- Nurses Turnover and Nurses Retention Words: 1148
- A Head Nurse as a Hospital Manager Words: 1180
- Nurse Autonomy in Practice Words: 1515
- The Career of a Registered Nurse Words: 618
- Nurse-Patient Ratios Problem Words: 586
- Addiction Among Nurses: Professional and Personal Experience of Nurses Words: 656
- Mandatory Overtime for Nurses Words: 581
- Forces as Magnetism: Nurses as Teachers Words: 675
- The Effects of Nurse Burnout on Patient Care and Safety Words: 7052
- Workplace Conflict Between Nurses Words: 1214
- Nurse Staffing and Differing Managerial Approaches Words: 978
- Duties of Learning Disability Nurses Words: 1485

Working as a Head Nurse: Personal Experience
Modern medicine is inextricably linked to the constant stress conditions created by high daily patients’ flow, a variety of problems, and the search for an individual approach to each patient. Such a chaotic state can be confusing, as medical personnel does not always understand exactly which tasks are more important at the moment. In order to create a formal structure, there is a senior nurse responsible for delegation, task allocation, and nurse management. This essay discusses my own experiences, impressions, and lessons learned from the head nurse’s work.
Indeed, most of the time, the patient spends with nurses and other nursing staff, and they are the face of the institution through which patients learn about the culture and values of the clinic. Nevertheless, as a leader, the head nurse is responsible for inspiration, management, and distribution. Initially, it is worth noting that the diversity of tasks assigned to the head nurse is daunting. It is a complex and responsible job associated with the management of subordinate employees to achieve maximum efficiency in clinical processes. There may have been moments when I wanted to give up the burden of responsibility, but I am convinced that such crisis conditions, or rather overcoming them, make medical staff more serious professionals.
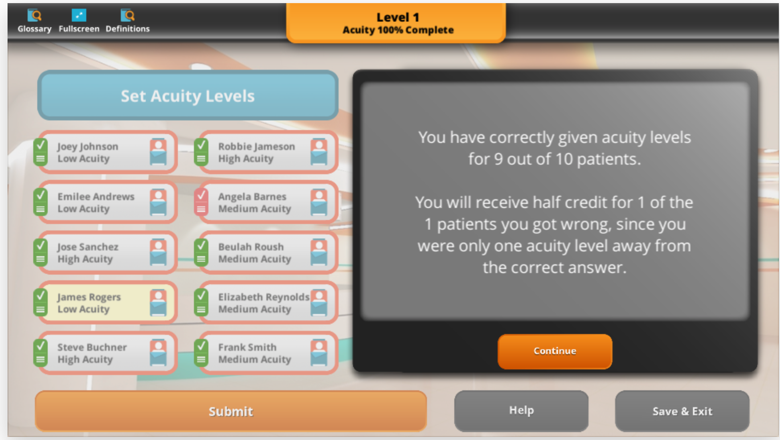
Lessons learned from training and personal experience suggest that it is essential to create a comfortable and stimulating work environment in which the risk of stress complication is minimized. In addition, as a senior nurse, I need to be aware of the responsibility placed on me to lead more effectively: the abundance of patients with a unique clinical picture should not be intimidating but should be used as a tool to perform medical duties. From the simulation, I learned more about how to draw a brief but logical conclusion based on a variety of medical data. With a diagnosis in hand, I need to have a clear understanding of the severity of the damage to health, so that I can then delegate the patient to the nurses or send them to the operating theatre.
As an administrator, the head nurse solves current nursing issues by focusing on today’s problems and ensuring that the work is done efficiently through the available staff capacity. A simulation of a medical organization has demonstrated that it is not enough to manage the nursing staff in the department, but that it is also necessary to schedule and monitor performance. Correct, accurate, and skilled management of the medical team, based on the rational use of each employee, is one of the direct responsibilities of the head nurse. The nurse should reasonably allocate direct duties to subordinates, assigning each to a specific patient according to the severity of the illness. Among other duties, it can be argued that the head nurse has an obligation to prevent and manage conflict, to develop the psychological maturity and high resistance of staff to the stresses of the profession, and to create a particular corporate culture that calls for respect, tolerance, and friendliness.
Through my simulated clinic experience, I realized that not all of my steps could be classified as correct, which was most likely due to a lack of objective assessment of the clinical picture. The leading indicators I paid attention to were primary medical data such as heart rate, pressure, as well as recommendations and diagnosis. However, additional emphasis should also be placed on breathing frequency, oxygen concentration, and, in particular, the blood’s biochemical composition. I am convinced that only by integrating these results can a correct decision be made about the type of treatment and the allocation of nursing responsibilities. If I were able to do the simulation again, I would definitely evaluate each patient more carefully and try not to spend as much time as I do now.
