Identify self-care strategies that Lucy or yourself as a health professional could implement to support mental health and wellbeing.
Thinking point
Sometimes people do not agree with a diagnosis of mental illness, which can be incorrectly labelled as ‘denial’ by health professionals. It is possible that the person is unable to perceive or be aware of their illness. This inability of insight is termed anosognosia (Amador, 2023). The cause of anosognosia in simple terms can be due to a non-functioning or impaired part of the frontal lobe of the brain, which may be caused by schizophrenia, bipolar disorder or other diseases such as dementia (Kirsch et al., 2021).
As healthcare workers will likely care for someone who is experiencing anosognosia, it is important to reflect on how you may work with someone who does not have the level of insight you would have hoped. Below is a roleplay activity whereby you can experience what it might be like to communicate with someone experiencing anosognosia. Reflect on your communication skills and identify strategies you could use to improve your therapeutic engagement.
Role play activity – Caring for a person who is experiencing anosognosia
Learning objectives.
- Demonstrate therapeutic engagement with someone who is experiencing mental illness
- Identify effective communication skills
- Reflect on challenges and identify professional learning needs
Resources required
- Suitable location to act out scene.
- One additional person to play the role of service user.
Two people assume role of either service user or clinician. If time permits, switch roles and repeat.
- Lucy has been commenced on lithium carbonate ER for treatment of her bipolar disorder.
- Lucy is attending the health care facility every week, as per the treating psychiatrist’s requests.
- The clinician’s role is to monitor whether Lucy is experiencing any side effects.
Role 1 – Clinician
- Clinician assumes role of health care worker in a health care setting of choice.
- Lucy has presented and your role is to ask Lucy whether she is experiencing any side effects and whether she has noticed any improvements in her mental state.
Role 2 – Lucy who lives with bipolar
- Lucy responds that she does not understand the need for the tablets. She also denies having a mental illness. Lucy says she will do what she is told, but does not think there is anything wrong with her. Lucy thinks she is just an energetic person who at times gets sad, which she describes as ‘perfectly normal.’ Lucy is not experiencing any negative side effects, but says she would like clarification about why the doctor has prescribed this medication.
Post role play debrief
Reflect and discuss your experiences, both as Lucy and as the clinician. Identify and discuss what was effective and what were the challenges.
Identify professional development opportunities and develop a learning plan to achieve your goals.
Additional resources that might be helpful
- Australian Prescriber: Lithium therapy and its interactions
- LEAP Institute: The impact of anosognosia and noncompliance (video)
Key information and links to other resources
Fisher (2022) suggests there are large numbers of health professionals who live with mental illness and recognise the practice value that comes with lived experience. However, the author also notes that as stigma is rife within the health care environment, disclosing mental illness can trigger an enhanced surveillance of the health professional’s practice or impede professional relationships (Fisher, 2022).
It is evident that the case studies derived from Lucy’s life story are complex and holistic care is essential. The biopsychosocial model was first conceptualised in 1977 by George Engel, who suggests it is not only a person’s medical condition, but also psychological and social factors that influence health and wellbeing (Engel,2012).
Below are examples of what you as a health professional could consider in each domain.
- Biological: Age, gender, physical health conditions, drug effects, genetic vulnerabilities
- Psychological: Emotions, thoughts, behaviours, coping skills, values
- Social: Living situation, social environment, work, relationships, finances, education
Developing skills through engaging in reflective practice and professional development is essential. Each person is unique, which requires you as the professional to adapt to their particular circumstances. The resources below can help you develop understanding of both regulatory requirements and the diagnosis Lucy is living with.
Organisations providing information relevant to this case study
- Rethink Mental Illness: Bipolar disorder
- Australian Health Practitioner Regulation Agency (AHPRA): Resources – helping you understand mandatory notifications
- Australian Health Practitioner Regulation Agency (AHPRA): Podcast – Mental health of nurses, midwives and the people they care for
- Black Dog Institute: TEN – The essential network for health professionals
- Borderline Personality Disorder Community
- National Institute of Mental Health (NIMH): Anxiety disorders
Case study 3 summary
In this case study, Lucy’s symptoms of mental illness emerge in her teenage years. Lucy describes periods of intense mood, both elevated and depressed, as well as potential anxiety-related responses. It is not until she develops a therapeutic relationship with a university school-based counsellor that she realises it might be beneficial to engage the services of a psychiatrist. After she is diagnosed with bipolar affective disorder she engages in treatment. Lucy shares her experience of both inpatient and community treatment as well as her professional practice requirements in the context of her mental illness.
Amador, X. (2023). Denial of anosognosia in schizophrenia. Schizophrenia Research , 252 , 242–243. https://doi.org/10.1016/j.schres.2023.01.009
Engel, G. (2012). The need for a new medical model: A challenge for biomedicine. Psychodynamic Psychiatry, 40 (3), 377–396. https://doi.org/10.1521/pdps.2012.40.3.377
Fisher, J. (2023). Who am I? The identity crisis of mental health professionals living with mental illness. Journal of Psychiatric and Mental Health Nursing . Advance online publication. https://doi.org/10.1111/jpm.12930
Kirsch, L. P., Mathys, C., Papadaki, C., Talelli, P., Friston, K., Moro, V., & Fotopoulou, A. (2021). Updating beliefs beyond the here-and-now: The counter-factual self in anosognosia for hemiplegia. Brain Communications , 3 (2), Article fcab098. https://doi.org/10.1093/braincomms/fcab098
Case Studies for Health, Research and Practice in Australia and New Zealand Copyright © 2023 by Nicole Graham is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book

How these organizations are leading in making employee mental health a priority
Learn more from these case studies of successful leaders promoting mental health among workers.
- Business and Industry
- Mental Health
- Applied Psychology

Psychological evidence suggests employee mental health is a critical component for organizational functioning and success. As with any positive business outcome, promoting mental health among your workers often requires a significant investment of time and resources.
If you’re dedicated to equipping your employees and organization to thrive but you don’t know exactly where to begin your efforts, learn from these organizations, who have taken steps to prioritize employee mental health.
American Psychological Association
APA’s science-led, empathy-based culture has always informed its approach to employee mental health. To ensure employees can access psychological support necessary to thrive in their personal and work lives, APA provides a robust package of mental health benefits.
Employees can access mental health care for a low copay through APA’s insurance provider or through an additional mental health care insurer that enables employees to access any mental health professional for only a $20 copay (with the exception of employees enrolled in a high-deductible Health Savings Account plan, to which APA contributes).
In addition, APA’s employee assistance program provides employees and their household members with free, confidential, 24/7 support to help with personal or professional matters that may interfere with work or family responsibilities.
APA found new opportunities to build on its ongoing dedication to employees’ mental health and well-being during the Covid -19 pandemic, starting by ramping up internal communications that instilled a much-needed sense of belonging during the transition to remote work and continues to solicit employee feedback that informs organizational policies, programs, and procedures. For example, the daily staff e-blast, APA Today , is now shared in video and text format, staff share fun personal photos through questions of the week, staff are given a few extra days off per year for strengthening mental health (in addition to a generous PTO plan), and staff can share with each other socially through themed Microsoft Teams channels and Coffee Connections meetups.
Along with considering employees’ needs and interests, new initiatives also weave in the latest psychological science about what employees and organizations need to thrive. Additionally, APA uses a cross-departmental approach to implement changes, in which experts in the areas of human resources, psychological science, employee well-being, as well as C-suite leaders, work together to communicate about employee and organizational needs and implement initiatives.
APA conducts regular “pulse” polls to survey employees about the level of support they feel from their managers and the organization and what they need to feel more supported, from computer hardware to more flexible working hours. Employees also have an opportunity to hear updates from and share concerns directly with APA’s CEO in a biweekly, virtual chat.
To address the multiple layers of stressors employees are facing, APA initiated multiple staff conversations around racism and related current events, inviting experts to speak about the issues and how to take action. Employee resource groups were formed to support employees and provide them with a community.
APA also assembled a working group to use lessons learned during the pandemic and employee feedback to plan the future of the organization’s workplace. Most employees (75%) participated, sharing their perspectives about the future of work via focus groups, conversations with leadership, pulse polls, surveys, or other forums.
In response, APA is evolving its concept of the workplace rather than simply returning to prepandemic office norms: APA established a flexible work policy that allows employees to move outside the Washington, D.C. area to one of 40 approved states, maintaining their current salary and same level of employee benefits no matter where they move. In response to employees’ desires to improve their work-life harmony, APA also implemented a Meet with Purpose campaign that encourages science-based best practices for all internal meetings. Each meeting needs to have a designated agenda, start on the hour or half-hour, and last for 25 or 50 minutes to ensure employees have breaks between meetings to tend to personal or family needs. Employees are also encouraged to consider and communicate to the team about whether video is required for a meeting or if it can be audio-only, since back-to-back video meetings can have a negative impact on employee well-being.
Blackrock, an international investment management organization, also recognized the urgency of prioritizing employee well-being during the Covid -19 pandemic. As the organization pivoted to remote or socially distanced work, it conducted periodic employee surveys to gather feedback that would inform new policies and procedures.
For example, Blackrock extended its health care coverage to ensure employees working out-of-state or out of the country, along with their families, could access health care. To better support employees’ mental well-being, Blackrock onboarded a new employee assistance provider to help deliver a range of new mental health benefits, including care navigation, easy online appointment booking, virtual care delivery, and a high-quality network of providers integrated into its medical plans. The firm also offered a company-paid subscription to the Calm app and launched a peer network of Mental Health Ambassadors.
To support employees with family responsibilities, the organization expanded the number of company-paid back-up care days, implemented more flexible work-from-home schedules, and encouraged the use of the existing flexible time off policy that allows all employees—regardless of title or tenure—access to paid time off as needed. To encourage employee collaboration, Blackrock also created online forums for sharing ideas and resources to support parenting and childcare.
Building on psychological research about the importance of manager support, Blackrock launched a series of enablement sessions to train supervisors in keeping their teams informed and motivated. The firm also created an intranet resource hub to streamline internal communications, so employees can quickly access information they need to do their jobs well and ask for help as needed.
YMCA of the USA
YMCA of the USA, (Y-USA), the national resource office for the nation’s YMCAs, pivoted to fully remote work in March 2020. Recognizing the increased need for social and emotional support, YMCA immediately began heavily promoting its employee assistance program (EAP) services through frequent newsletters, emphasizing free access to confidential services for employees’ entire families.
To learn more about additional unmet needs, Y-USA leaders also utilized pulse surveys in which employees rate various areas of well-being. Using this feedback, leaders made distinct efforts to implement changes. For example, when one survey found that many work-from-home employees needed additional office equipment to perform their jobs well, the organization provided it. Another survey made clear that employees weren’t ready to return to in-office work in 2021, so YMCA changed its plans and extended its flexible work policies.
In response to employee concerns about lack of camaraderie, Y-USA created weekly virtual Coffee Chats to connect employees with one another and Tech Tuesdays, an opportunity for employees to learn or refresh tech skills, ask tech questions, and learn about efficient hybrid work practices.
Biannual culture surveys conducted by a third party also guide Y-USA’s practices. To continue to ensure employee feedback is carefully implemented, Y recently formed a Culture Counsel of volunteer employees, who help review areas for improvement and discuss possible changes. After learning of employees’ continued desire for work flexibility, organization leaders extended the work-from-home practice, encouraging employees to visit the office as needed.
In addition, Y-USA convened a Mental Health Thought Leader Cohort, made up of local Y staff who curate and package “To Go” mental health kits, a grab and go resource for local Y leaders to implement with staff, such as “Dinner Table Resilience” which offers short videos, tools, and strategies for Y-USA staff and members to use at the dinner table with families to build resilience skills.
F5 Networks
F5 Networks, a large technology company in the Seattle area, also uses employee surveys extensively to promote its “human-first, high-performance” culture. Along with regularly surveying existing employees, leaders also seek input from candidates who weren’t hired, employees who left the company, and individuals who left and came back.
After learning how growth opportunities led to employee retention, F5 developed a company-wide mentorship program, increased its budget to allow employees to pursue continued education in their field, and created quarterly learning days on which employees have no internal meetings but instead focus on learning.
In response to an increased need for time off—without the stress of returning to an inbox full of emails—F5 also launched company-wide quarterly wellness weekends allowing all employees an extra paid consecutive Friday and Monday off.
Ongoing survey data suggest positive business outcomes. F5 employees report feeling more refreshed and ready to tackle projects when they return to work after time off, for example. In general, F5 staffers report feeling supported by their managers and the organization as a whole.
On its U.S. medical plans, F5 also removed out-of-network restrictions for psychotherapy to ensure employees could connect with diverse therapists and therapists not accepting insurance. Rather than paying a large deductible and being partially reimbursed for services, employees on the Preferred Provider Organization plan pay a $15 copay for any therapist (plus any additional fees if the therapist charges more than what the benefits cover). Additionally, F5 increased its EAP therapy visit max from three to five annual sessions per employee.
Ernst & Young
The consulting firm Ernst & Young (EY) offers a full suite of mental health and well-being resources for employees and their families. In addition to EY’s health care plan that includes mental health benefits, EY has an internal team of clinicians that conduct presentations and interactive sessions promoting mental health in the organization.
EY also works with a private vendor to offer up to 25 psychotherapy sessions for each employee and each person in their household per year. Because employees’ family lives can impact their well-being and work performance, the firm extended the mental health benefit to include all family members in the household including children, domestic partners, and relatives, regardless of their age or whether they’re on the employees’ health care plan. The network of clinicians represent a variety of backgrounds that can meet employees’ diverse needs. They use evidence-based psychotherapy practices to ensure the best outcomes.
EY recognizes the role of psychological concepts like resilience in staving off stress and burnout. EY allows employees to access mental health coaching sessions to prevent issues that could interfere with well-being and work performance and increase overall well-being in their daily lives. Data suggest employees working with a mental health coach or therapist saw an 85% improvement or recovery from the initial reason they sought care.
For people who would rather use digital tools, EY offers a positive psychology-informed app that educates employees about coping with stress and promoting resilience through articles and activities. Similarly, a digital sleep resource provides personalized guidance for improving sleep. On average, people using this digital tool are getting an average of four more hours of sleep per week.
An internal initiative called We Care educates employees on important topics such as recognizing signs of mental health concern and addiction and best practices for offering support. Employees share their own mental health stories to destigmatize the topic. To encourage time away from work, EY also reimburses employees for vacations and travel; the company also reimburses for physical wellness-related activities, such as gym memberships, fitness equipment, and even mattresses.
National League of Cities
The National League of Cities (NLC), the nonprofit advocate for municipal governments, is committed to supporting and nurturing a work culture that prioritizes the mental and physical health of its employees. It has done so through several targeted approaches. Like many organizations, NLC moved its entire 130-person Washington, D.C.-based staff to virtual work at the start of the pandemic. Employees were encouraged to maximize and leverage flexible schedules. As the pandemic evolved, NLC developed a hybrid model in which staff could continue to work remotely and also use the NLC offices for collaboration and other onsite work.
The organization’s health insurance plan covers mental health services on par with its coverage of physical health. NLC subsidizes coverage for employees and family members, including access to licensed mental health providers who offer services via telehealth. NLC also offers an EAP, which it promotes regularly (and even more frequently during the pandemic) to employees.
At the start and during the height of the pandemic, NLC gathered employee input. NLC surveyed employees in 2020 and 2021 to learn about their telework experience and hear their return-to-office concerns and suggestions. More than 90% of the staff participated. To determine the cultural norms for hybrid work, NLC used a dispersed decision-making method that employed focus groups to gather ideas from every employee in the organization. One resulting cultural norm the company has established, is that employees are highly encouraged to use their paid time off from work to unplug and refresh.
American Public Health Association
The American Public Health Association (APHA), a Washington, D.C.-based organization for public health professionals, champions the health of all people and all communities.
When Covid -19 struck, APHA’s staff worked harder than ever to develop essential Covid -19 resources for members. At the same time, employees were experiencing the loss of loved ones, isolation, racial inequity, financial burden, family job loss, and the need to provide around-the-clock family support. These strains caused a real need for mental health services and support.
How does APHA support its staff? APHA’s EAP, a free service for staff, offers three immediate counseling sessions with a licensed mental health professional. Staff can access EAP professionals 24 hours a day, 7 days a week. The EAP can also provide legal assistance, online will preparation, financial tools and resources, help addressing substance misuse and other addictions, as well as resources for dependent and elder care.
APHA’s mental health services through their insurer, CareFirst, are tailored for short-term and long-term mental health matters. Employees and covered family members seeing in-network professionals have no copayments and many of the providers offer telehealth visits from 7 a.m.–11 p.m. Eastern time, 7 days a week. The average therapy appointment is about 45 minutes. Psychiatrists are also available to help with mental health conditions requiring medication management.
Staff are encouraged to voice their needs. APHA instituted several internal services and activities to improve how management listened and responded to employee needs. “Courageous Conversation,” started after the George Floyd and Black Lives Matter protests, are discussions with peers in an honest and safe environment about experiences that relate to race. During the height of the Covid -19 pandemic, Half-day Fridays gave staff a mental health break from the stress of having inseparable work and home space. A mindfulness video APHA shared with staff reminded them to be present in the moment, take a breath, and tackle one thing at a time. While working from home, No Meeting Tuesday Afternoons ensured staff had a block of time to focus on one task at a time as they navigated the stresses of the pandemic and increased virtual meetings. Optional forums and surveys allowed staff to communicate their mental health needs and challenges. Complimentary Stretch Class—a free monthly service—gives staff a 45-minute break to relieve stress and tension.

5 ways to improve employee mental health

Supporting employees’ psychological well-being

Striving for mental health excellence in the workplace
Acknowledgments
APA gratefully acknowledges the following contributors to this content.
- Tammy D. Allen, PhD, professor of industrial and organizational psychology at the University of South Florida
- Christopher J. L. Cunningham , PhD, professor of industrial-organizational and occupational health psychology at University of Tennessee at Chattanooga
- Gwenith G. Fisher, PhD, associate professor of occupational health psychology at Colorado State University
- Leslie Hammer , PhD, professor of occupational health psychology at Oregon Health & Science University and codirector of the Oregon Healthy Workforce Center
- Jeff McHenry, PhD , principal at Rainier Leadership Solutions and faculty member at USC Bovard College
- Jon Metzler, PhD, director of human performance at Arlington, Virginia-based Magellan Federal
- Fred Oswald, PhD , professor of industrial and organizational psychology, Organization and Workforce Laboratory, Rice University
- Dennis P. Stolle, JD, PhD, senior director of APA’s Office of Applied Psychology
- Ryan Warner , PhD, founder and chief executive officer of RC Warner Consulting in Albuquerque, New Mexico
Make a commitment to mental health excellence in the workplace
Organizational leaders are well-positioned to influence a positive culture shift and normalize mental health in the workplace.
You may also like

- HR Most Influential
- HR Excellence Awards
- Advertising
Search menu
Rachel Muller-Heyndyk
View articles
Case study: Mental health support led by the individual

Monzo wanted to ensure a range of help is available to all employees, wherever and whenever they want it
The organisation
Formed in 2015, Monzo started as a prepaid card that could be topped up via an app to enable users to make free cash withdrawals abroad. It quickly built up a strong following, and after being given the green light by the Financial Conduct Authority became a fully-fledged banking brand in 2017. Its prepaid card system has since closed, with users upgraded to its current account. Last year Monzo was named a ‘best buy’ for current accounts by not-for-profit co-operative group Ethical Consumer.
The problem
Thanks to the efforts of campaigners, businesses and charities over recent years, mental health in the workplace is now recognised as a pressing concern for employers. But while there’s far more transparency around mental health than even a few years ago, substantial progress on supporting staff has been slow in some quarters.
Research from Business in the Community in September found that of 4,000 employees surveyed, 39% had experienced poor mental health due to their work, while 33% of those with mental health problems felt ignored. Even more worryingly, 9% had been subjected to disciplinary action, demotion or dismissal after disclosing their mental health issues.
Monzo’s head of people Tara Mansfield is determined that nothing like this happens at her company, and that mental health support isn’t treated as an afterthought.
“When it comes to poor mental health you know that it’s something everyone has [at some point], and there will inevitably be people who are struggling in your team,” she says.
Mental health support for staff makes sense both ethically and strategically for organisations, she adds.
“We’re an ethical company. I’m really proud that we’re able to offer advice on financial wellbeing to our customers, and act in a responsible fair way. For me it’s about making sure that we apply the same values to the workforce.”
Mansfield knew that any support on offer at Monzo needed to be as holistic as possible, because poor mental health is experienced differently by each individual.
“If you just focus on one area of mental health there’s always going to be a risk that you alienate someone,” she explains.
“There are lots of people who will go through a crisis at some point or a difficult challenge, and they might have increased levels of anxiety. There are also people who have a long-term diagnosed health condition and need more ongoing support, and there are others who might have a co-morbid mental health condition alongside being neurodiverse.”
Only offering one kind of mental health support would be short-sighted from a business point of view as it could alienate staff who require something different, she adds.
“It would be wrong for employers to say ‘we can help these people, but not those dealing with more serious issues’ – that’s a really risky approach. While employers can’t always directly improve people’s mental health, all employers can make it clear that they are open to supporting everyone.”
Crucially, however, there should always be boundaries, Mansfield says.
“We didn’t want people to feel as though we were interfering with their lives or dictating what they should do with their mental health,” she stresses. “Most people don’t want that much direct input from their employers. We just want people to have as many options as possible so they feel they’re in control of their wellbeing.”
So the challenge was to create a comprehensive strategy on mental health support at work while empowering individuals to manage their own wellbeing in a way that best suits them.
Organisations that are serious about mental health, and have the funds, must put their money where their mouths are, says Mansfield.
“We offer private healthcare to all employees, and mental health comes under that. Everyone is able to access a therapist if they need it,” she says.
The key is making sure employees know what support is available.
“We always make sure that people know that this is an option for them and make it very clear that mental health is just as important as what’s going on physically,” Mansfield adds. “It can be easy to forget that this is an option, so we tell everyone that this is something they can do regardless of if they come to us with an issue.”
Monzo has also trained 45 employees as mental health first aiders.
“We wanted to make sure that people have immediate help available. Mental health first aiders often really enjoy the process too, and feeling like they’re in a position where colleagues can come to them if they’re struggling,” she says.
However, it’s important to recognise that not everyone will necessarily want to turn to their employer or go to see a counsellor when something is wrong, Mansfield points out. Which is where mental wellbeing app Spill comes in.
Spill matches employees to one of 50 therapists who are reachable via text on the app. According to Spill 80% of people who use the app have never seen a therapist before. So Monzo’s use of Spill fits neatly with its aim of helping people with personal challenges early on before they develop into more serious problems.
“The great thing about Spill is that it’s completely external. It gives people that outside help of allowing them to talk to someone who is completely outside of their situation in quite a casual way,” says Mansfield. “The more help you can offer at an earlier stage, the better. It’s been a great way to help someone through a crisis before it develops into an illness.”
Visibility is also important. Indeed the company literally has its ethos towards mental health plastered on its walls.
“We’ve put posters up all around our offices with our key messages. They let people know that it’s alright to admit to making a mistake, to asking for a mental health day, and speaking up if you don’t understand something,” says Mansfield.“We’ve also got some tips on what people can do – from taking some fresh air, to being kind to others and bringing their dog to the office.”
Monzo’s all-encompassing approach to championing good mental health has paid off, both in terms of supporting current staff and attracting new talent, says Mansfield.
She believes the success of Spill is a good example of how sometimes it’s worth trying something new when it comes to wellbeing.
“People really weren’t sure about Spill initially. There’s understandably a lot of scepticism with tech companies using people’s data at the moment, and people will obviously feel particularly cautious about sharing details of their mental health,” she reveals.
However, after the HR team stressed that the app is entirely separate from the organisation – and entirely confidential – employees were slowly won over. A third of Monzo’s employees have now signed up for Spill. And of those who do use it 70% do so regularly.
“Those who have approached us about Spill have found it so beneficial. They’ve said it’s really helped them to develop a sense of self-awareness, and where they have ups and downs,” she says.
The smaller details of the strategy have made all the difference, reports Mansfield: “Our workforce is growing at an enormous speed. There were 42 people when I joined Monzo in 2017. Now there are more than 1,000, so we have newcomers pretty much every week.
“What’s been really great to hear is people saying ‘I noticed the posters as soon as I walked in, it’s so great to see a company that actually takes mental health seriously’. That’s what it’s all about for us: enabling people to start those conversations.”
This piece appeared in the December 2019 print issue. Subscribe today to have all our latest articles delivered right to your desk
Further reading

Case study: WHSmith's approach to mental health

Mental health support at HEINEKEN

Building the business case for action on mental health

Case study: keeping health practitioners healthy

Conflict at work linked to mental health issues

We test... Mental Health First Aid training

Millennial mental health: A particular problem?