This experience has clearly shown me not only my strongest points as a head nurse but also moments in which I have to work extra. It was a useful practice: despite its virtuality, it helped me to get an initial idea of the complexity of organizing effective work in a medical institution. When more than a dozen patients are asked every day for medical help, the head nurse must do everything possible to demonstrate the clinic’s quality and high reliability.
In terms of more specific lessons I have learned from virtual practice, it is worth mentioning that I have rethought the definition of some diseases. In particular, if a cursory analysis of anamnesis highlights complex conditions such as appendicitis or brain injury, it does not mean that the patient’s condition is critical. It has become more apparent to me what measures need to be taken by the doctor and nurse for specific diagnoses and their urgency. While some diagnoses require urgent care, others can be completed within 16-18 hours or more.
In conclusion, I would like to clarify that the head nurse’s work is multifaceted and challenging. The nurse should act as a manager, psychologist, and teacher for subordinate staff in order to create an environment in which internal clinical processes are addressed quickly, correctly, and effectively. In this course, I had the opportunity to go through a virtual simulation of the head nurse’s clinical work, which showed me the importance of making objective decisions based on a comprehensive view of the patient’s medical data. In addition, in the course of the assignment, I found that it is not enough to find keywords in the anamnesis to conclude the severity of the diagnosis, but it is necessary to back up the arguments with facts.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, February 25). Working as a Head Nurse: Personal Experience. https://studycorgi.com/working-as-a-head-nurse-personal-experience/
"Working as a Head Nurse: Personal Experience." StudyCorgi , 25 Feb. 2022, studycorgi.com/working-as-a-head-nurse-personal-experience/.
StudyCorgi . (2022) 'Working as a Head Nurse: Personal Experience'. 25 February.
1. StudyCorgi . "Working as a Head Nurse: Personal Experience." February 25, 2022. https://studycorgi.com/working-as-a-head-nurse-personal-experience/.
Bibliography
StudyCorgi . "Working as a Head Nurse: Personal Experience." February 25, 2022. https://studycorgi.com/working-as-a-head-nurse-personal-experience/.
StudyCorgi . 2022. "Working as a Head Nurse: Personal Experience." February 25, 2022. https://studycorgi.com/working-as-a-head-nurse-personal-experience/.
This paper, “Working as a Head Nurse: Personal Experience”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: February 25, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
- Search this journal
- Search all journals
- View access options
- View profile
- Create profile
Add email alerts
You are adding the following journal to your email alerts
| New content | |
|---|---|
| SAGE Open Nursing |
The Impact of Transformational Leadership Style on Nurses’ Job Satisfaction: An Integrative Review
Introduction, research question, implications for practice, acknowledgements, declaration of conflicting interests, data availability statement, supplementary material, cite article, share options, information, rights and permissions, metrics and citations, figures and tables, search methods, inclusion/exclusion criteria, inclusion criteria, exclusion criteria, selection of studies.

Data Extraction, Analysis, and Synthesis
Quality assessment, characteristics of the studies.
| Author (year), Country | Aim | Design, participants (sample size), setting | Variable measurement | Main outcomes | Main findings |
|---|---|---|---|---|---|
| ( ), Portugal | To assess the correlation between transformational leadership and the level of satisfaction experienced by nurses within their teams. | Cross-sectional, nurses ( = 95), multiple health care settings | The Global Transformational Leadership Scale and the Group Satisfaction Scale | Job satisfaction | There was a significant correlation ( = .740, = .000) indicating a strong positive relationship between transformational leadership (GTL) and nurses’ satisfaction with their teams (GSS). The presence of more transformational leadership behaviors was directly linked to higher levels of team satisfaction among nurses. |
| ( ), Turkey | To examine how nurse managers and staff nurses perceive the transformational leadership style of nurse managers and assess the impact of this leadership style on the organizational commitment and job satisfaction of staff nurses. | Cross-sectional, 153 nurses (17 nurse managers and 136 staff nurses), 1 University hospital | The LPI: Self/observer (LPI-self/observer), the Organizational Commitment Scale and the Job Satisfaction Scale | Organizational commitment and job satisfaction | The transformational leadership practices implemented by nurse managers contributed to 9% of the overall organizational commitment ( = .299, = .09, < .001) and 24% of the overall job satisfaction among staff nurses ( = .488, = .24, < .001). |
| ( ), Jordan | The aim was to explore the correlation between transformational leadership, job satisfaction, and organizational commitment among nurses | Cross-sectional, registered nurses ( = 253), 2 governmental hospitals | The Global Transformational Leadership scale, job satisfaction survey, and Organizational Commitment Scale | Job satisfaction and organizational commitment | A significant and positive correlation was observed between transformational leadership and job satisfaction ( = .297, = .000). Additionally, a positive relationship was found between TL and organizational commitment ( = .200, = .001). |
| ( & Joniaková, 2021), Slovakia | To examine the connection between communication skills and the transformation style of first-line nurse managers management with the job satisfaction of nurses and to verify the influence of three moderators on the strength of this relationship | Descriptive cross-sectional, first line nurse managers ( = 132), 5 university hospitals | The Multifactor Leadership Questionnaire-5× Short Rater, 5-point Likert scale | Job satisfaction | The findings point to the strong direct effects of communication skills and the transformational leadership style of first-line nurse managers on nurses’ job satisfaction (ß = 1.12, < .05). |
| ( et al., 2020), Philippines | To examine the influence of toxic and transformational leadership practices on nurses’ job satisfaction, psychological distress, absenteeism, and intent to leave the organization or the nursing profession | Cross-sectional, registered nurses ( = 770), 15 hospitals | The 7-item Global Transformational Leadership Scale, the six-item JSI. | Nurses’ job satisfaction, psychological distress, absenteeism and intent to leave the organization or the nursing profession | Transformational leadership predicted job satisfaction ( = .37, < .001) and intent to leave the profession ( = −.08, < .05). |
| ( ), Saudi Arabia | To determine the relationship between the leadership styles of nurse managers and the job satisfaction of staff nurses in hospital settings | Descriptive correlational design, nurses ( = 184), 5 hospitals | The Multifactor Leadership Questionnaire-5× Short Rater, 7-point Likert scale | Job satisfaction of staff nurses | The staff nurses’ level of job satisfaction slightly increased ( = .258, = .000) while nurse managers demonstrated transformational leadership. |
| ( ), Pakistan | To examine the relationships between transformational leadership, structural empowerment, job satisfaction, nurse-assessed adverse patient outcomes, and the quality of care. | Cross-sectional, registered nurse ( = 600), 17 government hospitals | The 7-item Global Transformational Leadership Scale | Quality of care and patient satisfaction | Transformational leadership is a crucial to improve quality of care, nurses’ job satisfaction ( = .43, < .01) and minimize adverse patient outcomes |
| ( ), Canada | To investigate the effects of nurse managers’ transformational leadership behaviors on job satisfaction and patient safety outcomes | Cross-sectional, acute care nurses ( = 378), acute care hospitals across Ontario | The Multifactor Leadership Questionnaire-5× Short Rater, the GJS questionnaire. | Job satisfaction and patient safety outcomes | Transformational leadership had a strong positive influence on workplace empowerment (β = 0.77, < .001), which in turn increased nurses’ job satisfaction (β = 0.86, < .001) and decreased the frequency of adverse patient outcomes (β = −0.35, < .05). |
| ( ), Italy | To describe staff nurses’ perceptions related to the leadership styles adopted by their nurse managers, identify which leadership style ensured job satisfaction in staff nurses and describe which nurse managers’ behavior should change. | Mixed method, staff nurse ( = 87 and 3 focus group), 3 acute hospitals | The Multifactor Leadership Questionnaire-5× Short Rater | Job satisfaction | A positive correlation emerged between staff nurses’ satisfaction and all dimensions of transformational leadership style. |
| ( ), Jordan | To explore how the leadership styles of nurse leaders affect job satisfaction among working nurses. | Cross -sectional, nurses ( = 200), 3 public hospitals, 3 private hospitals | The Multifactor Leadership Questionnaire-5× Short Rater, 3-point Likert scale | Nurses’ job satisfaction | The increased development of transformational leadership behaviors increased nurses’ job satisfaction ( = .37, < .001). |
| ( ), Saudi Arabia | To evaluate the effect of transformational and transactional leadership styles of head nurses on the job satisfaction of staff nurses in critical care units of a tertiary care hospital. | Cross-sectional, licensed nurses ( = 89), Critical care unit | The Multifactor Leadership Questionnaire-5× Short Rater, 6-point scale | Staff nurses’ job satisfaction. | Nurses working under leaders with a transformational leadership style demonstrated higher job satisfaction (R = .176, < .001. |
| ( ), USA | To examine the effect of transformational leadership on early career nurses’ intent to stay, job satisfaction and organizational commitment. | Cross-sectional, registered nurse ( = 1037), 51 metropolitan statistical areas and 9 rural areas in 34 US States and the District of Columbia | The Multifactor Leadership Questionnaire-5× Short Rater, 5-point Likert scale | Intent to stay, job satisfaction and organizational commitment | Transformational leadership did not show a significant correlation with nurses’ intent to stay at job and job satisfaction, but significantly associated with organizational commitment |