Case study: Early wage access at Camden Town Brewery
Study: Bad COVID lockdown memories faded in a year, but kids' mental health worsened

Although memories of COVID-19 lockdowns in Danish school children dimmed in detail and emotion from 2020 to 2021, their mental health remained poor, particularly among girls, Aarhus University–led researchers report in Child Development .
The researchers asked 247 students to write about their memories of the first lockdown and their psychological symptoms three times from June 2020 to June 2021. The students, recruited from five public and private schools, had a median age of 11.9 years.
Denmark closed schools from March 11 to April 17, 2020, for younger students and to May 18 for older ones. A second closure occurred from December 17, 2020, to May 6, 2021. Other measures taken were restaurant closures, gathering bans, physical-distancing policies, and work-from-home orders.
Older students, teen girls most emotional
Students whose memories were more negative and contained more COVID-19 information fared worse over time, which may mean that they integrated lockdown experiences more profoundly in their development and sense of self, the researchers said.
Only by examining the content of all these different memories will we know if these results reported here are specific to the first period of the pandemic... or if instead our patterns of results extend to other forms of remembering and imagining pandemic-related experiences.
Tirill Fjellhaugen Hjuler, PhD
Older students and adolescent girls were the most emotional in their memory descriptions, which may show that adolescents better integrate memories into their meaning-making narratives than younger students. And adolescent girls, the authors said, may be more likely than boys to elaborate on memories of COVID-19 and their emotional well-being.
The researchers called for research on the association between children's tendency to include semantic (eg, facts about COVID-19) rather than episodic (eg, interactions with family) in their recall of significant events and their adjustment.
"Only by examining the content of all these different memories will we know if these results reported here are specific to the first period of the pandemic, when radical changes in children's and adolescents' lives occurred, or if instead our patterns of results extend to other forms of remembering and imagining pandemic-related experiences," lead author Tirill Fjellhaugen Hjuler, PhD, of Aarhus University, said in a news release from the Society for Research in Child Development, publisher of Child Development .
Adjuvanted flu vaccine protects better than high-dose version in at-risk older adults, US data show

A study of patient data from the 2019-20 US flu season found that the MF59-adjuvanted flu vaccine was more effective than the high-dose flu vaccine at preventing serious flu complications in older adults with risk factors, researchers reported late last week in Open Forum Infectious Diseases.
The MF59-adjuvanted trivalent influenza vaccine (aTIV) and the high-dose trivalent influenza vaccine (HD-TIV) are both designed for adults age 65 and older, who are at serious risk from serious flu complications. An adjuvant is an immune-boosting agent added to vaccines.
Previous studies have found the two vaccines to have similar effectiveness in older adults, including those who have at least one underlying health condition known to increase their risk of experiencing severe flu. But there is limited research on how multiple concurrent high-risk conditions affect vaccine effectiveness.
aTIV more effective in adults with multiple risk factors
Using electronic health record data linked with pharmacy and medical claims, researchers estimated the relative vaccine effectiveness (rVE) in 1,115,725 aTIV recipients and 2,561,718 HD-TIV recipients from August 2019 through January 2020. The primary measure was prevention of influenza-related medical encounters (IRMEs). The secondary outcome was outpatient IRME and flu- and pneumonia-related hospitalizations.
Among older adults with risk factors for complications, aTIV was more effective than HD-TIV at preventing any IRME, with an rVE of 12.5% (95% confidence interval [CI], 10.0% to 15.0%) for adults with 1 or more risk factor, 18.4% (95% CI, 13.7% to 22.8%) for adults with 1 or 2 risk factors, and 10.4% (95% CI, 7.4% to 13.3%) for adults 3 or more risk factors. No difference in rVE was observed among older adults with no risk factors.
The same trends were observed for the secondary outcomes of outpatient IRMEs and flu- or pneumonia-related hospitalizations.
The study authors suggest the broader immune response provide by the MF59 adjuvant may account for the higher vaccine effectiveness observed among the most vulnerable in the population study, but say further research is needed to investigate how the immune response generated by aTIV contributes to overall vaccine effectiveness across populations with different risk profiles.
CDC issues Oropouche virus alerts for clinicians and travelers
The Centers for Disease Control and Prevention (CDC) recently posted a Health Alert Network notice for Oropouche virus following reports of expanded disease activity in Cuba and parts of South America, which has so far resulted in 11 imported US cases.
.jpg)
Oropouche virus, spread by certain biting midges and possibly some types of mosquitoes, has recently been linked to severe fetal outcomes, including death and congenital abnormalities. The CDC said travel-related cases have been reported in the United States and Europe among some people who visited Brazil and Cuba.
Though more cases from more countries are expected as surveillance and testing increase, no local transmission has been reported in any US state or territory, the CDC said.
The CDC urged clinicians to consider Oropouche virus in people who traveled to areas with confirmed or suspected cases within 2 weeks of initial symptoms and rule out dengue infection. It also asked clinicians to be aware of the risk of vertical transmission and to monitor pregnancies in women with confirmed Oropouche infections.
Travel notice for pregnant women considering Cuba travel
In a related development the CDC issued a level 2 travel notice regarding Oropouche virus for people planning travel to Cuba. It had previously issued a level 1 notice for travel to South America.
The CDC recommended that clinicians warn pregnant women considering travel to affected areas about the risk to the fetus and that all visitors practice precautions.
So far, Oropouche virus cases have been reported in 9 of Cuba's 15 provinces. The CDC urged pregnant women to reconsider nonessential travel to Cuba and if unavoidable to strictly follow the CDC's prevention recommendation s, which include using insect repellent, window and door screens, and fans when outdoors to blow biting midges away.
Salmonella outbreak linked to pet turtles sickens at least 51 people in 21 states
The US Centers for Disease Control and Prevention (CDC) has announced a Salmonella outbreak linked to contact with small pet turtles, similar to several other outbreaks linked to the animals in previous years.

In the latest outbreak, the CDC has received reports of 51 illnesses from 21 states, with 23 patients hospitalized. No deaths have been reported.
Two subtypes are tied to the outbreak, Salmonella Stanley (38) and Salmonella Poona (13). Illness onsets range from August 20, 2023, through July 9, 2024. More than a third of the patients are children younger than 5 years old.
Of 41 sick people who were interviewed, 27 (66%) had contact with pet turtles. Of 23 people who reported the size of the turtles, 21 said they had contact with turtles with shells less than 4 inches long. A similar outbreak in 2023 resulted in at least 80 illnesses in 24 states.
Testing of turtles identifies outbreak strain
Genetic sequencing of Salmonella samples from sick patients suggests that their illnesses are closely related, hinting at the same infection source. Also, California officials collected a sample from a sick patient's turtle in June, and tests revealed Salmonella Poona that was closely related to bacteria that infected humans. Testing of turtle and environmental samples from Illinois also yielded the Salmonella Poona outbreak strain.
The patient from California had purchased the turtle from a street vendor, and the person from Illinois had gotten the turtle at a souvenir shop. A survey of sick patients found that people had bought the turtles at those and other outlets, which also included online retailers.
The CDC urged people not to buy turtles with shells less than 4 inches long due to the well-known infection risk, and it noted that there's federal ban on the sale and distribution of small turtles as pets.
Quick takes: WHO mpox panel report, Eastern equine encephalitis, FDA OKs at-home syphilis test
- When the World Health Organization (WHO) mpox emergency committee met on August 14 to discuss the quickly evolving developments in Africa, it unanimously recommended that the situation warrants a public health emergency of international concern (PHEIC). In accepting the group's recommendation the same day, the WHO's director-general said the group would soon release its temporary recommendations and full report for countries, which the WHO published today . The recommendations cover but are not limited to the Democratic Republic of the Congo, Burundi, Kenya, Rwanda, and Uganda. Among several recommendations, the emergency committee urged countries to prepare for mpox vaccination for emergency response by convening immunization advisory groups. It also emphasized the importance of standing recommendations that the WHO issued when it called the end of the earlier PHEIC for the global spread of the clade 2 virus.
- Massachusetts and Vermont last week reported their first human Eastern equine encephalitis (EEE) cases of the year, according to notifications from the state health departments. The Massachusetts Department of Public Health said its case, the first since 2020, involved a man in his 80s who was exposed in Worcester County. Meanwhile, the Vermont Department of Health reported an EEE illness in a man in his 40s from Chittenden County. He was hospitalized in the middle of July, but has now been released. The case marks Vermont's first since 2012. EEE is a rare mosquito-borne illness that can lead to severe neurologic complications. Transmission is most common in and around freshwater hardwood swamps in Atlantic and Gulf Coast states and in the Great Lakes region. In its most recent update on August 13, the Centers for Disease Control and Prevention said it had received a report of only one case so far this season, involving a patient from New Jersey.
- The Food and Drug Administration on August 16 announced that it has approved the first at-home over-the-counter test for syphilis, which detects human antibodies to Treponema pallidum in human blood. The test, made by NOWDiagnostics, produces a result in 15 minutes and is designed to alert the user for a potential follow-up, which would require confirmation testing by a healthcare provider. Syphilis cases in the United States have been steadily rising since 2018, with congenital cases up even more sharply.
In case you missed it
This week's top reads, sweden reports first clade 1 mpox case outside of africa as nih shares disappointing tpoxx results.
The patient sought medical attention in Stockholm but had recently visited Africa.
New studies estimate long-COVID rates, identify risk factors
About 34% of infected postmenopausal women had symptoms for 8 weeks or more, while 61% of survivors in a second study had symptoms at 2 years.

COVID activity shows signs of slowing in parts of US
Wastewater levels are at the very high level nationally, but show downward trends in the South and Midwest.
CDC pandemic review of US H5N1 virus on par with earlier assessments from same clade
Like two recent 2.3.4.4b viruses, the subtype from the Texas patient is of moderate risk for both future emergence and public health impact.

WHO declares global public health emergency for mpox surge in Africa
As plans move forward to mobilize vaccine, health officials still better epi information to best target the supplies.

Study identifies risk groups for severe COVID-19 by patient age
Children were less commonly vaccinated compared to adults.
CDC alerts providers about spike in parvovirus B19 activity
CDC said it had received multiple reports of increased activity from multiple sources, including clusters of complications in vulnerable groups.
European officials say more imported clade 1 mpox cases likely
The ECDC said the risk is high for those who have close contact with affected communities and moderate for people who are contacts of imported clade 1 cases.
Routine lab tests can't reliably distinguish long COVID from other illnesses, NIH study suggests
The authors say that clinicians should continue to focus on symptoms and symptom relief rather than rely only on lab test results.

Medicare data estimate Lyme disease rate 7 times higher than surveillance shows
Most cases occurred in the summer among men and in residents of high-incidence states.

Our underwriters
Unrestricted financial support provided by.

- Antimicrobial Resistance
- Chronic Wasting Disease
- All Topics A-Z
- Resilient Drug Supply
- Influenza Vaccines Roadmap
- CIDRAP Leadership Forum
- Roadmap Development
- Coronavirus Vaccines Roadmap
- Antimicrobial Stewardship
- Osterholm Update
- Newsletters
- About CIDRAP
- CIDRAP in the News
- Our Director
- Osterholm in the Press
- Shop Merchandise

UCL Grand Challenges
- Impacts and Outputs
- Partnerships
- Funded Projects

Advocacy Across Boundaries: Co-creating a framework to improve mental health in construction
Working across sectors to foster a community focused on connected policies and collaborative practices to improve mental health and wellbeing in the construction industry

1 March 2024
Grant: Grand Challenges Mental Health and Wellbeing Network Building Year awarded: 2023-24 Amount awarded: £2,482.00
- Dr Jean Xu, Bartlett School of Sustainable Construction
- Dr Simon Addyman, Bartlett School of Sustainable Construction
- Dr Alexandra Pitman, Division of Psychiatry
The construction industry is a major employer in the UK, supporting 2.1 million workers and contributing 6% to the GDP. Yet, it faces a significant mental health crisis, with suicide rates 3.7x the national average. Addressing this issue is crucial for sustainable development, as workers endure pressures like tight schedules and financial instability, often leading to a reluctance to discuss mental health.
In a collaboration between the Bartlett School of Sustainable Construction (BSSC) and UCL Division of Psychiatry, a half-day roundtable event was held on 2 July 2024. The event brought together 25 professionals from different sectors of construction and 11 researchers from numerous disciplines and different universities. There was a mix of research presentations, panel discussions and roundtable workshops on various topics of mental health and wellbeing in construction. The panel consisted of 6 experts:
- Ruth Pott, Head of Workplace Wellbeing, BAM UK and Ireland
- Jim Senior, CMIOSH, Health, Safety and Environmental Consultant
- Dr Susanna Bennett, Research Follow, Suicidal Behaviour Research Lab, University of Glasgow
- Professor Billy Hare, Professor of Construction Management, Glasgow Caledonian University
- Maisie Jenkins, PhD researcher at the University of Edinburgh and Research Manager at the Wellcome Trust
- Emeritus Professor Hedley Smyth, University College London
The conversation explored several questions, and further detail can be found in the event summary report:
- What are the specific challenges of managing mental health and wellbeing in the construction industry?
- What are the opportunities for addressing the mental health and wellbeing issues in construction?
- How to transcend the boundaries between professional disciplines and organisations for a more integrated approach to mental health and wellbeing in construction?
The project aimed to foster a community focused on connected policies and collaborative practices by engaging UCL researchers and industry leaders, culminating in a cross-disciplinary symposium to identify challenges and co-create solutions for systemic change.

Outputs and Impact
- Received follow-on funding of £6,357 from UCL's Innovation & Enterprise's Innovation Network funding.
- Established a network between researchers and industry experts in the topic of mental health and wellbeing in construction.
- Exchanged knowledge across organisations and disciplines about organisational support for mental health and wellbeing in construction, opportunities and challenges in the construction industry and how to transcend the boundaries between sectors, organisations and professions.
event report
- Industry attention and organisational actions to address mental health and wellbeing based on the co-created framework.
- Cross-disciplinary research collaboration based on identified future research directions in the event.
- UCL-Industry collaborations in the form of KTP, consultancy projects and other scholarships based on the established network

Related links
- More Mental Health & Wellbeing projects
- More Small Grants projects
- Grand Challenges Small Grants
- Grand Challenges funding opportunities
Racial-Ethnic Differences in Receipt of Past-Year Health Care Services Among Suicide Decedents: A Case-Control Study
Information & authors, metrics & citations, conclusions:, get full access to this article.
View all available purchase options and get full access to this article.
Supplementary Material
Information, published in.
- Self-destructive behavior
- Racial-ethnic disparities
- Mental health systems
- Electronic health record
Competing Interests
Funding information, export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View Options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Psychiatric Services
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