| ( ) Malaysia | To investigate the causal relationships among perceived transformational leadership, empowerment, and job satisfaction among nurses and medical assistants in | Cross-sectional, nursing staff ( = 200), 1 public and 1 private hospitals | The Multifactor Leadership Questionnaire-5× Short Rater, 5-point Likert scale | Job satisfaction of medical assistants and nurses | Transformational leadership positively influences job satisfaction (R = .46, < .01) among nurse staffs. |
| ( et al., 2014), USA | To describe the relationship between pediatric RN-reported ratings of RN leadership characteristics (transformational and transactional leadership) and RN job satisfaction. The | Retrospective cross-sectional, pediatric RNs ( = 935), 1 hospital | The Multifactor Leadership Questionnaire-5× Short Rater, Job Satisfaction Scale | RN-job satisfaction | Transformational leadership style positively impacted RN's job satisfaction (β = 0.069, = .002). |
| ( ), Ethiopia | To investigate the relationship between leadership style of nurse managers and nurses’ job satisfaction | Nonexperimental correlation design (cross-sectional), nurses ( = 176), 1 University hospital | The Multifactor Leadership Questionnaire-5× Short Rater | Job satisfaction | All the 5 dimensions of transformational leadership were found to be positively associated with both intrinsic and extrinsic job satisfactions. Intrinsic: Individual consideration (β = 0.35, < .01), inspirational stimulation (β = 0.31, < .01), intellectual Motive (β = 0.49, < .01), idealized influence (attribute) (β = 0.29, < .01), idealized influence (behavior) (β = 0.32, < .01) and inspirational motive (β = 0.49, < .01) Extrinsic: Idealized influence (attribute (β = 0.21, < .05), idealized influence (behavior) (β = 0.19, < .05), intellectual stimulation (β = 0.42, < .05), inspirational motivation (β = 0.19, < .05) and individual consideration (β = 0.17, < .05)" |
| ( ), China | To describe the relationship between the transformational leadership of nurse managers and job satisfaction among clinical Registered Nurses at a tertiary care hospital | Correlational cross -sectional, clinical Registered Nurses ( = 250), 1 tertiary hospital | The Chinese version of the Leadership Practice Inventory observer, NJSS | Job satisfaction | A positive correlation was recorded between the transformational leadership of nurse managers and job satisfaction ( = .556, < .001). |
| ( & Alghamdi, 2012), Saudi Arabia | To examine the impact of leadership styles of nurse managers on Saudi nurses’ job satisfaction and their intent to stay at work. | Descriptive correlational design (cross-sectional), nurses ( = 302), 6 public hospitals | The MLQ-5×, Job Satisfaction Survey | Nurses’ job satisfaction | A significant moderate positive correlation was observed between the transformational leadership style and nurses’ job satisfaction ( = .45, < .001) Those who were more satisfied with their jobs intended to stay at work. |
Quality Appraisal of the Review
The impact of transformational leadership on nurses` satisfaction, limitations.
Please find the following supplemental material available below.
For Open Access articles published under a Creative Commons License , all supplemental material carries the same license as the article it is associated with.
For non-Open Access articles published, all supplemental material carries a non-exclusive license, and permission requests for re-use of supplemental material or any part of supplemental material shall be sent directly to the copyright owner as specified in the copyright notice associated with the article.
- sj-docx-1-son-10.1177_23779608231197428.docx
- sj-docx-2-son-10.1177_23779608231197428.docx
Download to reference manager
If you have citation software installed, you can download article citation data to the citation manager of your choice
Share this article
Share with email, share on social media, share access to this article.
Sharing links are not relevant where the article is open access and not available if you do not have a subscription.
For more information view the Sage Journals article sharing page.
Information
Published in.

- satisfaction
Rights and permissions
Affiliations, journals metrics.
This article was published in SAGE Open Nursing .
Article usage *
Total views and downloads: 11772
* Article usage tracking started in December 2016
Articles citing this one
Receive email alerts when this article is cited
Web of Science: 1 view articles Opens in new tab
Crossref: 0
There are no citing articles to show.
Figures & Media
View options, view options, access options.
If you have access to journal content via a personal subscription, university, library, employer or society, select from the options below:
I am signed in as:
I can access personal subscriptions, purchases, paired institutional access and free tools such as favourite journals, email alerts and saved searches.
Login failed. Please check you entered the correct user name and password.
Access personal subscriptions, purchases, paired institutional or society access and free tools such as email alerts and saved searches.
loading institutional access options
Click the button below for the full-text content
Alternatively, view purchase options below:
Access journal content via a DeepDyve subscription or find out more about this option.
Also from Sage
- CQ Library Elevating debate opens in new tab
- Sage Data Uncovering insight opens in new tab
- Sage Business Cases Shaping futures opens in new tab
- Sage Campus Unleashing potential opens in new tab
- Sage Knowledge Multimedia learning resources opens in new tab
- Sage Research Methods Supercharging research opens in new tab
- Sage Video Streaming knowledge opens in new tab
- Technology from Sage Library digital services opens in new tab
e-Publications@Marquette
- < Previous
Home > Dissertations, Theses, and Professional Projects > ESSAYS > 185
Master's Essays (1922 - )
Head nurse: position responsibility.
Genevieve M. Adrian
Date of Award
Degree type.
Master's Essay - Restricted
First Advisor
Louise Schmitt
Second Advisor
Agnes A. Shoemaker
A head nurse is an administrator, a nurse clinician, and a teacher in a specified unit of nursing service, where she is responsible for the planning, coordinating, and rendering of quality nursing care given the patients assigned to her unit. Legally she is responsible, with al the individuals who work with her, to provide quality nursing service. She is expected to know the educational and instructional backgrounds of persons whom she supervises, and be appraised of their competencies so that she can make assignments that are commensurate with the worker's ability and the law.
In the Nursing Service Department of the hospital the organizational paln includes the director of nursing, assistant director of nursing, supervisor, head nurse, staff nurse, and nursing assistants.
"Head Nurse Routine" at St. Luke's Hospital is a job description of the head nurse used to identify the responsibilities and guide the head nurse and as a special tool in orientation of new head nurses.
This study concerns one facet of responsibility taken from the "Head Nurse Routine."
Recommended Citation
Adrian, Genevieve M., "Head Nurse: Position Responsibility" (1966). Master's Essays (1922 - ) . 185. https://epublications.marquette.edu/essays/185
Since March 13, 2023
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Information about e-Pubs@MU
- General FAQ
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Nursing Essay Examples

Nursing Essay Examples That Will Help You Write a Stellar Paper
Published on: May 6, 2023
Last updated on: Jan 29, 2024

Share this article
Many nursing students struggle with writing effective nursing essays, which are an essential part of their education and professional development.
Poor essay writing skills can lead to low grades and an inability to effectively communicate important information.
This blog provides a comprehensive guide to writing nursing essays with examples and tips for effective writing. Whether you are a nursing student or a professional looking to improve your writing skills, this blog has something for you.
By following the tips and examples provided, you can write compelling nursing essays that showcase your dedication to the field.
Let’s get started.
On This Page On This Page -->
What is a Nursing Essay?
A nursing essay is a type of academic writing that aims to explore a particular topic related to nursing. It also presents a clear and concise argument or viewpoint supported by evidence.
Nursing essays can take many forms, including:
- Descriptive essays
- Reflective essays
- Analytical essays
- Persuasive essays
What is the Importance of the Nursing Essay?
Nursing essays are important for several reasons. First, they help nursing students develop critical thinking skills by requiring them to analyze and evaluate information.
Second, they help students develop research skills by requiring them to locate and use credible sources to support their arguments.
Third, nursing essays help students develop communication skills by requiring them to present their ideas clearly and concisely in writing. Finally, nursing essays are important for nursing education because they prepare students for the types of writing.
Paper Due? Why Suffer? That's our Job!
To help students better understand how to write nursing essays, it can be helpful to review examples.
Below are some examples of nursing essays.
Nursing School Essay Examples
College Nursing Essay Examples
Graduate Nursing Essay Examples
Nursing Scholarship Essay Examples
Nursing Essay Conclusion Examples
Nursing Essay Examples of Different Fields
Nursing is a diverse field with many different specialties and areas of focus. As a result, nursing essays can take many different forms and cover a wide range of topics.
Given below are some examples of different types of nursing essays:
Personal Philosophy Of Nursing - Essay Examples
Cal State Fullerton Nursing Essay Examples
Evidence Based Practice Nursing In Medical Field - Essay Examples
Leadership In Nursing And Healthcare Professionals - Essay Examples
Principles Of Professional Practice Of Nursing Professionals And Pharmacists
If you're seeking additional examples of nursing essays, you're in luck!
Below are some more examples that can help you gain a better understanding of nursing essays:
Health Care And Reflective Models For Nursing - Essay Examples
History Of Nursing Essay Examples
Ethical Dilemma In Nurses Work - Essay Examples
Mental Health Nursing Essay Examples
Why I Want To Be A Nurse Essay
Working In A Team And Collaboration In Nursing
How to Write a Nursing Essay
Writing a nursing essay can seem daunting, but with the right approach, it can be a rewarding experience.
Here are the key steps involved in writing a nursing essay:
Understanding the Topic and Question
The first step in writing a nursing essay is to carefully read and understand the topic and question.
This will help you determine what information you need to research and include in your essay. Make sure you understand any key terms or concepts related to the topic. Consider different perspectives or viewpoints that may be relevant.