View options
Share article link.
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
- Systematic Review
- Open access
- Published: 20 August 2024
Examining the mental health services among people with mental disorders: a literature review
- Yunqi Gao 1 ,
- Richard Burns 1 ,
- Liana Leach 1 ,
- Miranda R. Chilver 1 &
- Peter Butterworth 2 , 3
BMC Psychiatry volume 24 , Article number: 568 ( 2024 ) Cite this article
Metrics details
Mental disorders are a significant contributor to disease burden. However, there is a large treatment gap for common mental disorders worldwide. This systematic review summarizes the factors associated with mental health service use.
PubMed, Scopus, and the Web of Science were searched for articles describing the predictors of and barriers to mental health service use among people with mental disorders from January 2012 to August 2023. The initial search yielded 3230 articles, 2366 remained after removing duplicates, and 237 studies remained after the title and abstract screening. In total, 40 studies met the inclusion and exclusion criteria.
Middle-aged participants, females, Caucasian ethnicity, and higher household income were more likely to access mental health services. The use of services was also associated with the severity of mental symptoms. The association between employment, marital status, and mental health services was inconclusive due to limited studies. High financial costs, lack of transportation, and scarcity of mental health services were structural factors found to be associated with lower rates of mental health service use. Attitudinal barriers, mental health stigma, and cultural beliefs also contributed to the lower rates of mental health service use.
This systematic review found that several socio-demographic characteristics were strongly associated with using mental health services. Policymakers and those providing mental health services can use this information to better understand and respond to inequalities in mental health service use and improve access to mental health treatment.
Peer Review reports
Introduction
Mental disorders such as depression and anxiety are prevalent, with nationally representative studies showing that one-fifth of Australians experience a mental disorder each year [ 5 ]. More recent estimates derived from a similar survey during the period of the COVID-19 pandemic were 21.5% [ 11 ]. Mental illness can reduce the quality of life, and increase the likelihood of communicable and non-communicable diseases [ 116 , 137 ], and is among the costliest burdens in developed countries [ 22 , 34 , 80 ]. The National Mental Health Commission [ 96 ] stated that the annual cost of mental ill-health in Australia was around $4000 per person or $60 billion. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 reported that mental disorders rank the seventh leading cause of disability-adjusted life years and the second leading cause of years lived with disability [ 48 ]. Helliwell et al. [ 56 ] indicated that chronic mental illness was a key determinant of unhappiness, and it triggered more pain than physical illness. Mental health issues can have a spillover effect on all areas of life, poor mental health conditions might lead to lower educational achievements and work performance, substance abuse, and violence [ 102 ]. In Australia, despite considerable additional investment in the provision of mental health services research suggests that the rate of psychological distress at the population level has been increasing [ 38 ], this has been argued to reflect that people who most need mental health treatment are not accessing services. Insufficient numbers of mental health services and mental healthcare professionals and inadequate health literacy have been reported as the pivotal determinants of poor mental health [ 18 ]. Previous studies have reported large treatment gaps in mental health services; finding only 42–44% of individuals with mental illness seek help from any medical or professional service provider [ 85 , 112 ] and this active proportion was much lower in low and middle-income countries [ 32 , 114 , 130 ].
Several studies have investigated factors associated with high and low rates of mental health service use and identified potential barriers to accessing mental health service use. Demographic, social, and structural factors have been associated with low rates of mental health service use. Structural barriers include the availability of mental health services and high treatment costs, social barriers to treatment access include stigma around mental health [ 125 ], fear of being perceived as weak or stigmatized [ 79 ], lack of awareness of mental disorders, and cultural stigma [ 17 ].
Existing studies that have systematically reviewed and evaluated the literature examining mental health service use have largely been constrained to specific population groups such as military service members [ 63 ] and immigrants [ 33 ], children and adolescents [ 35 ], young adults [ 76 ], and help-seeking among Filipinos in the Philippines [ 93 ]. These systematic reviews emphasize mental health service use by specific age groups or sub-groups, and the findings might not represent the patterns and barriers to mental health service use in the general population. One paper has reviewed mental health service use in the general adult population. Roberts et al. [ 112 ] found that need factors (e.g. health status, disability, duration of symptoms) were the strongest determinants of health service use for those with mental disorders.
The study results from Roberts et al. [ 112 ] were retrieved in 2016, and the current study seeks to build on this prior review with more recent research data by identifying publications since 2012 on mental health service use with a focus on high-income countries. This is in the context of ongoing community discussion and reform of the design and delivery of mental health services in Australia [ 140 ], and the need for current evidence to inform this discussion in Australia and other high-income countries. This systematic review aims to investigate factors associated with mental health service use among people with mental disorders and summarize the major barriers to mental health treatment. The specific objectives are (1) to identify factors associated with mental health service use among people with mental disorders in high-income countries, and (2) to identify commonly reported barriers to mental health service use.
Methodology
Selection procedures.
Our review adhered to PRISMA guidelines to present the results. We utilized PubMed, Scopus, and the Web of Science to search for articles describing the facilitators and barriers to mental health service use among people with mental illness from January 2012 up to August 2023. There were no specific factors that were of interest as part of conducting this systematic review, instead, the review had a broad focus intending to identify factors shown to be associated with mental health service use in the recent literature. The keywords used in our search of electronic databases were related to mental disorders and mental health service use. The full search terms and strategies were shown in Supplementary Table 1. We uploaded the search results to Covidence for deduplication and screening. After eliminating duplicates, the first author retrieved the title abstract and full-text articles for all eligible papers. Then each title and abstract were screened by two independent reviewers, to select those that would progress to full-text review. Subsequently, the two reviewers screened the full text of all the selected papers and conducted the data extraction for those that met the eligibility criteria. There were discrepancies in 12% of the papers reviewed, and all conflicts were resolved through discussion and agreed on by at least three authors.
Selection criteria
Inclusion and exclusion criteria.
In this systematic review, the scope was restricted to studies that draw samples from the general population, and the participants were either diagnosed with mental disorders or screened positive using a standardized scale. Case-control studies and cohort studies were considered for inclusion. The applied inclusion and exclusion criteria are listed in Table 1 .
Data extraction
After the full-text screening, details from all eligible studies were extracted by field into a data extraction table with thematic headings. The descriptive data includes the study title, author, publication year, geographic location, sample size, population details (gender, age), type of study design, mental disorder type (medical diagnosis or using scales) and quality grade (e.g. good, fair, and poor).
Quality assessment
The Newcastle Ottawa Scale [ 136 ] was used to evaluate the study quality for all eligible papers. We assessed the cross-sectional and cohort studies using separate assessment forms and graded each study as good, fair, or poor. The quality grade for each study was included in the data extraction table. The first author conducted the quality assessment using the Newcastle Ottawa Scale for cohort studies and the adapted scale for cross-sectional studies.
The search process is summarized in Fig. 1 . The initial search from PubMed, Scopus, and the Web of Science yielded 3230 articles: 2366 remained after removing duplicates; 2129 studies were considered not relevant; and 237 studies remained following title and abstract screening. In total, 40 studies met the inclusion criteria. Of these, four were cohort studies while thirty-six were cross-sectional studies. Ten studies (25.0%) were conducted in Canada, and nine (22.5%) were from the United States. Three studies used data from Germany (7.5%). Two studies each reported data from Australia, Denmark, Sweden, Singapore, or South Korea (5.0% of studies for each country). A single study was included with data from either the United Kingdom, Italy, Israel, Portugal, Switzerland, Chile, New Zealand, or reported pooled multinational data from six European countries (each country/ study representing 2.5% of the total sample of studies) (Table 2 ).
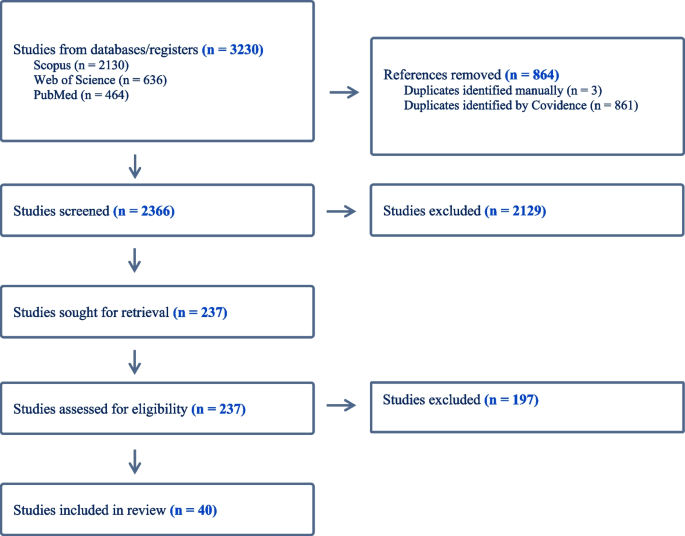
Flowchart for selections of studies
Study characteristics
As shown in Tables 2 , 3 and 4 , the sample size of studies varies; a cross-sectional study from Canada had the largest sample which contained over seven million participants [ 39 ], while the smallest sample size was 362 [ 100 ]. Sixteen studies (40.0%) used DSM-IV diagnoses [ 4 ] to measure mental disorders, twelve studies (30.0%) applied the International Classification of Disease [ 138 ], and six studies used (15.0%) the Kessler Psychological Distress Scale [ 69 ]. Only three studies (7.5%) had a hospital diagnosis of mental disorders, while three studies (7.5%) used the Patient Health Questionnaire [ 72 ] to define mental disorders.
Twenty-seven studies (67.5%) analyzed the rate of mental health service use over the last 12 months, six studies (15.0%) focused on lifetime service use, and three studies (7.5%) assessed both 12-month and lifetime mental health service use. A few studies examined other time frames, with single studies investigating mental health service use over the past 3 months, 5 years, and 7 years, and one included study considered mental health service use during the 24 months before and after a sibling’s death.
Twenty of the forty studies were classified as good quality (50.0%), seventeen as fair (42.5%), and three as poor quality (7.5%).
Overview of samples and factors investigated
The included studies examined a range of different factors associated with mental health service use. These included gender, age, marital status, ethnic groups, alcohol and drug abuse, education and income level, employment status, symptom severity, and residential location. The review identified service utilization factors related to socio-demographics, differences in utilization across countries, emerging socio-demographic factors and contexts, as well as structural and attitudinal barriers. These are described in further detail below.
Socio-demographic characteristics
Fifteen studies analyzed the association between gender and mental health service use, with fourteen studies reporting that mental health service use was more frequent among females with mental disorders than males [ 2 , 37 , 42 , 43 , 47 , 54 , 66 , 67 , 90 , 103 , 119 , 123 , 128 , 130 ]. A South Korean study concluded that gender was not associated with mental health service use [ 100 ], which might be due to the small sample size of 362 participants in the study.
Fourteen studies investigated age in association with mental health service use. Nine studies concluded that mental health service use was lower among young and old adult groups, with middle-aged persons with a mental disorder being most likely to access treatment from a mental health professional [ 26 , 42 , 43 , 47 , 54 , 66 , 67 , 123 , 130 ]. Forslund et al. [ 43 ] reported that mental health service use for women in Sweden peaked in the 45-to-64-year age group, while amongst males, mental health service use was stable across the lifespan. In contrast, two articles from New Zealand and Singapore each reported that young adults were the age group most likely to access services [ 28 , 119 ]. Reich et al. [ 103 ] concluded that age was unrelated to mental health service use when considered for the whole population, but sex-specific analyses reported that mental health service use was higher in older than younger females, while the opposite pattern was observed for males. A Canadian study using community health survey data also observed no significant age-related differences in mental health service use [ 104 ].
Marital status
There was mixed evidence concerning marital status. Studies from the United States and Germany concluded that participants who were married or cohabiting had lower rates of mental health service use [ 26 , 90 ], while Silvia et al. [ 120 ] found that mental health service use was higher among married participants in Portugal. Shafie et al. [ 119 ] reported being widowed was associated with lower rates of mental health service use in Singapore.
Ethnic groups
Eight studies examined the relationship between ethnic background and mental healthcare service use. Non-Hispanic White respondents were more likely to use mental health services in Canada and the United States [ 24 , 26 , 30 , 130 , 139 ], while Asians showed lower rates of mental health service use [ 28 , 139 ]. Chow & Mulder [ 28 ] investigated mental health service use among Asians, Europeans, Maori, and Pacific peoples in New Zealand. They concluded that Maori had the highest rate of mental health service use compared with other ethnic groups. De Luca et al. [ 30 ] reported that mental health service use was lower among ethnic minority non-veterans compared to veterans in the United States, especially for those with Black or Hispanic backgrounds. In contrast, a study conducted in the UK found that mental health service use did not vary by ethnicity, with no difference between white and non-white persons [ 54 ].
Alcohol and drug abuse
Two studies reported risky alcohol use was negatively associated with mental health service use [ 26 , 132 ]. However, within the time frame of the current review, there was insufficient published evidence on the impact of drug abuse on mental health service use among people with mental disorders. Choi, Diana & Nathan [ 26 ] found that drug abuse can lead to lower rates of mental health service use in the United States. In contrast, Werlen et al. [ 132 ] reported that risky use of (non-prescribed) prescription medications was associated with higher rates of mental health service use in Switzerland.
Education, income, and employment status
Four studies analyzed the relationship between education level, income, and mental health service use. Higher levels of educational attainment [ 26 , 120 ] and higher income [ 26 ] were generally reported to be associated with an increased likelihood of mental health service use. However, Reich et al. [ 103 ] observed that in Germany, high education and perceived middle or high social class were associated with reduced mental health service use. One paper reported no significant difference in mental health service use in South Korea, possibly due to the small number of people accessing mental healthcare services [ 100 ].
Three studies reported that compared to those who are unemployed, those in work were less likely to use mental health services [ 26 , 90 , 119 ]. This outcome aligned with a Canadian study consisting of immigrants and general populations, Islam et al. [ 66 ] concluded that immigrants who were currently unemployed had higher odds of seeking treatment than those who were employed. However, an Italian [ 123 ] and a South Korean study [ 100 ] found that employment status was not related to mental health service use.
Symptom severity
Ten studies investigated the association between symptom severity and mental health service use and ten papers concluded that participants with moderate or serious psychological symptoms were more likely to use mental health services compared to those with mild symptoms [ 23 , 27 , 66 , 103 , 120 , 123 , 130 , 139 ]. Other studies showed that study participants who viewed their mental health as poor [ 42 ], who were diagnosed with more than one mental disorder [ 103 ], and those who recognized their own need for mental health treatment [ 54 , 139 ] were more likely to receive mental health services.
Residential location
Three studies investigated the association between residential location and mental health service use. Volkert et al. [ 128 ] concluded that the rates of mental health service use in Germany were significantly lower among those living in Canterbury than those living in Hamburg. A Canadian study found individuals living in neighborhoods where renters outnumber homeowners were less likely to access mental health services [ 42 ]. In the United States, for participants with low or moderate mental illness, mental health service use was lower for those residing closer to clinics [ 46 ].
Immigrants & refugees
The reviewed research found that non-refugee immigrants had slightly higher rates of mental health service use than refugees [ 10 ]. Other research found that long-term residents were more likely to access services than immigrants regardless of their origin [ 31 , 134 ]. For example, Italian citizens were found to have higher rates of mental health service use compared to immigrants, especially for affective disorders [ 123 ]. In Canada, immigrants from West and Central Africa were more likely to access mental health services compared to immigrants from East Asia and the Pacific [ 31 ]. Research from Chile found that the rates of mental health service use were similar for immigrants and non-immigrants [ 40 ]. Although, a positive association between the severity of symptoms and rates of mental health service use was only observed among immigrants [ 40 ]. Whitley et al. [ 134 ] found that immigrants born in Asia or Africa had lower rates of mental health service use, but higher rates of service satisfaction scores compared to immigrants from other countries.
Emerging areas
Our literature review identified several areas in which only a small number of studies were found. We briefly describe them here as these may reflect emerging areas of research interest. Few published articles examined mental health treatment among participants with mental disorders together with chronic physical health conditions, and we only included the papers in this systematic review if they contained a healthy comparison group. We identified two papers that focused on survivors of adolescent and young adult cancer [ 68 ] and participants with physical health problems [ 110 ]. Both studies reported that participants with other chronic conditions reported higher rates of mental health service use than the general population [ 68 , 110 ].
Two studies compared treatment seeking among people experiencing stressful life events. Erlangsen et al. [ 39 ] investigated the impact of spousal suicide, and Gazibara et al. [ 45 ] examined the effect of a sibling’s death on mental health service use. People bereaved by relatives’ deaths were more likely to use mental health services than the general population [ 39 , 45 ]. The peak effect was observed in the first 3 months after the death for both genders, while evidence of an increase in mental health service use was evident up to 24 months before a sibling’s death and remained evident for at least 24 months after the death [ 45 ].
One paper studied the impact of the COVID-19 pandemic lockdown on mental health service use. An Israeli study concluded that compared to 2018 and 2019, adults reported they were reluctant to receive treatment during the pandemic lockdown and observed a decrease in mental health service use [ 13 ].
Structural and attitudinal barriers
In addition to the research considering a range of population characteristics (e.g. male, younger, or older age), several papers examined how attitudinal and structural factors were associated with mental health service use. The most frequently reported of these factors were cost [ 23 , 46 , 68 , 120 ], lack of transportation [ 46 , 83 ], inadequate services/ lack of availability [ 23 , 46 , 83 , 128 ], poor understanding of mental disorders and what services were available [ 10 , 11 , 22 , 83 , 100 , 105 , 120 ], language difficulties [ 10 ], and stigma-related barriers [ 83 , 100 , 103 , 105 , 128 ]. Cultural issues and personal beliefs may influence the understanding of mental disorders and prevent people from using mental health services due to mistrust or fear of treatment [ 100 , 128 ]. The review also observed some unique barriers to different population groups. Choi, Diana & Nathan [ 26 ] mentioned that lack of readiness and treatment cost were the biggest difficulties for older adults, while young participants were more concerned about stigma. Females also reported childcare as a factor limiting their ability to use mental health services, while the evidence reviewed argued that males prefer to solve mental health issues on their own, with internal control beliefs and lack of social support likely reducing their use of mental health services [ 37 , 103 ].
Summary of evidence
This systematic review investigated mental health service use among people with mental disorders and identified the factors associated with service use in high-income countries.
Most studies found that females with mental health conditions were more likely to use mental health services than males. The relationship between age and mental health service use was bell-shaped, with middle-aged participants having higher rates of mental health service use than other age groups. Possible explanations included that the elderly might be reluctant to disclose mental health symptoms, they might attribute their mental health symptoms to increasing age [ 20 ], and they may prefer to self-manage instead of seeking help from health professionals [ 44 ]. Caucasian ethnicity and higher household income were also associated with higher rates of mental health service use. Greater use of mental health services was observed in participants with severe mental symptoms, including among veterans [ 19 , 37 , 92 ]. Two studies also concluded that compared to other cultural groups, Asian respondents were more likely to receive treatment when problems were severe or had disabling effects [ 86 , 97 ]. There was mixed evidence regarding employment status, although some studies found employment to be negatively related to receiving treatment [ 26 , 90 ], and unemployed people are more likely to seek help [ 119 ]. There was inconsistent evidence for the association between marital status and service utilization. This contradictory evidence on marital status might be attributed to a lack of specification, some papers categorize it as married and non-married [ 26 , 71 , 131 ], while others further differentiate between those who were widowed, separated, and divorced [ 90 , 119 ].
A number of studies showed that immigrants can face unique stressors owing to their experience of migration, which may exacerbate or be the source of their mental health issues, and impact the use of mental health services [ 1 , 8 ]. These include separation from families, support networks, linguistic and cultural barriers [ 9 , 113 ].
Due to the increased number of international migrants, immigrants’ mental health status and healthcare use has drawn growing attention [ 7 , 77 , 99 ]. Kirmayer et al. [ 70 ] and Helman [ 57 ] found that culture might be associated with people’s attitudes and understanding of mental health, influencing help-seeking behaviors. In general, the current results showed that immigrants and refugees were less likely to use mental health services than their native-born counterparts, and this finding was consistent with previous studies [ 75 , 82 , 127 ]. For immigrants, the length of stay in the host country was closely related to rates of mental health service use, which was argued to reflect increasing familiarity with the host culture and language proficiency [ 1 , 59 ].
Both mental disorders and chronic diseases contribute significantly to the global burden of disease. Prior studies have shown that people with chronic disease have a higher chance of experiencing psychological distress [ 6 , 14 , 68 , 73 ], and vice versa [ 49 , 74 ]. Hendrie et al. [ 58 ] concluded that respondents with chronic diseases were more likely to attend mental healthcare and reported higher costs. Negative experiences and stressful consequences related to chronic disease might contribute to the increased potential for mental illness but more opportunities to seek help from health professionals [ 60 , 108 , 135 ]. People with chronic diseases and mental health problems might experience more long-term pain and limitations in their daily lives, and these stressors can exacerbate their health conditions, and impact their attitude toward seeking help.
The COVID-19 pandemic had a major impact on mental health service use worldwide, the hospital admission and consultation rate decreased dramatically during the first pandemic year [ 118 ]. This reduction in service access might be a side effect of social distancing measures taken as mitigation measures, reducing both inciting incidents and physical access to services.
Financial difficulty, service availability, and stigma were frequently identified in the literature as structural and attitudinal factors associated with lower rates of mental health service use. These factors were associated with the different rates of mental health service use for different ethnicities. For example, Asian people were less likely than other groups to identify cost as a factor limiting their use of mental health services, with a major barrier for Asian people being stigma and cultural factors [ 139 ].
Limitations
This systematic review employed a broad search strategy with broad search terms to capture relevant articles. Rather than emphasizing a particular mental disorder, this review focused on the rates of mental health service use among adults aged 18 years or older who were experiencing a common mental disorder. However, this review still contained limitations. First was the potential for selection bias. Although we used various search terms for mental health service use and mental disorder, it is possible that the service use was not the primary research question for some papers, or that the relevant service use outcome was not statistically significant- in these cases, if the information was not reported in the abstract, relevant papers might have been missed. It is also important to note that this systematic review includes studies conducted in different countries and that the mental health systems and opportunities for access vary among countries. We only searched for full-text peer-reviewed articles published in English. Grey literature and papers published in other languages were excluded from the search. Most of the included literature used self-reported data to measure service access, and these data can be liable to recall bias. Studies using administrative data were also included in the systematic review, and we note that although they have large datasets, compared to survey data, there is often a lack of adequate control variables included to minimize possible confounding influences.
Future research
There is a need for more published articles on several aspects that may influence the service utilization among people with mental disorders, including the impact of residential or neighborhood areas, and household income across various income groups. These aspects are important population characteristics that require further research to inform the targeting and type of support (e.g. low-cost, accessible). Additionally, there was a lack of longitudinal research on mental health service use, future studies could use the data to identify changes over time and relate events to specific exposures (e.g. Covid-19 pandemic). Future studies can investigate the cost of mental health treatment in detailed aspects, (e.g. publicly funded mental health services, community-based support for free or low-cost mental health services). Overall, there was a lack of studies for ethnic minorities, given ethnic minority groups were more vulnerable to mental disorders but with less mental health service use. Future research can expand gender identity representation in data collection and move beyond the binary genders. People with non-binary gender identities can face greater challenges and disadvantages in mental health and mental health service use.
This review identified that middle-aged, female gender, Caucasian ethnicity, and severity of mental disorder symptoms were factors consistently associated with higher rates of mental health service use among people with a mental disorder. In comparison, the influence of employment and marital status on mental health service use was unclear due to the limited number of published studies and/ or mixed results. Financial difficulty, stigma, lack of transportation, and inadequate mental health services were the structural barriers most consistently identified as being associated with lower rates of mental health service use. Finally, ethnicity and immigrant status were also associated with differences in understanding of mental health (i.e. mental health literacy), effectiveness of mental health treatments, as well as language difficulties. The insights gained through this review on the factors associated with mental health service use can help clinicians and policymakers to identify and provide more targeted support for those least likely to access services, and this in turn may contribute to reducing inequalities in not only mental health service use but also the burden of mental disorders.
Availability of data and materials
All data and materials related to the study are available on request from the first author, [email protected].
Abe-Kim J, Takeuchi DT, Hong S, Zane N, Sue S, Spencer MS, et al. Use of mental health–related services among immigrant and US-born Asian americans: results from the national latino and Asian American study. Am J Public Health. 2007;97(1):91–8.
Article PubMed PubMed Central Google Scholar
Abramovich A, De Oliveira C, Kiran T, Iwajomo T, Ross LE, Kurdyak P. Assessment of health conditions and health service use among transgender patients in Canada. JAMA Netw Open. 2020;3(8):e2015036. https://doi.org/10.1001/jamanetworkopen.2020.15036 .
Ambikile JS, Iseselo MK. Mental health care and delivery system at Temeke hospital in Dar Es Salaam, Tanzania. BMC Psychiatry. 2017;17:1–13. https://doi.org/10.1186/s12888-017-1271-9 .
Article Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
Book Google Scholar
Australian Bureau of Statistics. 2017-18, Mental health, ABS, viewed 23 July 2023. https://www.abs.gov.au/statistics/health/mental-health/mental-health/2017-18 .
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes. Diabetes Care. 2001;24(6):1069–78.
Article CAS PubMed Google Scholar
Bacon L, Bourne R, Oakley C, Humphreys M. Immigration policy: implications for mental health services. Adv Psychiatr Treat. 2010;16:124–32.
Bhatia S, Ram A. Theorizing identity in transnational and diaspora cultures: a critical approach to acculturation. Int J Intercultural Relations. 2009;33:140–9.
Bhugra D. Migration, distress and cultural identity. Br Med Bull. 2004;69:129–41.
Article PubMed Google Scholar
Björkenstam E, Helgesson M, Norredam M, Sijbrandij M, de Montgomery CJ, Mittendorfer-Rutz E. Differences in psychiatric care utilization between refugees, non-refugee migrants and Swedish-born youth. Psychol Med. 2022;52(7):1365–75. https://doi.org/10.1017/s0033291720003190 .
Australian Bureau of Statistics. (2020–2022). National study of mental health and wellbeing. ABS. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release .
Blais RK, Tsai J, Southwick SM, Pietrzak RH. Barriers and facilitators related to mental health care use among older veterans in the United States. Psychiatr Serv. 2015;66(5):500–6. https://doi.org/10.1176/appi.ps.201300469 .
Blasbalg U, Sinai D, Arnon S, Hermon Y, Toren P. Mental health consequences of the COVID-19 pandemic: results from a large-scale population-based study in Israel. Compr Psychiatr. 2023;123:123. https://doi.org/10.1016/j.comppsych.2023.152383 .
Bodurka-Bevers D, Basen-Engquist K, Carmack CL, Fitzgerald MA, Wolf JK, Moor Cd, Gershenson DM. Depression, anxiety, and quality of life in patients with epthelial ovarian cancer. Gynecol Oncol. 2000;78:302–8.
Bondesson E, Alpar T, Petersson IF, Schelin MEC, Jöud A. Health care utilization among individuals who die by suicide as compared to the general population: a population-based register study in Sweden. BMC Public Health. 2022;22(1):1616. https://doi.org/10.1186/s12889-022-14006-x
Borges G, Aguilar-Gaxiola S, Andrade L, Benjet C, Cia A, Kessler RC, Orozco R, Sampson N, Stagnaro JC, Torres Y, Viana MC, Medina-Mora ME. Twelve-month mental health service use in six countries of the Americas: a regional report from the World Mental Health Surveys. Epidemiol Psychiatr Sci. 2019;29:e53. https://doi.org/10.1017/s2045796019000477 .
Article CAS PubMed PubMed Central Google Scholar
Brenman NF, Luitel NP, Mall S, Jordans MJD. Demand and access to mental health services: a qualitative formative study in Nepal. BMC Int Health Hum Rights. 2014;14(1):1–12. https://doi.org/10.1186/1472-698X-14-22 . PMID: 25084826.
Budhathoki SS, Pokharel PK, Good S, Limbu S, Bhattachan M, Osborne RH. The potential of health literacy to address the health related UN sustainable development goal 3 (SDG3) in Nepal: a rapid review. BMC Health Serv Res. 2017;17(1):1–13. https://doi.org/10.1186/s12913-016-1943-z . PMID: 28049468.
Brown JS, Evans-Lacko S, Aschan L, Henderson MJ, Hatch SL, Hotopf M. Seeking informal and formal help for mental health problems in the community: a secondary analysis from a psychiatric morbidity survey in South London. BMC Psychiatry. 2014;14(1):275.