Researching the Topic
Once you have a clear understanding of the topic and question, it's time to research.
Start by gathering information from credible sources such as academic journals, textbooks, and government websites.
Consider both primary and secondary sources, and make sure to take detailed notes as you read.
Organizing and Outlining the Essay
Once you have completed your research, it's time to organize your ideas and create an outline for your essay.
Start by identifying the main points or arguments you want to make, and then organize them into a logical order that flows well.
Your outline should include an introduction, body paragraphs, and a conclusion.
Writing the Essay
With your outline in place, it's time to start writing your essay. Make sure to follow your outline closely, and use clear and concise language that effectively communicates your ideas.
Use evidence from your research to support your arguments, and cite your sources appropriately.
Editing and Revising the Essay
Once you have completed a first draft of your essay, take some time to edit and revise it. Look for any errors in grammar, spelling, or punctuation, and make sure your essay is well-organized and flows well.
Consider asking a peer or instructor to review your essay and provide feedback.
What To Include In Your Nursing Essay
When writing a nursing essay, there are several key elements that you should include. Here are some important things to keep in mind:
- Introduction
Your introduction should provide a brief overview of the topic and purpose of your essay. It should also include a clear thesis statement that presents your main argument or point of view.
- Background Information
Provide some background information on the topic to help the reader better understand the context of your essay. This can include relevant statistics, historical information, or other contextual details.
- Evidence and Examples
Use evidence and examples from your research to support your arguments and demonstrate your knowledge of the topic. Make sure to cite your sources appropriately and use a variety of sources to strengthen your argument.
- Analysis and Evaluation
Provide analysis and evaluation of the evidence and examples you've presented. This can include discussing strengths and weaknesses, comparing and contrasting different viewpoints, or offering your own perspective on the topic.
Your conclusion should summarize the main points of your essay and restate your thesis statement. It should also offer some final thoughts or suggestions for further research or action.
Nursing Essay Topic Ideas
Choosing a topic for your nursing essay can be challenging, but there are many areas in the field that you can explore. Here are some nursing essay topic ideas to consider:
- The role of technology in nursing practice
- The impact of cultural diversity on healthcare delivery
- Nursing leadership and management in healthcare organizations
- Ethical issues in nursing practice
- The importance of patient-centered care in nursing practice
- The impact of evidence-based practice on nursing care
- The role of nursing in promoting public health
- Nursing education and the importance of lifelong learning
- The impact of nursing shortages on healthcare delivery
- The importance of communication in nursing practice
These are just a few ideas to get you started. You can also explore other topics related to nursing that interest you or align with your academic or professional goals.
Remember to choose a topic that is relevant, interesting, and feasible to research and write about.
Tips for Writing an Effective Nursing Essay
Writing a successful nursing essay requires careful planning, research, and attention to detail. Here are some tips to help you write an effective nursing essay:
- Writing Concisely and Clearly
Nursing essays should be written in clear and concise language, avoiding unnecessary jargon or technical terms. Use simple language and short sentences to help ensure that your ideas are communicated clearly and effectively.
- Stating a Clear Thesis Statement
Your thesis statement should clearly state your main argument and provide a roadmap for the rest of your essay. It should be clear, concise, and located at the end of your introduction.
- Using Proper Citation and Referencing
Citing and referencing your sources is crucial in any academic writing, including nursing essays. Make sure to use proper citation and referencing styles, such as APA or MLA. Include a reference list or bibliography at the end of your essay.
- Seeking Feedback and Revising
Before submitting your nursing essay, seek feedback from peers, professors, or writing tutors. Use their feedback to revise and improve your essay. Make sure that it is well-structured, coherent, and effectively communicates your point of view.
By following these tips, you can write a nursing essay that demonstrates your knowledge and skills in the field.
In conclusion, writing a successful nursing essay requires careful planning, research, and attention to detail.
To showcase your knowledge in the field of nursing, it is important to have a clear understanding of the topic at hand. When writing your nursing essay, be sure to include relevant examples, incorporate current research, and use proper citation and referencing.
And remember , seeking feedback and revising your essay is key to ensuring that it effectively communicates your ideas and arguments.
If you need help with your nursing essay or any other type of academic writing, consider using our AI essay writer .
Our nursing essay writing service can provide personalized support to help you succeed in your academic goals.
So, why wait? Contact us to get college essay writing help today!
Cathy A. (Literature)
For more than five years now, Cathy has been one of our most hardworking authors on the platform. With a Masters degree in mass communication, she knows the ins and outs of professional writing. Clients often leave her glowing reviews for being an amazing writer who takes her work very seriously.
Paper Due? Why Suffer? That’s our Job!
Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.