Burroughs H, Lovell K, Morley M, Baldwin R, Burns A, Chew-Graham C. Justifiable depression’: how primary care professionals and patients view late-life depression? A qualitative study. Fam Pract. 2006;23(3):369–77. https://doi.org/10.1093/fampra/cmi115 .
Caron J, Fleury MJ, Perreault M, Crocker A, Tremblay J, Tousignant M, Kestens Y, Cargo M, Daniel M. Prevalence of psychological distress and mental disorders, and use of mental health services in the epidemiological catchment area of Montreal South-West. BMC Psychiatry. 2012;12:12. https://doi.org/10.1186/1471-244X-12-183 .
Chan CMH, Ng SL, In S, Wee LH, Siau CS. Predictors of psychological distress and mental health resource utilization among employees in Malaysia. Int J Environ Res Public Health. 2021;18(1):1–15. https://doi.org/10.3390/ijerph18010314 .
Chaudhry MM, Banta JE, McCleary K, Mataya R, Banta JM. Psychological distress, structural barriers, and health services utilization among U.S. adults: National Health interview survey, 2011–2017. Int J Mental Health. 2022. https://doi.org/10.1080/00207411.2022.2123694
Chiu M, Amartey A, Wang X, Kurdyak P, Luppa M, Giersdorf J, Riedel-Heller S, Prütz F, Rommel A. Ethnic differences in mental health status and service utilization: a population-based study in Ontario, Canada frequent attenders in the German healthcare system: determinants of high utilization of primary care services. Results from the cross-sectional. Can J PsychiatryBMC Fam Pract. 2018;6321(71):481–91. https://doi.org/10.1186/s12875-020-1082-9 .
Cho SJ, Lee JY, Hong JP, Lee HB, Cho MJ, Hahm BJ. Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2009;44:943–51.
Choi NG, DiNitto DM, Marti CN. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014;145:113–20. https://doi.org/10.1016/j.drugalcdep.2014.10.004 .
Chong SA, Abdin E, Vaingankar JA, Kwok KW, Subramaniam M. Where do people with mental disorders in Singapore go to for help? Ann Acad Med Singap. 2012;41(4):154–60.
Chow CS, Mulder RT. Mental health service use by asians: a New Zealand census. N Z Med J. 2017;130(1461):35–41.
PubMed Google Scholar
Dang HM, Lam TT, Dao A, Weiss B. Mental health literacy at the public health level in low and middle income countries: an exploratory mixed methods study in Vietnam. PLoS ONE. 2020;15(12):e0244573. https://doi.org/10.1371/journal.pone.0244573
De Luca SM, Blosnich JR, Hentschel EA, King E, Amen S. Mental health care utilization: how race, ethnicity and veteran status are associated with seeking help. Community Ment Health J. 2016;52(2):174–9. https://doi.org/10.1007/s10597-015-9964-3 .
Durbin A, Moineddin R, Lin E, Steele LS, Glazier RH. Mental health service use by recent immigrants from different world regions and by non-immigrants in Ontario, Canada: a cross-sectional study. BMC Health Serv Res. 2015;15(1):336. https://doi.org/10.1186/s12913-015-0995-9
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA. 2004;291(21):2581–90.
Derr AS. Mental health service use among immigrants in the United States: a systematic review. Psychiatr Serv. 2016;67:265–74. https://doi.org/10.1176/appi.ps.201500004 .
Dimoff JK, Kelloway EK. With a little help from my Boss: the impact of workplace mental health training on leader behaviors and employee resource utilization. J Occup Health Psychol. 2019;24:4–19.
Duong MT, Bruns EJ, Lee K, et al. Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm Policy Ment Health. 2021;48:420–39. https://doi.org/10.1007/s10488-020-01080-9 .
Edman JL, Kameoka VA. Cultural differences in illness schemas: an analysis of Filipino and American illness attributions. J Cross Cult Psychol. 1997;28(3):252–65.
Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, Timko C, Beckham JC. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr Serv. 2013;64(2):134–41. https://doi.org/10.1176/appi.ps.004792011 .
Enticott J, Dawadi S, Shawyer F, Inder B, Fossey E, Teede H, Rosenberg S, Ozols Am I, Meadows G. Mental Health in Australia: psychological distress reported in six consecutive cross-sectional national surveys from 2001 to 2018. Front Psychiatry. 2022;13:815904. https://doi.org/10.3389/fpsyt.2022.815904
Erlangsen A, Runeson B, Bolton JM, Wilcox HC, Forman JL, Krogh J, Katherine Shear M, Nordentoft M, Conwell Y. Association between spousal suicide and mental, physical, and social health outcomes a longitudinal and nationwide register-based study. JAMA Psychiatry. 2017;74(5):456–64. https://doi.org/10.1001/jamapsychiatry.2017.0226 .
Errazuriz A, Schmidt K, Valenzuela P, Pino R, Jones PB. Common mental disorders in Peruvian immigrant in Chile: a comparison with the host population. BMC Public Health. 2023;23(1):1274. https://doi.org/10.1186/s12889-023-15793-7
Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, Chiu WT, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hu C, Karam EG, Kawakami N, Lee S, Lund C, Kovess-Masfety V, Levinson D, Thornicroft G. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48(9):1560–71. https://doi.org/10.1017/s0033291717003336 .
Fleury MJ, Grenier G, Bamvita JM, Perreault M, Kestens Y, Caron J. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int J Equity Health. 2012;11(1):20. https://doi.org/10.1186/1475-9276-11-20
Forslund T, Kosidou K, Wicks S, Dalman C. Trends in psychiatric diagnoses, medications and psychological therapies in a large Swedish region: a population-based study. BMC Psychiatry. 2020;20(1):328. https://doi.org/10.1186/s12888-020-02749-z
Garrido MM, Kane RL, Kaas M, Kane RA. Use of mental health care by community-dwelling older adults. J Am Geriatr Soc. 2011;59(1):50–6. https://doi.org/10.1111/j.1532-5415.2010.03220.x .
Gazibara T, Ornstein KA, Gillezeau C, Aldridge M, Groenvold M, Nordentoft M, Thygesen LC. Bereavement among adult siblings: an examination of health services utilization and mental health outcomes. Am J Epidemiol. 2021;190(12):2571–81. https://doi.org/10.1093/aje/kwab212 .
Glasheen C, Forman-Hoffman VL, Hedden S, Ridenour TA, Wang J, Porter JD. Residential transience among adults: prevalence, characteristics, and association with mental illness and mental health service use. Community Ment Health J. 2019;55(5):784–97. https://doi.org/10.1007/s10597-019-00385-w .
Gonçalves DC, Coelho CM, Byrne GJ. The use of healthcare services for mental health problems by middle-aged and older adults. Arch Gerontol Geriatr. 2014;59(2):393–7. https://doi.org/10.1016/j.archger.2014.04.013 .
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. 2022;9:137–50. https://doi.org/10.1016/S2215-0366(21)00395-3 .
Article PubMed Central Google Scholar
Goff DC, Sullivan LM, McEvoy JP, et al. A comparison of ten-year cardiac risk estimates in schizophrenia patients from the CATIE Study and matched controls. Schizophr Res. 2005;80(1):45–53. https://doi.org/10.1016/j.schres.2005.08.010 .
Goncalves Daniela C. From loving grandma to working with older adults: promoting positive attitudes towards aging. Educ Gerontol. 2009;35(3):202–25.
Gong F, Gage S-JL, Tacata LA Jr. Helpseeking behavior among Filipino americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88. https://doi.org/10.1002/jcop.10063 .
Grossbard JR, Lehavot K, Hoerster KD, Jakupcak M, Seal KH, Simpson TL. Relationships among veteran status, gender, and key health indicators in a national young adult sample. Psychiatric Serv. 2013;64(6):547–53. https://doi.org/10.1176/appi.ps.003002012 .
Hajebi A, Motevalian SA, Rahimi-Movaghar A, Sharifi V, Amin-Esmaeili M, Radgoodarzi R, Hefazi M. Major anxiety disorders in Iran: prevalence, sociodemographic correlates and service utilization. BMC Psychiatry. 2018;18(1):261. https://doi.org/10.1186/s12888-018-1828-2
Harber-Aschan L, Hotopf M, Brown JSL, Henderson M, Hatch SL. Longitudinal patterns of mental health service utilisation by those with mental-physical comorbidity in the community. J Psychosom Res. 2019;117:10–9. https://doi.org/10.1016/j.jpsychores.2018.11.005 .
Huýnh C, Caron J, Fleury MJ. Mental health services use among adults with or without mental disorders: do development stages matter? Int J Soc Psychiatry. 2016;62(5):434–51. https://doi.org/10.1177/0020764016641906 .
Helliwell JF, Layard R, Sachs JD, De Neve JE, Aknin LB, Wang S, editors. World Happiness Report 2022. New York: Sustainable Development Solutions Network; 2022.
Google Scholar
Helman C. Culture, health and illness. 5th ed. CRC Press; 2007. https://doi.org/10.1201/b13281 .
Hendrie HC, Lindgren D, Hay DP, et al. Comorbidity profile and healthcare utilization in elderly patients with serious mental illnesses. Am J Geriatr Psychiatry. 2013;21(12):1267–76. https://doi.org/10.1016/j.jagp.2013.01.056 .
Hermannsdóttir BS, Aegisdottir S. Spirituality, connectedness, and beliefs about psychological services among Filipino immigrants in Iceland. Counsel Psychol. 2016;44(4):546–72.
Hoffman KE, McCarthy EP, Recklitis CJ, Ng AK. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169:1274–81.
Hoge C, Castro C, Messer S, McGurk D, Cotting D, Koffman R. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22.
Hoge C, Grossman S, Auchterlonie J, Riviere L, Milliken C, Wilk J. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatric Serv. 2014;65(8):997–1004. https://doi.org/10.1176/appi.ps.201300307 .
Hom MA, Stanley IH, Schneider ME, Joiner TE. A systematic review of help-seeking and mental health service utilization among military service members. Clin Psychol Rev. 2017;53:59–78. https://doi.org/10.1016/j.cpr.2017.01.008 .
Hwang W, Miranda J, Chung C. Psychosis and shamanism in a Filipino–American immigrant. Cult Med Psychiatry. 2007;31(2):251–69.
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR. (Eds.). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington National Academies Press (US). 2023. https://doi.org/10.17226/12875 .
Islam F, Khanlou N, Macpherson A, Tamim H. Mental health consultation among Ontario’s immigrant populations. Community Ment Health J. 2018;54(5):579–89. https://doi.org/10.1007/s10597-017-0210-z .
Jacobi F, Groß J. Prevalence of mental disorders, health-related quality of life, and service utilization across the adult life span. Psychiatrie. 2014;11(4):227–33. https://doi.org/10.1055/s-0038-1670774 .
Kaul S, Avila JC, Mutambudzi M, Russell H, Kirchhoff AC, Schwartz CL. Mental distress and health care use among survivors of adolescent and young adult cancer: a cross-sectional analysis of the National Health Interview Survey. Cancer. 2017;123(5):869–78. https://doi.org/10.1002/cncr.30417 .
Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9.
Kirmayer LJ, Weinfeld M, Burgos G, et al. Use of health care services for psychological distress by immigrants in an urban multicultural milieu. Can J Psychiatry. 2007;52:295–304.
Kose T. Gender, income and mental health: the Turkish case. PLoS ONE. 2020;15(4):e0232344. https://doi.org/10.1371/journal.pone.0232344
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Kugaya A, Akechi T, Okuyama T, Nakano T, Mikami I, Okamura H, Uchitomi Y. Prevalence, predictive factors, and screening for psychological distress in patients with newly diagnosed head and neck cancer. Cancer. 2000;88:2817–23.
Kurdyak PA, Gnam WH, Goering P, Chong A, Alter DA. The relationship between depressive symptoms, health service consumption, and prognosis after acute myocardial infarction: a prospective cohort study. BMC Health Serv Res. 2008;8: 200. https://doi.org/10.1186/1472-6963-8-200 .
Le Meyer O, Zane N, Cho YI, Takeuchi DT. Use of specialty mental health services by Asian americans with psychiatric disorders. J Consult Clin Psychol. 2009;77(5):1000–5. https://doi.org/10.1037/a0017065 .
Li W, Dorstyn DS, Denson LA. Predictors of mental health service use by young adults: a systematic review. Psychiatric Serv. 2016;67(9):946–56. https://doi.org/10.1176/appi.ps.201500280 .
Lindert J, Schouler-Ocak M, Heinz A, Priebe S. Mental health, health care utilisation of migrants in Europe. Eur Psychiatry. 2008;23 Suppl 1:14–20.
CAS PubMed Google Scholar
Lovering S. Cultural attitudes and beliefs about pain. J Transcult Nurs. 2006;17(4):389–95.
Luitel NP, Jordans MJD, Kohrt BA, Rathod SD, Komproe IH. Treatment gap and barriers for mental health care: A cross-sectional community survey in Nepal. PLoS One. 2017;12(8):1–15. https://doi.org/10.1371/journal.pone.0183223 . PMID: 28817734.
Article CAS Google Scholar
Jansson I, Gunnarsson AB. Employers’ views of the impact of Mental Health problems on the ability to work. Work. 2018;59:585–98.
Kayiteshonga Y, Sezibera V, Mugabo L, Iyamuremye JD. Prevalence of mental disorders, associated co-morbidities, health care knowledge and service utilization in Rwanda - towards a blueprint for promoting mental health care services in low- and middle-income countries? BMC Public Health. 2022;22(1):1858. https://doi.org/10.1186/s12889-022-14165-x .
Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, Hassan G, Rousseau C, Pottie K, Canadian Collaboration for Immigrant and Refugee Health (CCIRH). Common mental health problems in immigrants and refugees: general approach in primary care. Can Med Assoc J. 2011;183(12):E959-67. https://doi.org/10.1503/cmaj.090292 .
Kline AC, Panza KE, Nichter B, Tsai J, Harpaz-Rotem I, Norman SB, Pietrzak RH. Mental health care use among U.S. Military veterans: results from the 2019–2020 national health and resilience in veterans study. Psychiatr Serv. 2022;73(6):628–35. https://doi.org/10.1176/appi.ps.202100112 .
Knipscheer JW, Kleber RJ. Help-seeking behavior of west African migrants. J Community Psychol. 2008;36:915–28. https://doi.org/10.1002/jcop.20264 .
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
PubMed PubMed Central Google Scholar
Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese americans. J Community Psychol. 2004;32(1):27–43.
Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. College students: 10-year population-level trends (2007–2017). Psychiatr Serv. 2019;70(1):60–3. https://doi.org/10.1176/appi.ps.201800332 .
Liu L, Chen XL, Ni CP, Yang P, Huang YQ, Liu ZR, Wang B, Yan YP. Survey on the use of mental health services and help-seeking behaviors in a community population in Northwestern China. Psychiatry Res. 2018;262:135–40. https://doi.org/10.1016/j.psychres.2018.02.010 .
Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, Yin H, Ma Y, Wang L, Huang Z, Yan Y, Wang B, Xiao S, Zhou L, Li L, Zhang Y, Chen H, Zhang T, Yan J, Zhang N. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2021;8(11):981–90. https://doi.org/10.1016/S2215-0366(21)00251-0 .
Mack S, Jacobi F, Gerschler A, Strehle J, Höfler M, Busch MA, Maske UE, Hapke U, Seiffert I, Gaebel W, Zielasek J, Maier W, Wittchen HU. Self-reported utilization of mental health services in the adult German population–evidence for unmet needs? Results of the DEGS1-Mental Health Module (DEGS1-MH). Int J Methods Psychiatr Res. 2014;23(3):289–303. https://doi.org/10.1002/mpr.1438 .
Mahar AL, Aiken AB, Cramm H, Whitehead M, Groome P, Kurdyak P. Mental health services use trends in Canadian veterans: a Population-based Retrospective Cohort Study in Ontario. Can J Psychiatry. 2018;63(6):378–86. https://doi.org/10.1177/0706743717730826 .
Maneze D, DiGiacomo M, Salamonson Y, Descallar J, Davidson PM. Facilitators and barriers to health-seeking behaviours among Filipino migrants: inductive analysis to inform health promotion. BioMed Res Int. 2015;2015:506269.
Martinez AB, Co M, Lau J, et al. Filipino help-seeking for mental health problems and associated barriers and facilitators: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2020;55:1397–413. https://doi.org/10.1007/s00127-020-01937-2 .
McKibben JBA, Fullerton CS, Gray CL, Kessler RC, Stein MB, Ursano RJ. Mental health service utilization in the U.S. Army Psychiatr Serv. 2013;64(4):347–53. https://doi.org/10.1176/appi.ps.000602012 .
Mosier KE, Vasiliadis H-M, Lepnurm M, Puchala C, Pekrul C, Tempier R. Prevalence of mental disorders and service utilization in seniors: results from the Canadian community health survey cycle 1.2. Int J Geriatr Psychiatry. 2010;25(10):960–7. https://doi.org/10.1002/gps.2434 .
National Mental Health Commission. Economics of Mental Health in Australia. 2016. Available at: https://www.mentalhealthcommission.gov.au/news-and-media/media-releases/2016/december/economics-of-mental-health-in-australia . Accessed: 20 July 2023.
Nicdao EG, Duldulao AA, Takeuchi DT. Psychological Distress, Nativity, and Help-Seeking among Filipino Americans. Education, Social Factors, and Health Beliefs in Health and Health Care Services. Emerald Group Publishing Ltd. 2015:107–20. https://doi.org/10.1108/S0275-495920150000033005 .
Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, et al. Prevalence and correlates of suicidal behavior among soldiers: results from the Army study to assess risk and resilience in service members (Army STARRS). JAMA Psychiatry. 2014;71(5):514–22. https://doi.org/10.1001/jamapsychiatry.2014 .
Ortega AN, Fang H, Perez VH, Rizzo JA, Carter-Pokras O, Wallace SP, et al. Health care access, use of services, and experiences among undocumented mexicans and other latinos. Arch Intern Med. 2007;167(21):2354–60.
Park S, Cho MJ, Bae JN, Chang SM, Jeon HJ, Hahm BJ, Son JW, Kim SG, Bae A, Hong JP. Comparison of treated and untreated major depressive disorder in a nationwide sample of Korean adults. Community Ment Health J. 2012;48(3):363–71. https://doi.org/10.1007/s10597-011-9434-5 .
Patel V, Saxena S, Lund C, et al. The lancet commission on global mental health and sustainable development. Lancet. 2018;392:1553–98.
Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–13. https://doi.org/10.1016/S0140-6736(07)60368-7 .
Reich H, Niermann HCM, Voss C, Venz J, Pieper L, Beesdo-Baum K. Sociodemographic, psychological, and clinical characteristics associated with health service (non-)use for mental disorders in adolescents and young adults from the general population. Eur Child Adolesc Psychiatry. 2023. https://doi.org/10.1007/s00787-023-02146-3 .
Pelletier L, O’Donnell S, McRae L, Grenier J. The burden of generalized anxiety disorder in Canada. Health Promot Chronic Dis Prev Can. 2017;37(2):54–62. https://doi.org/10.24095/hpcdp.37.2.04 .
Rim SJ, Hahm BJ, Seong SJ, Park JE, Chang SM, Kim BS, An H, Jeon HJ, Hong JP, Park S. Prevalence of Mental disorders and Associated factors in Korean adults: national mental health survey of Korea 2021. Psychiatry Invest. 2023;20(3):262–72. https://doi.org/10.30773/pi.2022.0307 .
Pols H, Oak S. War & military mental health: the US psychiatric response in the 20th century. Am J Public Health. 2007;97:2132–42.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet. 2007;370(9590):859–77. https://doi.org/10.1016/S0140-6736(07)61238-0 .
Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 2013;32:1143–52.
Raphael MJ, Gupta S, Wei X, Peng Y, Soares CN, Bedard PL, Siemens DR, Robinson AG, Booth CM. Long-term mental health service utilization among survivors of testicular cancer: a population-based cohort study. J Clin Oncol. 2021;39(7):779–86. https://doi.org/10.1200/jco.20.02298 .
Reaume SV, Luther AWM, Ferro MA. Physical morbidity and mental health care among young people. J Adolesc Health. 2021;68(3):540–7. https://doi.org/10.1016/j.jadohealth.2020.06.040 .
Reavley NJ, Morgan AJ, Petrie D, Jorm AF. Does mental health-related discrimination predict health service use 2 years later? Findings from an Australian national survey. Soc Psychiatry Psychiatr Epidemiol. 2020;55(2):197–204. https://doi.org/10.1007/s00127-019-01762-2 .
Roberts T, Miguel Esponda G, Krupchanka D, Shidhaye R, Patel V, Rathod S. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry. 2018;18(1):262. https://doi.org/10.1186/s12888-018-1837-1 .
Rogler LH. International migrations. A framework for directing research. Am Psychol. 1994;49(8):701–8.
Sagar R, Pattanayak RD, Chandrasekaran R, Chaudhury PK, Deswal BS, Singh RL, et al. Twelve-month prevalence and treatment gap for common mental disorders: findings from a large-scale epidemiological survey in India. Indian J Psychiatry. 2017;59(1):46.
Saxena S, Sharan P, Saraceno B. Budget and financing of mental health services: baseline information on 89 countries from WHO’s project atlas. J Ment Health Policy Econ. 2003;6(3):135–43.
Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P. Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry. 2002;41(5):530–7. https://doi.org/10.1097/00004583-200205000-00010 .
Seal KH, Metzler TJ, Gima KS, Bertenthal D, Gaguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using department of veterans affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–8.
Sepúlveda-Loyola W, Rodríguez-S´anchez I, P´erez-Rodríguez P, Ganz F, Torralba R, Oliveira DV, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020;24(9):938–47.
Shafie S, Subramaniam M, Abdin E, Vaingankar JA, Sambasivam R, Zhang Y, Shahwan S, Chang S, Jeyagurunathan A, Chong SA. Help-seeking patterns among the general population in singapore: results from the Singapore mental health study 2016. Adm Policy Ment Health Ment Health Serv Res. 2021;48(4):586–96. https://doi.org/10.1007/s10488-020-01092-5 .
Silva M, Antunes A, Azeredo-Lopes S, Cardoso G, Xavier M, Saraceno B, Caldas-de-Almeida JM. Barriers to mental health services utilisation in Portugal–results from the National mental health survey. J Mental Health. 2022;31(4):453–61. https://doi.org/10.1080/09638237.2020.1739249 .
Stecker T, Fortney J, Hamilton F, Ajzen I. An assessment of beliefs about mental health care among veterans who served in Iraq. Psychiatric Serv. 2007;58:1358–61.
Sodhi-Berry N, Preen DB, Alan J, Knuiman M, Morgan VA, Corrao G, Monzio Compagnoni M, Valsassina V, Lora A. Pre-sentence mental health service use by adult offenders in Western Australia: baseline results from a longitudinal whole-population cohort studyAssessing the physical healthcare gap among patients with severe mental illness: large real-world investigati. Crim Behav Ment HealthBJPsych Open. 2014;247(35):204–21. https://doi.org/10.1192/bjo.2021.998 .
Spinogatti F, Civenti G, Conti V, Lora A, Bahji A. Ethnic differences in the utilization of mental health services in Lombardy (Italy): an epidemiological analysisIncidence and correlates of opioid-related psychiatric emergency care: a retrospective, multiyear cohort study. Soc Psychiatry Psychiatr Epidemiol J Opioid Manage. 2015;5016(13):59223–65226. https://doi.org/10.5055/jom.2020.0572 .
The World Bank. Population, total, population, total - low income, middle income, high income. Washington, D.C.: The World Bank (producer and distributor); 2022. https://data.worldbank.org/indicator/SP.POP.TOTL?end=2022&locations=XM-XP-XD&start=1960&view=chart
Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiol Psychiatric Sci. 2008;17(1):14–9. https://doi.org/10.1017/S1121189X00002621 .
Thornicroft G, Tansella M. Components of a modern mental health service: a pragmatic balance of community and hospital care: overview of systematic evidence. Br J Psychiatry. 2004;185:283–90.
Tiwari SK, Wang J. Ethnic differences in mental health service use among White, Chinese, south Asian and South East Asian populations living in Canada. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):866–71. https://doi.org/10.1007/s00127-008-0373-6 .
Volkert J, Andreas S, Härter M, Dehoust MC, Sehner S, Suling A, Ausín B, Canuto A, Crawford MJ, Ronch D, Grassi C, Hershkovitz L, Muñoz Y, Quirk M, Rotenstein A, Santos-Olmo O, Shalev AB, Strehle AY, Weber J, Schulz K. Predisposing, enabling, and need factors of service utilization in the elderly with mental health problems. Int Psychogeriatr. 2018;30(7):1027–37. https://doi.org/10.1017/S1041610217002526 .
Wang N, Xie X. Associations of health insurance coverage, mental health problems, and drug use with mental health service use in US adults: an analysis of 2013 National Survey on Drug Use and Health. Aging Ment Health. 2019;23(4):439–46. https://doi.org/10.1080/13607863.2018.1441262 .
Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–50.
Wei Z, Hu C, Wei X, Yang H, Shu M, Liu T. Service utilization for mental problems in a metropolitan migrant population in China. Psychiatr Serv. 2013;64(7):645–52. https://doi.org/10.1176/appi.ps.201200304 .
Werlen L, Puhan MA, Landolt MA, Mohler-Kuo M. Mind the treatment gap: the prevalence of common mental disorder symptoms, risky substance use and service utilization among young Swiss adults. BMC Public Health. 2020;20(1):1470. https://doi.org/10.1186/s12889-020-09577-6 .
Wettstein A, Tlali M, Joska JA, Cornell M, Skrivankova VW, Seedat S, Mouton JP, van den Heuvel LL, Maxwell N, Davies MA, Maartens G, Egger M, Haas AD. The effect of the COVID-19 lockdown on mental health care use in South Africa: an interrupted time-series analysis. Epidemiol Psychiatr Sci. 2022;31:e43. https://doi.org/10.1017/s2045796022000270 .
Whitley R, Wang J, Fleury MJ, Liu A, Caron J. Mental health status, health care utilisation, and service satisfaction among immigrants in montreal: an epidemiological comparison. Can J Psychiatry. 2017;62(8):570–9. https://doi.org/10.1177/0706743716677724 .
Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social well-being among adolescents and young adults with cancer: a systematic review. Cancer. 2016;122:1029–37.
Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Canada. Canada: University of Ottawa; 2000. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.Asp
Westerhof GJ, Keyes CL. Mental illness and mental health: the two continua model across the lifespan. J Adult Dev. 2010;17(2):110–9. https://doi.org/10.1007/s10804-009-9082-y .
World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
Yang KG, Rodgers CRR, Lee E, B LC. Disparities in mental health care utilization and perceived need among Asian americans: 2012–2016. Psychiatr Serv. 2020;71(1):21–7. https://doi.org/10.1176/appi.ps.201900126 .
Rosenberg S, Hickie AMI. Making better choices about mental health investment: the case for urgent reform of Australia’s better access program. Australian New Z J Psychiatry. 2019;53(11):1052–8. https://doi.org/10.1177/0004867419865335 .
World Bank. World Bank income groups [dataset]. World Bank, Income Classifications [original data]. 2023. Retrieved May 2, 2024 from https://ourworldindata.org/grapher/world-bank-income-groups .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
The National Centre for Epidemiology and Population Health, Australian National University, Canberra, Australia
Yunqi Gao, Richard Burns, Liana Leach & Miranda R. Chilver
School of Psychology, Deakin University, Melbourne, Australia
Peter Butterworth
Department of Health, Economics, Wellbeing and Society, Australian National University, Canberra, Australia
You can also search for this author in PubMed Google Scholar
Contributions
YG was responsible for the study design, title and abstract screening, full-text screening, and writing the manuscript. PB, RB, and LL contributed to the study design, title and abstract screening, full-text screening, and offered comments and detailed feedback on the draft paper. MC also helped with the title and abstract screening, full-text screening, and provided comments and detailed feedback on the draft paper.
Corresponding author
Correspondence to Yunqi Gao .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gao, Y., Burns, R., Leach, L. et al. Examining the mental health services among people with mental disorders: a literature review. BMC Psychiatry 24 , 568 (2024). https://doi.org/10.1186/s12888-024-05965-z
Download citation
Received : 18 February 2024
Accepted : 15 July 2024
Published : 20 August 2024
DOI : https://doi.org/10.1186/s12888-024-05965-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health services
- Service use
- Mental disorder
- Systematic review
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Youth mental health is a 'global crisis' according to world-leading study
Topic: Mental Health
New analysis has found teen mental health is worsening. ( ABC News: Alexi Belacqua )
A global consortium of world-leading mental health experts and young people have come together to deliver 'a definitive analysis of the worldwide state of youth mental health'.
Published in the scientific journal The Lancet Psychiatry, experts say there are big implications for the health, wellbeing and productivity of young people.
What's next?
Experts and young people are calling for urgent action and better resourcing for youth mental health.
A world-first review into youth mental health describes a lack of action as a "scandal" that is having big implications for the health, wellbeing and productivity of young people.
The Lancet Psychiatry Commission on youth mental health report, published today, is the culmination of four years' work by more than 50 leading psychiatrists, psychologists, academics and young people who have experienced mental illness throughout the world.
Lead author Professor Patrick McGorry said it was clear governments were "failing young people".
"Over the last 15 to 20 years, we've seen an alarming rise, a 50 per cent increase in the need for care in this age group [in Australia]," Professor McGorry said.
Professor Patrick McGorry said not addressing teen mental health issues would have wider impacts on society. ( Supplied )
Led by Orygen, Australia's Centre of Excellence in Youth Mental Health, the report has called for existing evidence-based solutions to be scaled up, stating that "even when these illnesses do not cause death, they are the largest and most rapidly growing cause of disability and lost human potential and productivity across the life span".
"Young people have been termed as the snowflake generation, lacking in resilience," Professor McGorry said.
"It's not just that we neglect them.
"We actually blame them for the problems that they're suffering from."
Urgent call to transform care
For Finlaey Hewlett, the report was a bittersweet acknowledgement of their own difficulties in accessing support for mental health issues that began when they were just eight years old.
Finlaey Hewlett, 23, said the report was a bittersweet acknowledgement of their experiences with the health system. ( ABC News: Kenith Png )
"I grew up in regional, Western Australia and so the there was a real distinct lack of support and resources out there, especially for young people," they said.
"I couldn't even leave my house."
"I remember how lonely I felt, and how inadequate I felt."
The 23-year-old, who is on the Orygen youth advisory council, said they were let down by the system when they experienced their worst psychological distress at age 16 and in desperation went to a hospital emergency department.
"I was experiencing suicidal ideation and this sense of overwhelming hopelessness," they said.
After a 12 hour wait, they were turned away.
"Not because I wasn't suffering … but simply because I hadn't actively made an attempt on my life," they said.
"They had to save the very, very limited beds that they did have for people who were experiencing that."
Professor McGorry said too many patients were having similar experiences, falling through the cracks of the primary health care system funded by the federal government, which includes Headspace and GPs, and the hospital-based system funded by state governments.
The report found existing paediatric/adult healthcare models which disrupt care at 18 were not working and recommended a model that offered multi-disciplinary wrap around care for 12 to 25-year-olds as the way of the future.
Patrick McGorry said it was an approach pioneered by Headspace in Australia, now being replicated by other countries, but needed to be further built upon to treat more complex forms of mental illness to better support the "missing middle".
He said 39 per cent of young Australians had a diagnosable and treatable condition.
"They're treatable but mostly not treated," he said.
But he said only 50 per cent of people with mental illness got access to care.
Mental health issues account for 45 per cent of the disease burden for 10 to 24-year-olds worldwide, but only 2 per cent of health budgets globally are devoted to mental health care.
Professor McGorry said while those figures were a little better in Australia, there was still a "huge mismatch" in the government spend compared to the scale of the crisis.
Global megatrends driving mental health issues
The report named several global megatrends driving psychological distress in young people including growing intergenerational inequality, financial pressure, global instability and the rise of social media.
Finlaey Hewlett said the impact on young people was profound.
Finlaey Hewlett is a part of the Orygen Youth Advisory Council. ( ABC News: Kenith Png )
"I think the reason why this crisis is getting worse and worse is to do with the world that we are set to inherit," they said.
"We're terrified of the climate, of the loneliness that we're experiencing, the cost of living, conflict throughout the world.
"It's so much more expensive to just be a human nowadays that your mental health often does go by the wayside when you're just trying to survive."
While the commission noted the harm of social media, it was just one factor in a range of things impacting young people.
"I'm not saying that social media is not harmful. But if it's seen as the total explanation, it's a very sort of soft target," Professor McGorry said.
"It does distract away from the much more challenging megatrends that are much more difficult for politicians to deal with."
He questioned whether calls to ban social media for those under 16 was the right target.
"Do we deal with that by restricting and reducing the agency of young people, or do we actually deal with the problem at its source?" Professor McGorry said.
He said politicians should be doing more to tackle the tech titans who were "unrestrained" and had created unsafe environments for young people.
Patrick McGorry warned a lack of action would have serious consequences for society.
"The world really has to get real here if we want to see the next generation flourish, if we want to make sure our societies are cohesive and productive, this is a no-brainer," he said.
"And if we invest in this way, we will actually get a return on investment."
Government ready to review models of care
Federal Health Minister Mark Butler agreed the health system was overwhelmed.
"I wouldn't describe it as broken, but I would describe it as pretty overwhelmed," Mr Butler said.
He said the older models of care had not kept pace with the sharp increase in mental distress and a review was about to get underway.
He said youth mental health was also on the agenda at this weeks' health ministers and mental health minister's meeting.
Shadow Minister for Health Anne Ruston said now was the time for reform and investment and said the first thing a Coalition government would do if elected would be restore the Medicare-funded psychology sessions to 20 after the Labor government cut them in half.
Opposition Health spokesperson Anne Ruston said workforce shortages were also having a big impact. ( ABC News: Nick Haggarty )
Ms Ruston said the nationwide shortage of both psychologists and psychiatrists was also a major challenge.
"We need to concentrate on having a national workforce strategy so that we've got a pipeline of psychologists and psychiatrists, particularly into the future so that we can make sure that we have got the support ready," Ms Ruston said.
TechRepublic
Account information.

Share with Your Friends
Mental Health in the Workplace: 55% of CEOs and 65% of Gen Z Report Mental Health Issues
Your email has been sent
Businessolver’s 2024 State of Workplace Empathy Study , which surveyed more than 3,000 CEOs, HR professionals, and employees, paints a concerning picture: mental health is declining sharply among some employee segments.
Overall, 55% of CEOs and 50% of employees cited a mental health issue in the past year, with Gen Z (65%), women (60%), LGBTQ+ (66%), caregivers (71%), veterans (73%), and disabled or neurodivergent (77%) employees especially prone to mental health issues. Notably, CEOs’ self-reported mental health issues jumped 24 points over 2023, shattering myths of invulnerable corporate leaders.

This year’s survey revealed additional surprises. For one, more CEOs than employees view their company’s culture as toxic, to the tune of 52% and 35%, respectively. Sixty-five percent of CEOs also report feeling intimidated by coworkers, up 17 points over 2023. The study also found a strong link between mental health issues and workplace toxicity: respondents who stated their workplace is toxic were 47% more likely to cite mental health issues.
There are many factors beyond the reach of HR teams that contribute to mental health, but a toxic work environment prevents any efforts they may take toward building a culture of empathy from flourishing. The good news is, toxicity can be mitigated with some practical—and empathetic—HR strategies to promote a healthy and supportive workplace culture.
The antidote to toxicity: empathy
Toxic workplaces can take many forms, but ultimately, there is a near-universal remedy—empathy. At its core, empathy is about understanding and sharing the feelings of others, and Businessolver’s research shows it has a powerful effect on how employees at all levels experience their jobs.
In 2023, 80% of respondents said they would be willing to leave their jobs to find more empathetic employers. Just a year later, in 2024, an even higher percentage (88%) said they would be willing to stay with an employer that empathized with their needs.
The importance of empathy extends beyond fostering a positive work atmosphere. Empathetic workplaces benefit from:
- Increased employee retention.
- Higher productivity.
- Improved overall well-being.
When leaders and colleagues demonstrate empathy, it fosters a sense of trust and psychological safety. Team members and leaders alike feel comfortable expressing concerns, seeking help, and admitting mistakes.
Open communication allows for early intervention when stress or mental health issues arise, preventing problems from escalating and fostering a more supportive and collaborative work environment. In fact, there’s near 90% agreement across employees, HR professionals, and CEOs that it’s important for senior leadership to openly discuss mental health issues to foster a safe environment that encourages others to do the same.
How to build a more empathetic workplace
The data paints a clear picture: empathy in the workplace needs a significant boost. This work begins with the foundational goal of fostering an organizational culture of open communication and understanding, particularly in light of the state of mental health in the workplace.
From the strong groundwork of empathy, there are actionable steps HR teams can take to build a work environment where everyone feels empowered to care for their mental health.
Destigmatize mental health
Particularly in the workplace, mental health issues remain shrouded in stigma. This is especially pronounced among CEOs, 81% of whom said companies view someone with mental health issues as weak or a burden.
Opening a dialogue about mental health can be incredibly beneficial, particularly when the message flows down from the top. Leaders can champion these discussions by sharing their own personal experiences or participating in employer-sponsored educational sessions.
“Leadership plays a vital role in breaking down the stigma of mental illness that our data shows still thrives among American workers,” said Rae Shanahan, Chief Strategy Officer at Businessolver. “I’ve been open about my lifelong mental health journey within the walls of Businessolver and publicly. Mental health does not discriminate—it is widespread and underreported.”
SEE: Psychological Insight Could Help Australian IT Pros Grow Technical Skills Into Organisational Influence
Offer the benefits employees want
The top benefits and resources employees say help them care for their mental health include:
- Open door policies (91%).
- Mental health benefits offered at enrollment (90%).
- Employee assistance programs (89%).
- Flexible working hours (89%).
- Access to online mental health resources or clinics (89%).
- Encouragement to take breaks away from work (88%).
Improve easy access to benefits information
An overwhelming number of employees (90%) said mental health benefits offered during annual enrollment are important. Yet, just 35% reported being aware that such benefits were offered to them. Even more pertinent, only 10% reported using a mental health benefit.
Why is there such a disconnect? After enrollment, it can be difficult for employees to remember exactly what’s included in their benefits plans, and the thought of combing through plan documents to find answers is overwhelming in some cases. This is where powerful but user-friendly tools, like virtual benefits assistants, can be game-changing.
For example, Sofia, Businessolver’s AI-powered benefits assistant, is available 24/7 to respond to employee questions with human-like empathy. Not only does this tool provide access to the information employees need at the precise moment they need it, thereby making it easier for them to actually use their benefits, but it also reduces the administrative burden that often falls on the HR staff’s shoulders.
Visit Businessolver
Train managers to be empathetic leaders
Equip managers with the skills to recognize signs of stress and burnout in their teams and encourage open communication and support. Couple this with an intentional employee wellness program—which can begin simply with lunch-and-learn sessions or an employee wellness committee—and the positive power of empathy will soon ripple throughout the entire organization.
The reported decline in workplace mental health is concerning, as untreated mental health can have a significant impact not just on the morale and performance of an organization, but also on the well-being of families and communities. For these reasons, the challenge is a critical one, but not insurmountable. In fact, small gestures of empathy can be very powerful. By prioritizing them now, organizations can create a thriving and resilient workforce for the future.
Marcy Klipfel is the chief engagement officer at Businessolver. See the results of its 2024 State of Workplace Empathy survey at businessolver.com .
- Mental Health Policy
- 19 Employee Burnout Statistics in 2024
- 7 Warning Signs of an Unhappy Employee
Create a TechRepublic Account
Get the web's best business technology news, tutorials, reviews, trends, and analysis—in your inbox. Let's start with the basics.
* - indicates required fields
Sign in to TechRepublic
Lost your password? Request a new password
Reset Password
Please enter your email adress. You will receive an email message with instructions on how to reset your password.
Check your email for a password reset link. If you didn't receive an email don't forgot to check your spam folder, otherwise contact support .
Welcome. Tell us a little bit about you.
This will help us provide you with customized content.
Want to receive more TechRepublic news?
You're all set.
Thanks for signing up! Keep an eye out for a confirmation email from our team. To ensure any newsletters you subscribed to hit your inbox, make sure to add [email protected] to your contacts list.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 19 August 2024
PlayStation is good for you: video games improved mental health during COVID
- Gemma Conroy
You can also search for this author in PubMed Google Scholar

Video games boosted people’s well-being and reduced distress. Credit: Yong Teck Lim/Getty
Playing video games for a couple of hours a day can improve mental health, according to a study on gamers in Japan during the COVID-19 pandemic 1 .
The research — which was done from December 2020 to March 2022 — found that even just owning a game console increased life satisfaction and reduced psychological distress. The results were published today in Nature Human Behaviour .
The findings are a first step towards demonstrating a causal link between gaming and mental-health benefits, says Andrew Przybylski, a psychologist who studies how video games influence players’ mental health at the University of Oxford, UK. “The study provides a worked example that games researchers all around the world should follow closely,” he says. But he adds that conducting the experiment during the pandemic could have amplified the mental-health benefits of gaming because people’s mental health was generally poorer at that time and there were fewer opportunities to engage in other activities. The effect on well-being will need to be tested outside that situation, he says.
‘Publish or Perish’ is now a card game — not just an academic’s life
Although studies have explored the effects of gaming on addiction, well-being, cognitive function and aggression, the results have been mixed 2 , 3 . Most of this research has relied on observational data, which cannot be used to tease apart cause and effect, says study co-author Hiroyuki Egami, a behavioural scientist at Nihon University in Tokyo. Many video-gaming studies are also done in controlled laboratory settings, making it difficult to assess the mental-health effects of gaming in daily life, adds Egami.
Gamers unite
Some three billion people play video games globally and, during the pandemic, that number surged. In Japan, this spike in demand led to a shortage of Nintendo Switch and PlayStation 5 (PS5) consoles. To handle this, retailers set up a lottery system that randomly selected consumers who could purchase a console when it became available. Egami and his colleagues saw an opportunity to conduct a natural experiment on gaming and mental health.

Gaming helped my lab-mates and me to conquer the social-distancing blues
The study focused on 8,192 people, aged between 10 and 69, who had entered the lottery. The team collected information about their mental health, video-game ownership and sociodemographic characteristics. The researchers sent five rounds of surveys to the participants, which included two checklists that measured psychological distress and life satisfaction. Participants were also asked whether they had played video games over the past 30 days and, if so, for how long.
Participants who got the opportunity to buy a Switch or PS5 console experienced a decline in their psychological distress and had a greater life satisfaction than respondents who missed out in the lottery. The mental-health benefits of owning a PS5 were more pronounced among men, hardcore gamers and households without children.
On the other hand, owning a Switch seemed to offer a greater well-being boost to family households and less-experienced gamers. This could be because the Switch is a portable console that can be played with family and friends, whereas the PS5 can only be played by connecting it to a television and is typically used by single players, says Egami.
Life satisfaction
Playing video games on either console increased life satisfaction among the lottery participants, and doing so for an extra hour a day led to a further improvement in mental health. However, these positive effects tapered off among players who spent more than three hours a day gaming, suggesting that a long playtime doesn’t lead to further improvements in mental health.
“These results are not surprising,” says Daniel Johnson, a psychologist who specializes in video games at the Queensland University of Technology in Brisbane, Australia. “They fit with what we know from talking to video-game players for decades.”
Przybylski adds that a limitation of the study is that it didn’t investigate other factors that could affect gamers’ mental health, such as how they approach playing and their games of choice.
Egami says the next step is to replicate the study to see whether the findings hold up outside a pandemic. “The result might be different,” he says.
doi: https://doi.org/10.1038/d41586-024-02643-8
Egami, H., Rahman, M. S., Yamamoto, T., Egami, C. & Wakabayashi, T. Nature Hum. Behav . https://doi.org/10.1038/s41562-024-01948-y (2024).
Article Google Scholar
Orben, A. & Przybylski, A. K. Nature Hum. Behav. 3 , 173–182 (2019).
Article PubMed Google Scholar
Hazel, J., Kim, H. M. & Every-Palmer, S. Australas. Psychiatry 30 , 541–546 (2022).
Download references
Reprints and permissions
Related Articles

‘There’s a lot of privilege masquerading as merit’: why inclusion matters in academia
Career Q&A 19 AUG 24

Gender bias might be working at level of whole disciplines
Nature Index 19 AUG 24

Can floating homes make coastal communities resilient to climate risks?
Comment 19 AUG 24

Cash for catching scientific errors
Technology Feature 19 AUG 24

How pregnancy transforms the brain to prepare it for parenthood
News Feature 31 JUL 24
To explain biological sex, look to evolution
Correspondence 09 JUL 24

A publishing platform that places code front and centre
Technology Feature 07 AUG 24
China’s robotaxis need regulation
Correspondence 06 AUG 24
Faculty Positions in the Center for Nonhuman Primate Research in the School of Life Sciences
SLS invites applications for multiple tenure-track/tenured faculty positions at all academic ranks.
Hangzhou, Zhejiang, China
School of Life Sciences, Westlake University
Faculty Position, Center of Excellence in Neuro-Oncology Sciences (CENOS)
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Postdoctoral Fellow Position
Birmingham, Alabama (US)
University of Alabama at Birmingham (UAB)
Postdoctoral Scholar - Pharmaceutical Sciences
The University of Tennessee Health Science Center (UTHSC)
Postdoctoral Scholar- Speech Language Pathologist
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Pryjmachuk S, Elvey R, Kirk S, et al. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Southampton (UK): NIHR Journals Library; 2014 Jun. (Health Services and Delivery Research, No. 2.18.)

Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study.
Chapter 5 the case study.
This chapter focuses on Stage 2, the empirical – or ‘primary research’ – aspect of the study, which we conducted using the case study method. We start with an outline of the specific research methods used, after which we provide a descriptive overview of the individual case study sites; we then present our findings, organised according to a number of analytical themes.
This stage of the project was designed to inform research objectives 3 and 4, which were concerned with, respectively, the factors influencing the acceptability of mental health self-care support services for CYP and the barriers affecting the implementation of such services. In addition, as with the mapping exercise (see Chapter 4 ), this stage of the study also helps realise objective 5, which was concerned with the interface between the NHS and other service providers in the provision of mental health self-care support services for CYP.
Stage 2 was conducted as a collective case study . A case study is an empirical enquiry that focuses on a single phenomenon in its real-life context, especially useful (as in our circumstances) when description or explanation is required. 181 Collective case studies are those in which multiple cases are studied simultaneously or sequentially in an attempt to generate a broad appreciation of a particular issue. 182 Yin 181 (p. 6) defines a ‘case’ as a ‘bounded entity’, a broad and flexible definition that allows the case to be as varied as an event, an individual, a service or a policy. In this project we have defined the case as a ‘mental health self-care support service for CYP in England and Wales’.
Sampling and recruitment
A purposive sampling strategy was employed to ensure that the various dimensions of the self-care support typology we derived from the mapping exercise and systematic reviews (see Chapter 4 , Table 19 ) were reflected in our sample. Accordingly, sites were recruited to include a variety of theoretical bases (e.g. cognitive–behavioural, social learning, recovery) and platforms (e.g. face-to-face or remote, group or individual). We also recruited on the basis of organisational characteristics, such as the sector the site operated in (e.g. NHS vs. local authority vs. voluntary sector) and the site leaders (e.g. health professionals vs. other trained workers vs. volunteers). It was also important to include key characteristics of the study population; thus, the sample included sites offering condition-specific and more generic support, CYP from different age groups, and different types of location (urban, rural) across England and Wales. Using the typology and these characteristics, six potential sites were selected from our sampling frame of 33 services (delivered by 27 providers), and these were approached to participate in the study. One site declined to participate so an alternative, similar in terms of typology dimensions and characteristics to the site that declined, was invited to participate and agreed.
The six sites which agreed to participate were:
- a psychotherapy group for young people aged 14–17 years who self-harm and their families, provided by the NHS in an urban area of England
- a group intervention (Dina School) for children aged 5–6 years with emotional and behavioural difficulties (EBD), based on The Incredible Years 183 programme and provided in rural Wales by the voluntary sector
- a parenting group for parents of children with EBD, based on The Incredible Years 183 programme and operating in rural Wales as a joint NHS/local authority initiative
- a resilience-focused family support service for families of children aged 5–14 years with emerging EBD, provided by the voluntary sector (but local authority funded) and operating in an urban area of England
- a national, recovery-focused online support group for young people aged up to 25 years with eating disorders
- a supported online cognitive–behavioural intervention (Beating the Blues 184 ) provided to young people aged 14–30 years with depression and/or anxiety by the voluntary sector in an urban area of England.
Recruitment of participants at the case study sites was also purposive in that it was driven by the characteristics of the particular self-care model employed. Additionally, to ensure a range of relevant perspectives, the views of younger, as well as older, children, and those of parents and staff with differing roles providing the services were sought.
Regarding the recruitment of service user participants (i.e. CYP and their parents), we received valuable advice from the SAG on engaging these participants in the study. Recruitment documentation (the covering letter, participant information sheets, contact form and consent/assent forms; see Research ethics and governance below) was developed with guidance and feedback from CYP. At five of the sites, staff provided the recruitment documentation to current and ex-service users (or to their parents if they were aged 14 years or below), via the post or by handing the documentation to users when they attended the self-care support service. Participants provided their contact details using the contact form and the researcher (Elvey) telephoned them to arrange the interview. For the eating disorders online support site, the study was publicised, including contact details for the research team, on a web page listing details of current research projects wanting to recruit participants, via an e-mail distribution list of service users who were willing to be contacted about research projects, and via the site’s Twitter feed. CYP participants were eligible to participate only if they were aged between 5 and 17 years. Although two of the sites (sites 5 and 6) did not offer services specifically tailored for CYP, they were eligible for this study because they did offer services to those under the age of 18 years. Non-professional participants (i.e. CYP and parents) were offered £10 in gift vouchers as a token of thanks for their participation.
Recruitment of staff at each site was facilitated via a key contact, usually a service manager, who not only took part in the research, but also identified additional relevant staff to invite as participants. At five of the six sites, staff were provided with the recruitment documentation, either through the post or in person by the researcher; at the eating disorders site, documentation was supplied via e-mail.
Research ethics and governance
Like all empirical research conducted within a university setting, the case study was subject to ethical approval by the host institution, the University of Manchester. Moreover, because the research involved potential access to NHS sites and NHS patients, the ethical aspects of the study required consideration by the NHS National Research Ethics Service (NRES) prior to any consideration by the university. Regulations introduced by NRES in 2011 185 allowed an expedited proportionate ethical review in circumstances where a project had no material ethical issues . NRES provides a tool 186 to help researchers identify whether there are material ethical issues or not, and use of this tool suggested that our project might be eligible for such an expedited review. This turned out to be the case and a favourable ethical opinion was obtained through proportionate review in March 2012. As is the standard procedure, this favourable opinion was accepted by the University of Manchester Research Ethics Office shortly afterwards. While conducting the case study research, it was necessary, on two occasions (in September 2012 and October 2012), to inform NRES of a ‘substantial amendment’ to the ethics-approved protocol. One amendment was required because one site requested that the wording on the covering letter be modified to remove the term ‘mental health’. The other arose because another site worked predominantly with children aged 5 years, so we asked that our original lower age limit for CYP participants be reduced from 6 to 5 years. Both of these amendments NRES subsequently approved.
Ethical research is underpinned by three inter-related factors: (1) informed consent; (2) the safety of participants and researchers; and (3) the safeguarding of any data obtained during the course of the research.
Regarding informed consent, all identifiable participants received an age-appropriate participant information sheet informing them of the study’s nature and purpose. The participant information sheets and associated consent/assent forms were designed according to NRES guidance. 187 The versions specific to CYP, furthermore, were piloted with colleagues’ children, students at a local secondary school and young people with experience of mental health services, and were subsequently amended as a result of their feedback. Written consent was obtained from all adult participants. In line with NRES guidance, 187 all CYP participants aged 15–17 years provided their own written consent; parents provided written consent for children under 15 years old, although, in line with good practice, written assent was also obtained from these children. We needed to take a slightly different approach to consent for the online eating disorders support group (site 5). We were interested in postings on the site’s discussion boards – postings that were both anonymous and publicly available. As the postings were anonymous, it would have been very difficult to obtain individual consent for the use of these postings, so we obtained ‘proxy’ consent to access and use these postings from the eating disorders organisation providing the service.
Regarding the safety of participants and researchers, the principal risks identified for participants were that they might get upset during the interview or disclose information (e.g. in relation to child protection) that would require action by the researcher. Written protocols were prepared for both of these situations. Risks to researcher safety were minimised by adherence to the University of Manchester’s guidance on lone working.
Data safeguarding requires that confidentiality and anonymity issues be addressed, not only in the conduct of the research but also in the reporting and storage of any data associated with the research. To preserve anonymity, the data generated by the research were, wherever possible, stored with identifying features removed. In any case, the data were stored securely, with due regard to confidentiality and in accordance with the University of Manchester’s information governance regulations. When the data were circulated around the study team or SAG, analysed or (as is the case here) reported, we ensured that any identifying features were removed.
At each case study site, we complied with any specific research governance requirements. This included complying with NHS Research and Development requirements at the NHS sites selected.
Data collection and management
Case study research requires data from a variety of sources and, once collected, the data should be managed systematically. 181 Data were obtained through semistructured interviews, documentary review and virtual non-participant observation and, wherever possible, from all three participant categories: CYP, parents and staff.
Semistructured interviews
Semistructured interviews were used as the main data collection technique. They were conducted with staff at all six sites and with CYP and/or parents at all sites except the eating disorders online support site. Pragmatism largely dictated the way in which participants were interviewed in that they were given choices as to which approach they preferred (e.g. telephone vs. face to face; individual vs. group). Forty-two interviews involving 52 participants were conducted; 37 were conducted in person, either at the site’s premises or at the service user’s home, and five were conducted via the telephone. The majority of interviews (35/42) were individual, five were joint interviews with a child or young person plus parent, one was a group interview with a child, parent and sibling and one was a focus group of four young people. The interviews ranged in length from 10 minutes (for some of the youngest children, aged 5 and 6 years) to 1 hour and 20 minutes. Interviews were facilitated by the use of topic guides, copies of which can be found in Appendix 12 . All of the interviews were digitally audio recorded with the permission of participants and the recordings were subsequently transcribed verbatim by a professional company.
Documentary review
Where available, relevant documentary evidence was collected from each site. For sites 5 and 6, documentary evidence was obtained simply from the relevant websites of the services. More comprehensive data were obtained from the other four sites, including a referrer’s leaflet for site 1 as well as a printed self-injury ‘toolkit’ used in providing the self-care support service there; a Microsoft PowerPoint general presentation about the Incredible Years services at sites 2 and 3, and one about the funder’s strategic plan regarding these services; an information leaflet about Dina School training for teachers at site 2; and information leaflets about the site 4 service for referrers, parents and CYP. The documentary evidence largely served to provide a contextual background to, and additional understanding of, the six sites.
Virtual non-participant observation
For the eating disorders online support site (site 5), we collected the data via ‘netnographic’ non-participation observation, adopting the principles of a method designed specifically for health-care research. 188 , 189 Netnography is a form of ethnography used in the study of online behaviour, and as ethnography concerns everyday routine behaviours in a natural setting, 190 netnography was an entirely appropriate method of observing a service that operated entirely online. The service centred around discussion threads that were organised by the providers into nine boards, following themes such as ‘recovery’, ‘caring about someone’, ‘introductions’ and ‘poetry’. Two boards were excluded from the study as the content merely described how to use the boards. All postings over a 4-month period (August to November 2012) were collected from the remaining seven boards. These comprised 114 discussion threads with more than 500 individual messages, each of which was screened for relevance. The postings were copied from the website and pasted into Microsoft Word 2010 documents (Microsoft Corporation, Redmond, WA, USA) prior to analysis.
Regarding management and coding of the data, the three data sets – interview transcripts, background information about the sites (documentary evidence) and the online group postings – were imported into NVivo 10 (QSR International, Warrington, UK), computer software designed to assist in the collection, organisation and analysis of qualitative and mixed-methods data.
Data analysis
The data were analysed using the framework method, 191 , 192 which has five stages: (1) familiarisation; (2) identifying a thematic framework; (3) indexing; (4) charting; and (5) mapping and interpretation. For the interview data, familiarisation was achieved by all of the transcripts being read by the team member who conducted the interviews (Elvey; Kendal also facilitated one group interview), and through other members of the research team (Kirk; Kendal; Pryjmachuk; Catchpole) each reading a sample of transcripts. For the virtual non-participation observation data (site 5’s online postings), Elvey and Kendal undertook an analogous process in that they treated the Word documents into which the postings had been pasted as ‘transcripts’. Following familiarisation, the study’s research questions and the topic guides (see Appendix 12 ) were used to devise an initial thematic framework. Using this initial framework, data from the transcripts (including the online postings) and the background documents obtained from each site were then indexed by Elvey in order to produce an initial chart for each of the six sites. An example of such a chart is provided in Appendix 13 . These six charts were then circulated around team members and a final thematic framework was developed through an iterative process, whereby we met as a team several times to discuss the data and any emerging salient themes. As the final thematic framework emerged, the data from the six initial charts were assimilated into a single chart which was used to guide our analysis and interpretation of the case study findings. The final thematic framework is outlined in Table 22 in the Findings section of this chapter, and Appendix 14 illustrates (using one of the themes, ‘facilitating self-care support’, as an example) how data from each of the initial charts were subsequently assimilated into a single chart.
Themes and subthemes emerging from the case study data
- Characteristics of the case study sites
Details of the six case study sites are summarised in Table 20 and described in detail below.
Details of the six case study sites
Site 1: self-harm psychotherapy group
This NHS service was designed for young people aged 14–17 years who self-harm; it also offered some support for the families of these young people via family support groups, and families could telephone the service and talk to staff between sessions. The service was run from an outpatient setting at an NHS mental health hospital. The service operated within a recovery-focused philosophy and was eclectic in its approach, in that the group intervention employed elements of group psychotherapy, CBT, Linehan’s dialectical behaviour therapy 193 and supportive counselling. Groups ran on a weekly basis (weekday mornings), lasted 2 hours and were led by nurses and support workers. Although the service was manualised – in that there was a specific protocol in place for how the service should be delivered – there was no limit, other than reaching the age of 18 years, to the number of weekly sessions a young person could attend. Young people were referred to the service via community or inpatient services.
Site 2: Dina School
The incredible years.
The group for children with emotional and behavioural problems (site 2) and the parenting group (site 3) were interconnected, but separate, services. Both operated as part of Webster-Stratton’s The Incredible Years programme 183 that had been adopted region-wide (across the local authority area) by the commissioning bodies in the region. The Incredible Years is an evidence-based programme, influenced heavily by social learning theory. It emphasises attachment, relationship building and emotional coaching, with a focus on children learning through play and parents and teachers spending time with children, listening to them and giving them positive feedback. The overall Incredible Years programme comprises universal and targeted (indicated) interventions, both of which were available in the region. At the time of data collection, around half of the region’s schools were Incredible Years schools. In these schools, all staff members were trained in the approach and were thus able to implement the programme universally (in a regular classroom setting, for example) or in a more targeted way.
Dina School
Site 2 was an example of a targeted intervention operating in one of the Incredible Years schools. Known as Dina School, it involved children taking part in 18 weekly, small group sessions, which took place in a room at the children’s school. The groups were facilitated by two classroom assistants, who delivered the programme as set out in the Dina School manual. The programme makes use of a dinosaur puppet called ‘Dina’ (which was also used universally in the main classroom setting) as well as two additional character puppets, ‘Wally’ and ‘Molly’. These puppets were used in role plays, demonstrations of behaviours and communication techniques and in video vignettes. Each session followed a similar format, with a review of the ‘homework’ tasks that were set at the previous session, followed by activities and games and the setting of a further homework task at the end. Parents came to collect their children at the end of the session which coincided with the end of the school day.
Site 3: parenting group
Like site 2, site 3 was a targeted programme. It was one of more than 20 Incredible Years group parenting programmes that operated in the same region as site 2, offering parent training to parents of children aged from 0 years upwards, grouped according to the children’s age. The parenting group participating in this study was for parents of preschool children, aged 2–4 years, who wanted support with their child’s behaviour or communication (e.g. being withdrawn or having tantrums that the parent found difficult to deal with). Parents could self-refer or be referred to the service. The service was provided by a voluntary sector organisation and operated from its premises, although it was commissioned and funded jointly by the NHS and local authority. Parents attended 15 weekly group sessions which were facilitated by two members of staff with backgrounds in family and youth work, and in accordance with the programme manual.
Site 4: resilience-focused family support
Site 4 was a voluntary sector family support service provided to families of children aged 5–12 years with complex emotional and behavioural needs who did not require Tier 3 CAMHS care. Some children were referred to the service because their needs were not seen to warrant CAMHS input; others had attended CAMHS and were subsequently referred to this service for the more generalised support with coping and resilience that it offered. The service is based on the Daniel-Wassell model of resilience, 194 a model with six domains – secure base, friendships, talents and interests, education, positive values and social competences – that have some affinity with the principles of recovery. Staff members work through these domains with families to identify the family’s needs and then focus on those domains where the most support is needed. The family support was delivered by a member of staff from the voluntary organisation operating the service. The staff, who had a variety of professional backgrounds including youth work, social work, psychology and nursing, met with the child and his or her parent(s) individually (sometimes together) at home and at school. As with The Incredible Years, this service was manualised with a prescribed number of sessions.
Site 5: online eating disorders discussion board
This site, operated by an eating disorders charity, consisted of online message boards for young people concerned about, or experiencing, eating disorders. The message boards were established around 6 years ago to improve access to support. Although the online eating disorders service was a ‘virtual’ service, operating entirely over the internet, the charity operating the service offered some other services for young people including a telephone helpline and a live online chat service which some message board users had also participated in. Like the self-harm service, this service operated within a recovery-focused philosophy. To post messages, users had to register on the internet site (supplying their name and e-mail address). Although the posts were moderated, they were freely available on the internet for anyone to read. The boards were organised into themes, and users posted messages that mostly described their worries about food or eating, or their experiences of living with eating disorders, as well as messages that sought support from others or offered emotional support and practical tips to others. The boards were moderated by volunteers, many of whom had experienced eating disorders themselves and some of whom had trained in relevant fields such as counselling. Although the service was open to young people up to the age of 25 years, it was eligible as a case study site because those under 18 years of age were represented in the postings. Unlike the other five sites (which were manualised to one degree or another), this service was inherently spontaneous and adaptable.
Site 6: supported online cognitive–behavioural therapy intervention
Site 6 was a charity-operated, supported online CBT service for young people with anxiety or depression aged between 14 and 30 years. Although the service was open to people up to the age of 30 years, it was, like site 5, eligible as a case study site because those under 18 years of age used the service. The service had been established by staff at the site who had had prior experience of anxiety and depression themselves. It was set up in response to a perceived gap in suitable service provision for young people and young adults and aimed to appeal to this group by being accessible and flexible. The site operated as a drop-in centre, whereby people could come without an appointment and access information and advice. Service users came to the charity’s base and worked through a specific online CBT course – Beating the Blues 184 – with a volunteer from the charity facilitating the young person through each CBT session. Like most CBT interventions, this service was manualised with a prescribed number of sessions.
- Participant characteristics
Table 21 summarises the interviews conducted at each case study site. In total, 52 participants were interviewed between July 2012 and March 2013. The CYP ( n = 17) who took part ranged in age from 5 to 17 years. Of these 17 CYP, four were interviewed as a focus group (at the self-harm group psychotherapy site), and six were interviewed along with a parent, five at the family support site and one at the self-harm site. Of the 15 parents who took part, nine were interviewed individually and six along with their child. Two of the individual parent interviews at the parenting site were conducted via the telephone. The service provider staff interviewed ( n = 19) included nurses, psychologists, classroom assistants, social workers, youth workers, counsellors and lay volunteers. Three members of staff at the family support, group parenting and eating disorder sites were interviewed over the telephone. The majority of staff and family members were female; two male staff members and three fathers were interviewed. Of the six young people interviewed at the self-harm and anxiety/depression sites, half were male and half female; at the sites where younger children were interviewed, most (8/11) were male.
Participants by site and category
Although the overall quantity of data is sufficient for a case study, 195 a few observations need to be made about the relative success of our recruitment strategy across the six sites. Recruitment was relatively successful for all three participant categories across sites 1, 2 and 4, though only having one parental interview at site 1 was disappointing. Site 3’s recruitment was also reasonably successful given that parents were the target of the service and that, as they were under 5 years of age, we did not have ethical permission to interview the children. We did not attempt to recruit parents at sites 5 and 6 because the very nature of the services at these sites meant that it would be difficult to identify parents. The low numbers of staff participants at these two sites was also understandable because these services – both provided by the voluntary sector – had limited resources to employ significant numbers of staff. With site 5, we did not manage to recruit any CYP participants for interview despite advertising on the service provider’s website and through other online networks. Though disappointing, this is not an especially serious recruitment limitation as any interview data obtained would have merely augmented the CYP’s perspectives on self-care support which we obtained via the netnographic non-participation observation data.
Site 6 perhaps created the most significant recruitment issue in that we only managed to recruit one CYP participant at this site. This site was a relatively newly established service which was operated by a small organisation with one full-time member of staff. We recruited via the service manager who asked that we involve only ex-, not current, users of the service. The service manager searched the contact database and telephoned or sent information to all ex-users inviting them to participate in an interview. During the 7 months that we were in contact with the site, only eight people aged 17 years and below accessed the service. Two agreed to be contacted by the research team and subsequently participated in interviews, one of whom has since taken on a role as a volunteer providing the service.
From the analysis of the case study data, four principal themes emerged, each containing a number of subthemes. These themes and subthemes are summarised in Table 22 and discussed in more detail in the ensuing sections. At this point, however, it can be noted that the first two themes mostly provide contextual detail about, respectively, the users and providers of mental health self-care support services for CYP, whereas the remaining two focus largely on the factors contributing to the acceptability of such services.
Having a mental health problem
This theme provides some contextual detail about CYP’s and their families’ understanding of the mental health problems experienced prior to using the services at the case study sites, their understanding of self-care in the context of these problems and their experiences of any self-care support received.
Understanding the mental health problem
The conceptualisation of CYP’s difficulties specifically as mental health problems appeared to be connected to the CYP’s age. The youngest children interviewed, aged 5 and 6 years, did not describe having any mental health problems or difficulties themselves. School staff and parents tended to think that these children mainly lacked confidence or had difficulties expressing or managing their emotions. Some parents described emotional outbursts and tantrums and two described their children as being ‘unhappy’.
I had concerns about his behaviour; he would break down into quite severe tantrums that would last for 20 minutes . . . he would spit all over the seats . . . strip naked and hit and lash and kick; hurt himself, hurt me. And generally I just felt that I had this unhappy child on my hands … I couldn’t go out with him . . . So I was kind of feeling trapped in my own home because of his behaviour. Parent of younger child
Older, primary school-age children and their parents described various emotional and behavioural problems: being unsettled or disruptive at school; having emotional outbursts at home; having problems with family members or in making friends; lacking confidence; and having communication problems, especially in expressing emotions.
Me and my mum didn’t really use to get along, and not able to cope, like, and with my brother and sister, I didn’t know how to be responsible and stuff. Child