How to Write a Nursing Essay with a Quick Guide

Ever felt the blank-page panic when assigned a nursing essay? Wondering where to start or if your words will measure up to the weight of your experiences? Fear not, because today, we're here to guide you through this process.
Imagine you're at your favorite coffee spot, armed with a cup of motivation (and maybe a sneaky treat). Got it? Great! Now, let's spill the secrets on how to spin your nursing tales into words that not only get you that A+ but also tug at the heartstrings of anyone reading. We've got your back with nursing essay examples that'll be your inspiration, an outline to keep you on the right path, and more!
What Is a Nursing Essay
Let's start by dissecting the concept. A nursing essay serves as a focused exploration of a specific aspect of nursing, providing an opportunity for students to demonstrate their theoretical knowledge and its practical application in patient care settings.
Picture it as a journey through the challenges and victories of a budding nurse. These essays go beyond the classroom, tackling everything from tricky ethical dilemmas to the impact of healthcare policies on the front lines. It's not just about grades; it's about proving, 'I'm ready for the real deal.'
So, when you read or write a nursing essay, it's not just words on paper. It's like looking into the world of someone who's about to start their nursing career – someone who's really thought about the ins and outs of being a nurse. And before you kick off your nursing career, don't shy away from asking - write my essay for me - we're ready to land a professional helping hand.
How to Start a Nursing Essay
When you start writing a nursing essay, it is like gearing up for a crucial mission. Here's your quick guide from our nursing essay writing service :

Choosing Your Topic: Select a topic that sparks your interest and relates to real-world nursing challenges. Consider areas like patient care, ethical dilemmas, or the impact of technology on healthcare.
Outline Your Route : Plan your essay's journey. Create a roadmap with key points you want to cover. This keeps you on track and your essay on point.
Craft a Strong Thesis: Assuming you already know how to write a hook , kick off your writing with a surprising fact, a thought-provoking quote, or a brief anecdote. Then, state your main argument or perspective in one sentence. This thesis will serve as the compass for your essay, guiding both you and your reader through the rest of your writing.
How to Structure a Nursing Essay
Every great essay is like a well-orchestrated performance – it needs a script, a narrative that flows seamlessly, capturing the audience's attention from start to finish. In our case, this script takes the form of a well-organized structure. Let's delve into the elements that teach you how to write a nursing essay, from a mere collection of words to a compelling journey of insights.

Nursing Essay Introduction
Begin your nursing essay with a spark. Knowing how to write essay introduction effectively means sharing a real-life scenario or a striking fact related to your topic. For instance, if exploring patient care, narrate a personal experience that made a lasting impression. Then, crisply state your thesis – a clear roadmap indicating the direction your essay will take. Think of it as a teaser that leaves the reader eager to explore the insights you're about to unfold.
In the main body, dive into the heart of your essay. Each paragraph should explore a specific aspect of your topic. Back your thoughts with examples – maybe a scenario from your clinical experience, a relevant case study, or findings from credible sources. Imagine it as a puzzle coming together; each paragraph adds a piece, forming a complete picture. Keep it focused and let each idea flow naturally into the next.
Nursing Essay Conclusion
As writing a nursing essay nears the end, resist the urge to introduce new elements. Summarize your main points concisely. Remind the reader of the real-world significance of your thesis – why it matters in the broader context of nursing. Conclude with a thought-provoking statement or a call to reflection, leaving your reader with a lasting impression. It's like the final scene of a movie that leaves you thinking long after the credits roll.
Nursing Essay Outline
Before diving into the essay, craft a roadmap – your outline. This isn't a rigid skeleton but a flexible guide that ensures your ideas flow logically. Consider the following template from our research paper writing service :
Introduction
- Opening Hook: Share a brief, impactful patient care scenario.
- Relevance Statement: Explain why the chosen topic is crucial in nursing.
- Thesis: Clearly state the main argument or perspective.
Patient-Centered Care:
- Definition: Clarify what patient-centered care means in nursing.
- Personal Experience: Share a relevant encounter from clinical practice.
- Evidence: Integrate findings from reputable nursing literature.
Ethical Dilemmas in Nursing Practice
- Scenario Presentation: Describe a specific ethical challenge faced by nurses.
- Decision-Making Process: Outline steps taken to address the dilemma.
- Ethical Frameworks: Discuss any ethical theories guiding the decision.
Impact of Technology on Nursing
- Current Trends: Highlight technological advancements in nursing.
- Case Study: Share an example of technology enhancing patient care.
- Challenges and Benefits: Discuss the pros and cons of technology in nursing.
- Summary of Key Points: Recap the main ideas from each section.
- Real-world Implications: Emphasize the practical significance in nursing practice.
- Closing Thought: End with a reflective statement or call to action.