Young people – that is, older children – who had used the self-harm (site 1), eating disorders online support (site 5) and depression/anxiety (site 6) services had a wide range of experiences, from severe mental health problems and diagnosed conditions, to milder symptoms and difficulties. Some attendees at the self-harm site had been diagnosed with depression and others described feelings of low mood, anxiety and intense feelings. Staff at the self-harm group mentioned a variety of self-harm that users presented with, including cutting and burning. Some CYP attending the self-harm (site 1) and family support (site 4) services had experienced more than one type of difficulty or problem, including being bullied at school, not attending school, displaying signs/symptoms of autism, family relationship problems and misuse of alcohol and/or drugs.
Self-care and self-care support
Just as participants described a wide range of mental health problems and difficulties, their experiences of self-care and support for their problems and difficulties prior to accessing the services were also mixed. Obtaining support was sometimes related to their understanding of the specific mental health problem, as in the case of one young person who had struggled with depression over an extended period:
Interviewer: So had you had any help with your depression before you went to the centre?
Young person: No, none, not at all. I had little understanding as well, it wasn’t something that had been spoken about.
Participants generally described undertaking little self-care before coming into contact with the services. Nonetheless, some parents whose children had attended the Dina School groups (site 2) had also previously attended an Incredible Years parenting course and had used some of the approaches at home. A few parents mentioned using techniques from books or television programmes such as Supernanny . Across most of the sites, the situation for many participants was that they came into contact with the services at a point when their problems had emerged, but they had rarely engaged in self-care themselves or received support they were happy with.
With some of the older children (young people), there was some evidence that they could make rational choices regarding self-management, especially when it came to medication:
Young person: I usually forget to take it, or I intentionally go out my way not to take it, because I feel as if I don’t need it and it makes me feel different . . . I was on Sertraline, but it kept me awake and then I was on Mirtazapine and then some other things . . . I didn’t like them . . . I don’t feel as if meds help me.
Another young person: I’m on medication at the moment, because my depression has peaked at the moment . . . so it [the medication] does work.
However, these choices were not always adaptive, as in these examples of young people ‘self-medicating’ with alcohol:
Young person, interviewed in a group: I used to drink and hide in a tree to drink, because my mum wouldn’t allow it, so I used to hide and had to go in a hole and fall out of a tree regularly drinking, that’s how I coped.
Second young person in the group: Yeah. I used to think alcohol helped me, but it used to just make me worse.
Regarding the support received, there were participants at all of the case study sites with experience of accessing some form of health care or support prior to attending the self-care support service; CAMHS, social services, GPs, psychiatrists, paediatricians, school counselling services and social services were all mentioned. For example, some families had a history of contact with social services due to family situations and some parents had sought help because they were concerned that their child might have an autistic spectrum disorder. There were some reports of positive experiences, such as helpful school counsellors, health visitors and other workers:
My outreach worker who works with me to integrate into the community, because I’m, kind of, agoraphobic, I don’t like people, crowds, so he works with me to try and get me into the community. Young person
However, many negative experiences were recounted where families had felt dismissed when they raised concerns, for example, about their children’s behaviour or social understanding and had found support hard to access. The mother of one child who had previously been referred to community-based mental health services had found the care provided inadequate:
It didn’t help much, she used to just enjoy going there because I was doing all the talking, they would watch her play, so it wasn’t . . . [helping her with] expressing her feelings . . . and then it just kind of stopped, they were thinking she didn’t need it, but she’d got so much anger at the time, she wanted to leave the house . . . I was worried for her. Parent
Two settings in particular were singled out for criticism by young people: mainstream schools and inpatient hospital care. Young people had experienced bullying at school, including being bullied about their mental health problems by other students. Some had stopped attending mainstream school and were at school units and felt that staff at mainstream schools often struggled to help students who self-harmed:
They’re not trained in mental health and are only really equipped to do with stuff, like, things to do with education and . . . bullying and peer pressure . . . they’re not equipped . . . they really don’t have a clue when it comes to stuff like mental health and things like self-harm . . . I had a really bad experience with my mentor. Young person
In terms of hospitals, participants described how support for self-harm in inpatient settings focused mainly on preventing physical harm. For example, two participants reported being restrained and put into seclusion (actions which could both be seen as punitive) when staff found that they were in possession of objects which the staff thought the young people would use to self-harm. Participants had found that they could access either group ‘talking therapies’ or an individual to talk to in the units, but had found this problematic because the therapy was not suitable for them at that stage, or because staff did not spend enough time with them:
Young person, interviewed in a group: There’s people there all the time that you can talk to, [but] I think the therapy puts quite a lot more stress on you at the very beginning . . . you’re taken out of your house . . . kind of throw you in with a bunch of new people, that’s hard to deal with . . . it’s a lot harder to then feel comfortable . . . I think, I had therapy twice, it didn’t work, so they basically just left me.
Second young person in the group: [My named nurse] was on nights and then when she was on days, she didn’t speak to me anyway, that was so unhelpful. She came to my room at like half past 10 and I’d be talking about stuff and getting upset and minutes later I had to try and sleep.
Young person: Yeah I had some nights when mine was . . . on nights and the head of [name of department], so he really didn’t have time [for me].
Running throughout the narratives of the young people was a recurring sense of anxiety around accessing support. Feeling alone, not knowing where to turn for help, discomfort and worry about discussing their problems with family or friends were mentioned repeatedly. The following data extract was taken from one of the site 5 message boards:
When you realise youve got some kind of (eating disorder) what was the first thing you all did? It’s just im stuck and going nowhere, the idea of food and excercise is going round and round in my mind, having crazy thoughts in my head all the time- but i cant tell anyone or even talk about it to anyone because i could shy when it comes to spilling out information about myself . . . any help? Pleasepleaseplease . . . ALSO, if you call the youthline what do they ask you and stuff? because I really wanna call them but im scared of the reponse and over the phone (procedure). Young person, verbatim message board posting
Providing self-care support
This section explores the findings relating to staff views about providing self-care support services, their reasons for involvement, training and supervision, and the extent to which their service is integrated with other services.
Service development
Staff at the sites became involved in the services for a variety of reasons: a desire to change things or innovate on the basis of personal, often negative, experiences of mental health services; wanting to improve the evidence base for practice; and often just sheer enthusiasm to help CYP. For example, the manager of one site had been motivated to found an independent alternative to traditional ‘clinical’ approaches on the basis of personal negative experiences elsewhere:
I started to experience the onset of depression and anxiety and looked at what sort of support or help was available to me and there was nothing that I felt I would have been likely to access or appealed . . . so I . . . basically came up with a service that I would have liked to see when I was in that situation and applied for funding and got it. Service lead
At another site, the service lead had been influenced by observations from her own practice, at a time when there was a perceived ‘epidemic’ of self-harm among young people and generally insufficient support available, and when anxiety about the risk of serious harm, including suicide, was high among staff who worked with young people. The rationale behind setting up a group therapy service was that a group approach could be appropriate for young people because of the influence and importance of peer groups to this age group. Moreover, improvements in peers would be clearly visible in a group setting and so serve as a vehicle for hope and optimism in other group members.
The Incredible Years programme, on the other hand, had been adopted at two sites because of its perceived strong evidence base:
I felt really strongly that I knew that the programmes were blueprint [evidence-based] programmes . . . that met the high standards for replicability and for research . . . I really, really like the Incredible Years model. Staff member
Moreover, service development seemed to be coupled with service leads who were enthusiastic and highly motivated, even to the point of being ‘on a mission’:
So it kind of became my mission and it’s grown into the mission for the Authority to develop all of those programmes. Service lead
Across all six case study sites, the attributes of the service leads in particular were suggestive of a high level of leadership skills, in that there was evidence of innovation, planning, empathy (for CYP, parents and colleagues), motivation and communication.
Training and supervision
All of the sites except the online eating disorders site (site 5) were manualised, that is there was a specific written manual in place for how the service should be delivered. The Incredible Years sites (sites 2 and 3) and the anxiety/depression site (site 6) were guided by manuals that prescribed the topics to be covered in each session; the self-harm (site 1) and family support (site 4) services had manuals that were less prescriptive.
At the self-harm site (site 1), all staff running the groups were provided with the service manual and, as part of their training, they also observed groups prior to becoming a group leader. Staff running the groups met monthly for group supervision with the service lead. On its initial formation, staff at the family support service (site 4) had been trained in the resilience approach by its architects. New staff members were first introduced to the model and subsequently trained by the service’s current staff, as well as receiving clinical supervision from a psychologist. At the anxiety/depression site (site 6), training was provided by the company supplying the CBT programme and all volunteers had to work through the course before working as a volunteer; there was no formal clinical supervision in place at this site, however.
The two Incredible Years services (sites 2 and 3) were different in that, of all the sites, they had the most structured and formal arrangements for training and supervision. To deliver a programme, staff members were required to undergo formal training. Staff members were regularly supervised by local colleagues and there was ongoing monitoring from the programme base in the USA. The service lead explained why she thought the training and ongoing supervision and support were important:
We’re using an evidence-based programme and actually unless you really are delivering with fidelity we know that you can’t guarantee that you’re going to get the same results as [the] research . . . everybody who delivers the group in [area name] can be sure they’re either going to be able to work with [or get] supervision from someone who’s accredited either as a peer coach or as a mentor . . . I think that is really important in making it effective. These are hard groups to run, so it’s important ensuring that people do get the support. Service lead
Fidelity was not emphasised as strongly at any of the other sites. This is perhaps because fidelity can be in opposition to flexibility, a characteristic seen by many as a key factor in a service’s accessibility, as will become apparent when the next theme, Accessing self-care support , is discussed.
Integration with other services
As outlined earlier in the site descriptions, the two Incredible Years sites (sites 2 and 3) had been widely adopted by local commissioning bodies. These services were closely integrated with local planning and commissioning structures and with the local education, health and social services sectors. The Incredible Years services were an exception, however. None of the other services had this level of integration with health, education and social care. The family support service (site 4) was integrated in as much as it was run by a voluntary sector organisation but funded by a local authority, with clinical supervision provided by an NHS psychologist. It also had close links with special educational needs co-ordinators (SENCOs) in schools and could form part of an action plan arising from national ‘Common Assessment Framework’ 196 assessments. Staff at the family support service, however, perceived that there were overlaps between their work and that of the NHS and social services, and that they fitted into a niche between the two.
The self-harm group (site 1) was run from a NHS mental health trust, at a CAMH day service. The service is attached to an inpatient unit with residential and non-residential care and education provision. Self-harm groups using the same principles are run at other NHS locations in the region, and although these groups are integrated with other services to the extent that GPs and consultants can refer CYP to them, they are usually run as ‘standalone’ services with little integration with the NHS CAMHS provider delivering them. The eating disorders (site 5) and depression/anxiety (site 6) services were provided by charities dedicated to helping people with particular difficulties in these areas. The depression/anxiety service was run by a small, relatively new organisation which provided some other activities as well as the supported online CBT, and to some extent could be seen as an alternative, rather than a complement to, statutory services. Regarding the eating disorders charity operating at site 5, integration tended to be limited to ‘signposting’ in that message board posters often offered advice to other board users about how to access statutory services, encouraging users to overcome their anxieties in accessing such services and offering opinions about those services.
Where integration was most evident was in the referral processes at the various sites. This is discussed further in the next section.
Accessing self-care support
This theme, and the next, will present findings on the acceptability of the self-care support services, both in terms of their general accessibility (this theme) and the perceived attributes that services and their staff possess that facilitate CYP and their parents to care for themselves (the next theme). Regarding general accessibility, two key subthemes emerged from the data: one pertaining to referral and one focusing on engagement.
Referral to services
Children, young people and their families had accessed the services via a range of routes, including self-referral, signposting and referral by professionals. The self-harm (site 1), family support (site 4) and parenting group (site 3) services were well integrated into referral pathways and several CYP and parents at these sites had been referred in this way. Several postings on the eating disorders message boards (site 5) mentioned being ‘signposted’ to the board by health professionals, including psychologists and doctors. The parenting group (site 3) and anxiety/depression (site 6) sites encouraged self-referral and publicised their services; some parents had found out about the service through leaflets in their child’s school bag, or through a friend. The anxiety/depression site was advertised through posters and leaflets in shops and bars as well as through presentations at schools and Sure Start centres. At Dina School (site 2), staff at the school had approached the parents of children who they thought would benefit from the service and asked these parents for consent to include their children in the group. Schools were a common source of referrals for the family support service (site 4) and two children who participated in the study had been referred by school staff, one by a SENCO and one by a school nurse. The young person interviewed at the anxiety/depression site (site 6) had self-referred to this service following a presentation at school; in interview, the service manager expressed disappointment that no school nurses had made referrals to the service.
One family who had attended the family support service recalled a long wait (around 2 years) from becoming aware of the programme to the time when they started receiving the support. Waiting times were not cited as a problem, however, by other study participants.
Building and maintaining engagement
In building engagement with health-care services, one of the first barriers to overcome can be the physical access to services. The participants at all of the case study sites seemed to encounter few physical barriers to access, though it should be added that we did not recruit those with probably the best information about barriers to access – ‘dropouts’ from the services – to our sample. For the physically provided services, none of the CYP or parents reported particular problems with travel to the sites. The virtual eating disorders support site could be accessed via the internet at any time, although messages were only uploaded when staff members were available at the service to moderate them (until 20.30 on weekdays and until the afternoon on Saturdays). The Incredible Years services (sites 2 and 3) covered a large rural area and were provided in convenient venues across the region. The young people at the self-harm group site (site 1) were all at school or college and often had to miss school or college to attend the service, though none of the young people interviewed raised this as an issue. These young people were mostly brought by car to the service by their parents. There were several examples of staff working to make services convenient to attend, or taking the service to the families. For example, staff at the family support service (site 4) worked with families in their homes and with children at school. The parenting group (site 3) was generally provided in a group setting but could be run by staff on an individual basis at people’s homes if necessary:
Staff member: It’s very different to a traditional service where you might send out an invitation and if the parents don’t come then . . . they might say that you might not be able to access the service. With Incredible Years it’s more about going out and getting the parents really. So it’s about awareness raising, training lots of agencies who know about the programme . . . but [also] offering really nice coffee and biscuits. If parents miss a session, [it’s] really important that they have the hand-outs. So, if it’s possible, the leader goes and visits them at home.
Another staff member: Recently we’ve had a case [where] mum . . . is not ever there physically when we turn up for our appointment . . . so our worker . . . she’ll go to the child’s nursery . . . to try and catch mum at a drop-off, just to have that initial face-to-face engagement because we were mindful that this is a mum who is surrounded at the moment by professionals who are all breathing down her neck, and we wanted to make sure that mum had a fair view of where we were in that process, what our role is and that we’re not scary monsters who are trying to trip her up.
Flexibility in service provision seemed to be a key in not only building, but also maintaining, engagement with CYP and their families. As a member of staff at the family support service (site 4) outlines:
It’s looking at each case on an individual basis and thinking about what are the reasons for disengagement, why haven’t they engaged, is this a language issue, did they not understand when the appointment was, is it that the intervention isn’t working for them . . . It’s quite involved; but we don’t just do a kind of, if you don’t pitch up we send you a letter and then if you don’t pitch up again we bin you off to be picked up by some other agency – we will attempt always to get an answer. And then if it’s just that it’s not working, well, then we’ll have a conversation about that and let’s work it out. Staff member
Another example of the flexible nature of the services was the between-session support that the sites offered. At the self-harm (site 1), family support (site 4) and parenting group (site 3) sites, support in addition to the scheduled sessions was available, including staff being available to parents over the telephone if they wanted to make contact. Staff at these sites emphasised that they worked hard to engage people in the services and to maintain engagement once a supporting relationship had been established. However, a participant who provided clinical supervision at one of the sites provided an alternative perspective on this, suggesting that it was possible to be overly flexible in that, for example, always bringing the service to a family’s home could potentially discourage independence:
I think, the fact that they [the organisation] go out and work with families in their local area, either at home, or in schools . . . that’s really important . . . something that families will like [but] if you’re going to visit somebody at home then . . . how do you evaluate their motivation to change? Because . . . if you’re at home and somebody comes to see you then actually you don’t necessarily need to do anything to engage, other than sit and nod and make the right noises . . . but if you’ve actually got to physically leave the house and go somewhere, then that suggests that your motivation might be greater to engage . . . it’s trying to get the match between that initial buy in to the service [and maintaining engagement]. Staff member (from outside the organisation)
Some staff expressed an awareness of working with parents who were used to being highly monitored by statutory services and said this could sometimes be a challenge when working to engage parents initially. A school-based member of staff, for example, who had referred several children to the service observed:
You do have the odd family who you refer who don’t engage. And it’s very sad really . . . it’s usually . . . parents who have already got to the point of social services . . . [people think] oh, don’t get social services involved, they’ll take my children from me. And once social services are involved . . . they’re breathing down your neck all the time then, aren’t they? I mean, they’re popping in and out of your house all the time, they’re watching your every move, very intrusive. Staff member
Facilitating self-care support
This theme explores the perceived attributes that services and their staff possess that facilitate CYP and their parents to care for themselves. Key facilitators of mental health self-care support for CYP appear to be organisations and staff that are welcoming; a skills focus whereby CYP and parents are taught relevant self-care skills and then given the chance to practise these skills; opportunities for peer support; and the provision of time and attention.
Welcoming staff; welcoming organisations
Positive staff attitudes appeared to be particularly important. At every site (apart from the online eating disorders service), service users spoke spontaneously and positively about the staff running the service, using adjectives such as ‘nice’, ‘lovely’, ‘good’ and ‘thoughtful’ to describe them. Listening to CYP, allowing them to tell their own story and treating them with empathy and compassion, was also important. This was mentioned particularly by parents at the family support service (site 4) and the young people at the self-harm service (site 1), who liked the manner of the staff and contrasted this with previous, negative experiences at other services. Young people using the self-harm (site 1) and anxiety/depression (site 6) services in particular emphasised the importance of being able to trust staff in order to talk to them openly:
You have to feel comfortable talking to that person, if you don’t like them, then you’re not going to feel comfortable, so you’re not going to engage with them at the level that’s needed to help [you] recover. Young person
At several sites, CYP and parents perceived staff as wanting to understand and help them and felt that they were treated with care and compassion:
The service worker talked to me as if he’d been there before . . . went out of his way for me. Young person
It wasn’t just a job to her. Parent of a younger child
Knowing that the service would accept people for who they were and be open to hearing about their problems was an important attribute of the case study sites operated by voluntary sector organisations. Being non-judgemental or offering non-judgemental support was a particularly positive aspect:
You could be honest and say, ‘This is what my child has done’, and you weren’t judged. Parent of a younger child
Indeed, contrasts were sometimes drawn with other statutory or conventional health and social care services perceived (unfairly or not) as being judgemental. A worker who referred into the family support service noted:
You’ve got to the point where this has become . . . crisis time: ‘We’ve got a plan here in front of us, you will do this, you will do this, you will do this’ . . . whereas with [site name] it’s not, ‘you will do . . .’ it’s ’these are the suggestions that we can make, that will make things better for you’. So it’s not as judgemental, well, social services aren’t judgemental, I suppose, but it might feel like they are . . . I hear in lots of groups that I go to . . . ‘you’re all judging me, that I’m this, you’re judging me on that’. Staff member
A similar feeling was expressed in an interview with a young person at another site:
Young person: [With the general practitioner (GP) and] even with CAMHS sometimes . . . it seems a bit like I’m being judged, or it doesn’t seem like they’re there for me in the way that I’d like, but it was different with [site name], like, it definitely felt a lot more welcoming.
Interviewer: Okay. Is it the people at the GP and CAMHS? Or is it more general?
Young person: I think, it’s more the method, like, I mean, it’s just all about a feeling, it feels like if I’m at the doctors . . . it becomes a thing that I’m ill, or there’s something wrong with me . . . you still sit there and you feel like you’re being judged . . . it definitely affects your confidence when you’re trying to answer, like, the questions, like, confidently and with, like, full honesty . . . I don’t know, like, when I saw my GP I didn’t tell him the whole truth, just because I didn’t feel that comfortable.
Organisational features of the sites were also important in determining how welcoming a service was. In the earlier Service development and Building and maintaining engagement subthemes, we discussed how the service leads appeared to have a high level of leadership skills, and described how staff often worked hard to make services convenient to attend, or took the service directly to the families. There were also some comments about the premises that the services were delivered from. At two of the voluntary sector sites, staff explained that particular efforts had been made to ensure that the physical surroundings were attractive to young people, featuring, for example, bright colours and soft furnishings or having music playing. On the other hand, CYP at one site commented that the rooms in which the groups were held were somewhat small. The physical features of the premises, however, were overshadowed by spontaneous references that CYP and parents made to the welcoming ambience. Indeed, there was often blurring between organisational and individual staff attributes: ‘welcoming’, ‘friendly’ and ‘non-judgemental’ were used by CYP and parents to describe both the staff and the general atmosphere or ambience of the service, often in contrast to other services they had experienced.
Activities to build skills for self-care
The use of skill-building techniques and opportunities to practise such skills in their daily lives was considered an important feature of all six services. Children, young people and parents outlined a variety of practical activities and techniques, including games and exercises, which they had used in formal sessions (in vitro) as well as at home and in school (in vivo). Fittingly, given the nature of this study, most of these activities and techniques were designed to assist the participants in managing (self-managing) the CYP’s condition or problems. For example, in the self-harm group (site 1), young people were supported in devising coping strategies other than self-harming; in site 2, children practised communication skills at home that they had learnt at Dina School; and in the family support group (site 4), families were encouraged to action plan and set goals. For younger children in particular, a large proportion of their narratives consisted of their recollections of the various games and activities in which they had taken part. The youngest children stated that they had gone to Dina School to learn things and that they got ‘prizes’ (plastic chips) for doing well at the activities there:
Interviewer: And what did you get a chip for?
Child: When I’m doing stuff nice.
Many of these activities focused on identifying thoughts and emotions or on learning techniques to relieve anxiety or calm anger. These had been introduced by staff at the sites and also practised by children outside the sessions. The older primary school-aged children seemed to have more insight into the purpose of the activities and techniques:
We used to do these words about temper and then after that to calm me down we used to play a few games. Child
The parents who were interviewed also seemed to appreciate practical techniques and talked at length about implementing these at home. Reward systems including sticker charts were mentioned frequently, along with techniques designed to help children manage tasks and express their feelings:
I think it is important to have a task and try and complete it and stuff. Young person
I think she is responding well to positive rewards . . . she loves the reward charts . . . I give her a sticker just on her T-shirt if she’s done something really nice. Parent of younger child
And from an interview with another parent:
Interviewer: Are there any things in particular that you find helpful?
Parent of younger child: Well there was the words on the fridge . . . the fridge magnets spelling out, ‘I’m not happy’, ‘I’m . . .’
Child: ‘. . . sorry’.
Parent: ‘Sad’, ‘I’m sorry’ and . . .
Child: ‘I love you’.
Parent: ‘I love you’, yeah. We did that for a while. We lost all the pieces, like, we did it for a while.
Some games and techniques were ‘prescribed’ as part of the manual or workbook for the course. However, most of the activities allowed some personalisation such as tailoring rewards to the individual child. For example, staff at the family support service (site 4) found out what children were interested in or enjoyed and then looked for local activities or clubs they could join, such as football or the Boys’ Brigade. At the self-harm site (site 1), young people put together their own ‘tool boxes’ of distraction techniques, memorabilia and keepsakes that helped them reduce urges to self-harm. The service also provided support for caring for wounds that arose from cutting, and advice on ways to camouflage scars, with an organisation specialising in this visiting the group.
I’ve got this thing called a tool box in my room that I put all my different distraction techniques inside so, like, if I’m having a bad day, even if I’m not having a bad day . . . I could use the different things. And different things work at different times, so one time, like, writing out your feelings might be enough, or drawing might be enough, but sometimes you have to use a range of things to minimise that urge and sometimes nothing works, but . . . at least I’ve tried. Young person, interviewed with parent
The programmes delivered at sites 2 and 3 (the Incredible Years sites) and site 6 (the anxiety/depression support service) were supplemented by videos for participants to watch that contained vignettes or examples of role plays to augment the situations or techniques that the programmes considered. These were criticised repeatedly by staff and service users for being outdated and participants disliked that they had been filmed in the USA as they would have preferred British accents. One service user found them ‘idealised’ in that the actors looked too ‘perfect’ and suggested that videos featuring real people, not actors, would be more helpful.
Sharing experiences and peer support
Although a key aspect of all of the services at the case study sites was introducing CYP and their families to stock tools and techniques to help them care for themselves, an important aspect of skills building was supporting CYP and parents to discover self-care techniques for themselves. Often, this happened with the support of their peers, especially in the sites operating group-based approaches where other group members could play a key role in generating ideas or giving feedback. For example, children in the Dina School groups (site 2) took part in role plays and other interactions that helped them to think through how they could handle things that children might find difficult, such as sharing:
[Using a puppet to act out] snatching a book, [then discussing], is that kind?, is that unkind? . . . then after a while you’d get them to bring their problems in, you know, if you have a problem on the yard [playground], you know, if someone’s not listening to you, or doesn’t want to play, well, eventually they would come up [and talk about it with the group]. Staff member
Similarly, users of the online support service (site 5) frequently exchanged tips and techniques. Postings on the message boards often included users sharing self-care tips and suggestions with each other, and describing various relaxation or distraction techniques and activities such as reading, knitting, writing, drawing and exercising:
Listening to music is a huge relaxation thing for me, also drawing/writing – either a story, poetry or in a journal. Do you enjoy reading? To begin with i didnt have much concentration for reading, but now I am really enjoying reading again, and i find if i start reading after a meal when i am anxious that I can get lost in the book, and before i know it half an hour has passed. I’ve also tried knitting, but i’m a bit of a perfectionist so that didnt go so well. Hope you are ok, and that some of these tips may help you. Verbatim message board posting
The following were taken from two other sites:
They discuss coping strategies, like, they’ll say, like, if you get the urge to self-harm, what do you do? And they, sort of, come up with, ‘well, I’ll go and do this, I’ll go and put my favourite music on, my film, go for a walk, walk the dog, talk to my mum’ . . . and I do think it’s very beneficial. Staff member
I enjoyed the discussion. And what was nice is the feedback we gave each other . . . Because I think, that does you good, to have other people sometimes go, no, you’re good at that or why don’t you try this or why don’t you try that? . . . because you put it into practice with other people, it works better than you just reading books. Parent
Although the sharing of practical tips and techniques was an important element of peer support, the sharing of the experiences among CYP and parents was perhaps more beneficial. As discussed in the first theme, Having a mental health problem , some participants had not talked about their difficulties with other people prior to coming into the services and had felt alone with their problems. Staff members and attendees at several sites talked about the emotional benefit of being in a group with people who had had similar experiences, in that people who had previously felt isolated with their problems, or uncomfortable about seeking help for them, felt less alone:
It was actually amazing really; firstly because you realise that what your child was doing was normal and that all the other children were doing the same things. Parent of younger child
I think they listen more to their peers, their peers is pivotal, isn’t it, in adolescence, so I think the peer groups are very important, and that sense of belonging is good. And often . . . I’ve found that every single youngster who attends a group, is excluded from some aspect of their life, either from their family or from a peer group, because they’re bullied or they bully or, you know, they don’t fit somehow . . . So I guess being together with other young people helps you feel, you know, you’re not on your own with this. Staff member, another site
As well as receiving support from others, satisfaction gained from feeling that they had helped others was also important to some participants:
It was good for [my daughter] to see that she had helped other people, she liked that; that helped her as well. Parent of older child
As well as perceiving that the sharing of experiences was helpful, staff and parents felt that having a mixture of experiences and people at different stages of illness or recovery within a group provided additional benefits. The self-harm and parenting groups brought together people from different social groups who would normally not socialise together, but who had experienced similar problems, and this seemed to be helpful in terms of giving people a wider perspective on their problems, or perhaps developing empathy:
[They] have a good understanding of each other’s needs . . . it runs well because it’s a mixture . . . they’re all at different stages of their recovery . . . we’ve got young people who have been established for a long time and . . . have almost recovered, others are at the stage of contemplating, sort of, change and in the process of recovery and some that are not ready to change. And that’s, as I say, a very supportive group . . . those that are almost recovered, they do get and understand where [those who are less recovered] are coming from. Staff member
Very heterogeneous . . . you’d have youngsters in local authority care, and then you’d have very upper middle class young people, who were anxious about exams and stuff like that. And that actually works as well, because kind of sometimes it’s good to see people in other situations . . . you thought your situation was really bad, but actually, there’s people who are worse off, and something about that kind of gratitude about what you have got. Another staff member, same site
The participant quoted below, who described herself as ‘middle class and educated’ seemed to agree that this could be a benefit:
It sounds awful, but people that you might not necessarily have mixed with before, because you wouldn’t have had the chance, and got to know them . . . different social spheres . . . all of that’s broken down . . . [there can be perceptions that] . . . some backgrounds are better, supposedly, than others. And actually, you know, one of the mums in particular, who hadn’t got any further education . . . was just a fantastic mum. Whenever we’d . . . learn a new principle, when we’d feed back the next week, her and her partner had discussed it, and had both tried it . . . And it was nice to hear about other people, and there is a range of us, you know, people with partners, people without. Parent of younger child
The ‘sharing experiences’ aspect of peer support was complemented by others including the social aspect and what might be termed an ‘empowerment’ aspect. Regarding the social aspect, service users at the self-harm (site 1) and parenting (site 3) sites enjoyed attending the groups and especially liked the social aspect of getting to know others in the group. The parenting course (site 3) had an arranged ‘buddy system’ where parents were paired up and encouraged to telephone each other between sessions to talk about how they were getting on with their tasks or exercises, and some of these parents also reported forming friendships and continuing to meet socially after the programme had finished. From the focus group:
Young person 1: I prefer group talks, like, talking in groups, instead of taking medication . . . [at first] I was an inpatient so I was really struggling and . . . just having the support off people in the group was what I needed.
Young person 2: We’re good for each other!
Young person 3: We just, like, support people with what’s been going on in their week, and stuff, and it’s nice, because we’re like a little family.
Young person 4: We are like a family aren’t we?
The social benefit of groups was also reported by the staff member at the eating disorders message board service (site 5):
[T]he message board is a really good place to start forging links with other people in a very safe and supported way and it helps to build their confidence . . . when they suggest something to somebody [and they] come back and say, ‘that was really good, I did that and it really worked for me’ [they] make very strong bonds with each other. Staff member
Some of the group activities also appeared to help empower the CYP. For example, the self-harm groups (site 1) helped participants develop empathy by encouraging the young people to take it in turns to chair the group. Each group began with each member giving an update on how his or her week had been, and a role of the chair was to ensure that each person contributed. Staff observed that some young people in the group seemed unhappy or annoyed when they would have preferred not to contribute but the chairperson still asked them to share their experiences with the group. The staff member who described this thought that this could help young people to appreciate the difficult task that staff sometimes faced in encouraging young people to engage in ‘talking therapies’, and that sometimes encouraging someone to contribute in a group, even if they seemed not to want to, could help develop empathy and leadership skills in the young person.
Although our data demonstrate that peer support is beneficial, the risk of ‘contagion’, or triggering self-harm or problems with eating, was perceived as a key challenge by staff at the self-harm (site 1) and eating disorders (site 5) sites. Staff at both of these services saw risks in group work and worked actively to manage such risks. Unlike the parenting site (site 3), where parents were ‘buddied’ with another parent and encouraged to support each other between sessions, young people at other sites were discouraged from having contact outside of the service. At the self-harm site, young people were actively discouraged from meeting outside the group and, at the online site, interaction was controlled through moderation of the message board postings. This involved screening and editing posts to ensure that they did not contain contact information.
Some people who had attended the self-harm groups (site 1) and parenting courses (site 3) remembered feeling nervous about attending their first session. As it was the first time they had attended anything of that nature, they were unsure what to expect and were nervous about having to talk about their difficulties in front of other people. They felt that groups were only helpful for people who were at a stage of their illness or recovery where they were ready to attend a group. Our interviewees had all settled into the groups and had positive experiences, but they thought that the group setting would not be suitable for everyone; some people simply would not want or choose to discuss their problems in a group setting. Staff at the self-harm group identified managing dominant personalities as a further challenge that they had to be aware of, in order to make sure that all group members had a chance to participate during each session.
Time and attention
Giving CYP time and attention appeared to be a valued characteristic of the services. At four of the six sites, participants valued simply spending time with children, especially when this involved enjoyable activities. A key principle of Dina School (site 2) and the parenting course (site 3) was giving children positive attention. The Dina School groups allowed for each child to receive more attention than would be possible in a regular class. Parents felt that their children enjoyed being in the group and that the environment was more realistic than the regular classroom for them to learn about talking about their feelings. Parents who attended the parenting course found that setting time aside for their children was helpful, including scheduling time to play with them and also having activities together as a reward for good behaviour, and reported that their children were calmer. At the family support service (site 4), a worker described how during school holidays, instead of having appointments with children at their school, she had collected them from home and brought them to the centre, and had been surprised by how much they enjoyed this:
Often I’ll go and pick the children up and bring them here, which they just think is the best thing in the world . . . it’s not that exciting, but it’s just something different . . . that’s what some of them say. Staff member
Participants of different ages seemed to enjoy positive attention, perhaps away from a school or the clinical or home environment:
Another thing as well that sticks in my mind about the group is when [staff member] actually took us out once into town . . . as a group . . . just to do something nice, instead of being stuck in a small room that’s quite clinical . . . it was good. Young person
At one site, young people recalled their experiences of being inpatients, when some staff would come to talk to them, but often at inappropriate times or not for long enough. At another, family members of younger children appreciated project workers talking to the children themselves.
I think that young people often really have appreciated the fact that someone has taken the time to listen to them and hear their side of the story. Staff member
An older sibling of one of the children at the same service singled out the way that the project worker had helped her brother to understand his behaviours and the emotions attached to them, and what might affect these:
When [child’s name] used to get angry we used to talk to him and try and calm him down . . . but we never used to speak to him about why he got angry . . . I think because [project worker’s name] spoke to him and broke it down into steps that he could understand . . . and then she used to ask him stuff about his friends and his family. Sibling
Although CYP and parents appreciated the time and attention that staff at the sites gave them, staff mentioned that operational constraints sometimes prevented them from providing as much time as they would have liked. The manuals for the Incredible Years services (sites 2 and 3, Dina School and parenting groups) were prescriptive, with themes and associated activities being set out for each session. However, although staff at these sites liked the fact that all the materials for the sessions, and also the letters to send home to parents, were provided (as this made the course easy to deliver), they felt that there was too great a volume of material, and that they had often had to leave out certain aspects in order to complete the sessions on time.
Sometimes it was hard to keep their attention, because we’ve got a programme to deliver and it’s quite a lot to fit into those 2 hours, so sometimes [we] would look at it before and think we’re never going to fit all that in so we’d think, right, we won’t do that activity today, we’ll do that next week and try to fit in an activity where they’d be moving a bit more and try to adapt it a little bit. Staff member
Both CYP and parent participants at several sites mentioned that they would have preferred more sessions or time with the service – a statement also echoed by staff at some sites – but financial constraints prevented this from occurring. In particular, staff at one of the voluntary sector sites outlined how a scheduled 15-week programme had to be reduced to 12 weeks because of financial and resource restraints.
Now we have this 12-week programme and it used to be a bit more like 15 weeks and we used to be able to be a bit more flexible with what each different family needed . . . I feel I used to do a lot more . . . therapeutic work with the young people and creative work, and some of that has had to be cut because we’re having to be a bit more focused on where we need to get to, which is a bit of a shame . . . I used to do a lot more kind of crafty things . . . than I feel that I’ve got the time to really do now. Staff member
- Summary of the case study findings
This chapter has presented the findings derived from 52 interviews with children, young people, parents and staff, some documentary evidence and over 500 message board postings at six case study sites.
The aim of this stage of the project was to investigate the acceptability of mental health self-care support services for CYP and the interface between mental health self-care support providers, the NHS and other service providers in the statutory, private and voluntary sectors.
A common feature across all the case study sites was the perceived accessibility of the services provided. The self-care support services appeared to offer convenient locations and appointment times, maintained engagement with between-session support, and were staffed by people who were caring and compassionate. Given that self-care support necessarily requires an agent – a professional or lay person to provide that support – it was reassuring to witness passionate, motivated, welcoming, non-judgemental and child-centred staff at all six sites. Where barriers were mentioned, they tended to be discussed in the context of other, sometimes competing, services (including standard NHS and local authority services) rather than with reference to the services at the six sites. These barriers could be seen as criticisms of the other sites and were broadly related to inflexibility: applying (stigmatising) diagnoses and labels, rather than seeing the child or young person as a person needing help and support; being dismissive of, or failing to appreciate, the concerns that CYP and their families might have about having a ‘mental health problem’ or accessing services; adhering rigidly to manualised interventions without questioning the readiness of CYP and their families to self-care or the intervention’s suitability to the CYP; and affording them little choice in their (self-)care.
Taking all of the participants’ perspectives – CYP, parents and staff – into account, we can speculate on some of the key elements of effective mental health self-care support for CYP. From the case study data it seems that, in addition to flexibility, effective mental health self-care support services for CYP seem to be built on straightforward access; positive staff and organisational attributes that are non-judgemental and welcoming; the provision of time and attention; the chance to learn and practise skills relevant to self-care; and systems of peer support which include opportunities to share experiences and practical tips.
If there is an overall constraint, it is regarding the interface with other services. The case study sites cut across the NHS, other statutory providers and the voluntary sector, yet there was no clear pattern of how well these providers worked together, if at all. In the two Incredible Years sites, there was a seamless integration of the health, social care and education sectors; yet in another site (the family support group), even though there was ‘nominal’ integration between health, social care and education, the service preferred to see itself as a ‘niche’ not quite fitting into any of these domains. In the other sites, there was either no visible integration or somewhat erratic integration or, as in the case of one site, an almost defiant refusal to integrate demonstrated by the setting up of an alternative, rather than complementary, service. Where the interface between the sectors worked best was in relation to referral: though only a few services had extremely well-integrated referral pathways, all had some degree of interface, even if it was as simple as merely signposting into, or out of, the self-care support service, or using networks among the sectors to promote self-referral to the service.
Included under terms of UK Non-commercial Government License .
- Cite this Page Pryjmachuk S, Elvey R, Kirk S, et al. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Southampton (UK): NIHR Journals Library; 2014 Jun. (Health Services and Delivery Research, No. 2.18.) Chapter 5, The case study.
- PDF version of this title (3.8M)
In this Page
Other titles in this collection.
- Health Services and Delivery Research
Recent Activity
- The case study - Developing a model of mental health self-care support for child... The case study - Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their closest friends. In order to break the stigma that surrounds mental health struggles, we're looking to share your ...
Sarah's case study highlights several important lessons about depression and its treatment: 1. Early intervention is crucial: Sarah's initial reluctance to seek help led to a prolongation of her symptoms. Recognizing and addressing mental health concerns early can prevent the condition from worsening. 2.
Clinical Case Studies (CCS), peer-reviewed & published bi-monthly electronic only, is the only journal devoted entirely to innovative psychotherapy case studies & presents cases involving individual, couples, & family therapy.The easy-to-follow case presentation format allows you to learn how interesting & challenging cases were assessed & conceptualized, & how treatment followed such ...
Driving up quality in mental health care. Mental health care across the NHS in England is changing to improve the experiences of the people who use them. In many areas, a transformation is already under way, offering people better and earlier access as well as more personalised care, whilst building partnerships which reach beyond the NHS to ...
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
The 33-page case study, Mental Health Crisis Support Rooted in Community and Human Rights, presents a viable, replicable framework for a holistic approach to mental health crisis response that ...
The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med Public Health Prep 2012;6:67-71. Crossref
Mental health. Children's mental health case studies. Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and ...
Among the various models of integrated mental health care, the Collaborative Care model (CoCM) ... Women's health: perinatal depression as a case study in the application of CoCM. During the childbearing years, many women receive primary care services through an OBGYN provider. These services include routine monitoring of labs, health ...
This collection of case studies in the ethics of mental health research responds to that gap. This collection comprises six case studies written by contributors from around the world (Table 1). Each describes a mental health research study that raised difficult ethical issues, provides background and analysis of those issues, and draws ...
National Institute of Mental Health (NIMH): Anxiety disorders; Case study 3 summary. In this case study, Lucy's symptoms of mental illness emerge in her teenage years. Lucy describes periods of intense mood, both elevated and depressed, as well as potential anxiety-related responses. It is not until she develops a therapeutic relationship ...
NCMHCE Sample Case Study. You are a licensed mental health counselor working in a community agency. Your client self-referred for services because "my mother won't stop bugging me for staying in bed all day. I can't help it. I am in a rut and cannot find a way out.".
This case study offers important implications regarding the importance of trauma-informed care in the field of mental health. Discover the world's research 25+ million members
Case Studies in Infant Mental Health: Risk, Resiliency, and Relationships Joan J. Shirilla & Deborah J. Weatherston, Editors Washington, D.C. Published by: ZERO TO THREE 2000 M Street NW, Suite 200 Washington, DC 20036-3307 (202) 638-1144 Toll-free for orders: (800) 899-4301
Positive and supportive workplace practices can boost employee mental health, company morale, and your bottom line. Even with foundational steps in place, psychological science can provide answers to take your organization to the next level. Organizational leaders are well-positioned to influence a positive culture shift and normalize mental ...
Surprisingly, however, there has been negligible formal study of case reports and not infrequently there have been calls to cease publishing them . In mental health, case reports may focus on the consumer's journey or life trajectory, providing the clinician with an opportunity to reflect and strengthen their practice. Sharing case reports and ...
In the latest 'Community Case Studies' blog from PLOS Mental Health, we speak to Dr. Anil Fastenau, an author on a recent publication in the journal in which psychosocial interventions in individuals with Leprosy are considered. We spoke to Anil to learn more about his work in this community, and what is needed to support the mental health of those in communities with neglected tropical ...
bject case study design was used in which pre and post-assessment was carried out. Cognitive. behaviour casework intervention was used in dealing with a client with depression. Through an in-depth case study using face to face interview with the client and f. mily members the detailed clinical and social history of the clients was ass.
All subjects Allied Health Cardiology & Cardiovascular Medicine Dentistry Emergency Medicine & Critical Care Endocrinology & Metabolism Environmental Science General Medicine Geriatrics Infectious Diseases Medico-legal Neurology Nursing Nutrition Obstetrics & Gynecology Oncology Orthopaedics & Sports Medicine Otolaryngology Palliative Medicine ...
But while there's far more transparency around mental health than even a few years ago, substantial progress on supporting staff has been slow in some quarters. Research from Business in the Community in September found that of 4,000 employees surveyed, 39% had experienced poor mental health due to their work, while 33% of those with mental ...
Although memories of COVID-19 lockdowns in Danish school children dimmed in detail and emotion from 2020 to 2021, their mental health remained poor, particularly among girls, Aarhus University-led researchers report in Child Development.. The researchers asked 247 students to write about their memories of the first lockdown and their psychological symptoms three times from June 2020 to June ...
Yet, it faces a significant mental health crisis, with suicide rates 3.7x the national average. Addressing this issue is crucial for sustainable development, as workers endure pressures like tight schedules and financial instability, often leading to a reluctance to discuss mental health.
Objective: Suicide remains an urgent public health crisis. Although some sociodemographic characteristics are associated with greater suicide risk in the general population, it is unclear whether individuals utilizing health care in the United States have similar suicide incidence patterns. The authors examined whether race-ethnicity is associated with suicide death among patients seeking ...
Fourteen studies investigated age in association with mental health service use. Nine studies concluded that mental health service use was lower among young and old adult groups, with middle-aged persons with a mental disorder being most likely to access treatment from a mental health professional [26, 42, 43, 47, 54, 66, 67, 123, 130].
Mental health issues account for 45 per cent of the disease burden for 10 to 24-year-olds worldwide, but only 2 per cent of health budgets globally are devoted to mental health care.
The study also found a strong link between mental health issues and workplace toxicity: respondents who stated their workplace is toxic were 47% more likely to cite mental health issues.
Playing video games for a couple of hours a day can improve mental health, according to a study on gamers in Japan during the COVID-19 pandemic 1. The research — which was done from December ...
From the case study data it seems that, in addition to flexibility, effective mental health self-care support services for CYP seem to be built on straightforward access; positive staff and organisational attributes that are non-judgemental and welcoming; the provision of time and attention; the chance to learn and practise skills relevant to ...