A+ in Nursing Essays Await You!
Ready to excel? Let us guide you. Click now for professional nursing essay writing assistance.
Nursing Essay Examples
Here are the nursing Essay Examples for you to read.
Writing a Nursing Essay: Essential Tips
When it comes to crafting a stellar nursing essay, a few key strategies can elevate your work from ordinary to exceptional. Here are some valuable tips from our medical school personal statement writer :

Connect with Personal Experiences:
- Approach: Weave personal encounters seamlessly into your narrative.
- Reasoning: This not only adds authenticity to your essay but also serves as a powerful testament to your firsthand understanding of the challenges and triumphs in the nursing field.
Emphasize Critical Thinking:
- Approach: Go beyond describing situations; delve into their analysis.
- Reasoning: Nursing essays are the perfect platform to showcase your critical thinking skills – an essential attribute in making informed decisions in real-world healthcare scenarios.
Incorporate Patient Perspectives:
- Approach: Integrate patient stories or feedback into your discussion.
- Reasoning: By bringing in the human element, you demonstrate empathy and an understanding of the patient's experience, a core aspect of nursing care.
Integrate Evidence-Based Practice:
- Approach: Support your arguments with the latest evidence-based literature.
- Reasoning: Highlighting your commitment to staying informed and applying current research underscores your dedication to evidence-based practice – a cornerstone in modern nursing.
Address Ethical Considerations:
- Approach: Explicitly discuss the ethical dimensions of your topic.
- Reasoning: Nursing essays provide a platform to delve into the ethical complexities inherent in healthcare, showcasing your ability to navigate and analyze these challenges.
Balance Theory and Practice:
- Approach: Connect theoretical concepts to real-world applications.
- Reasoning: By bridging the gap between theory and practice, you illustrate your capacity to apply academic knowledge effectively in the dynamic realm of nursing.
Highlight Interdisciplinary Collaboration:
- Approach: Discuss collaborative efforts with other healthcare professionals.
- Reasoning: Acknowledging the interdisciplinary nature of healthcare underscores your understanding of the importance of teamwork – a vital aspect of successful nursing practice.
Reflect on Lessons Learned:
- Approach: Conclude with a thoughtful reflection on personal growth or lessons from your exploration.
- Reasoning: This not only provides a satisfying conclusion but also demonstrates your self-awareness and commitment to continuous improvement as a nursing professional.
As we wrap up, think of your essay as a story about your journey into nursing. It's not just about getting a grade; it's a way to share what you've been through and why you want to be a nurse.
Imagine the person reading it – maybe a teacher, a future coworker, or someone starting their nursing journey. They're trying to understand your passion and why you care about nursing.
So, when you write, remember it's more than just an assignment. It's your chance to show why nursing matters to you. And if you ever need help – there's always support from our essay writer online .
Ready to Excel in Your Nursing School Essay?
Order now and experience the expertise of our professional writers!
How to Write a Nursing Essay?
How can a nursing essay effectively address ethical considerations, what are some examples of evidence-based practices in nursing essays.

Daniel Parker
is a seasoned educational writer focusing on scholarship guidance, research papers, and various forms of academic essays including reflective and narrative essays. His expertise also extends to detailed case studies. A scholar with a background in English Literature and Education, Daniel’s work on EssayPro blog aims to support students in achieving academic excellence and securing scholarships. His hobbies include reading classic literature and participating in academic forums.

is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.60; Jan-Dec 2023
- PMC10265372
Impact of Nurse Leaders Behaviors on Nursing Staff Performance: A Systematic Review of Literature
Nourah alsadaan.
1 Jouf University, Sakaka, Saudi Arabia
Basma Salameh
2 Arab American University, Jenin, Palestine
Fadia Ahmed Abdelkader Elsaid Reshia
3 Mansoura University, Mansoura, Egypt
Reem F. Alruwaili
Majed alruwaili, shaimaa ahmed awad ali, abeer nuwayfi alruwaili, gehan refat hefnawy, maha suwailem s. alshammari, afrah ghazi rumayh alrumayh, alya olayan alruwaili, linda katherine jones.
4 Charles Sturt University, Wagga Wagga, NSW, Australia
Nursing leadership is critical in facilitating and improving nurse performance, which is essential for providing quality care and ensuring patient safety. The aim of this study is to explore the relationship between nursing leadership and nurse performance by understanding the leadership behaviors and factors that motivate nurses to perform well. To study the factors that nurses believe motivate them to perform better, a systematic review was undertaken, correlating these factors to leadership behaviors/styles. The PRISMA guidelines were followed to identify relevant articles. After applying the selection criteria, 11 articles were included in the final analysis. Overall, 51 elements that influence nurses’ motivation to perform better were found and categorized into 6 categories, including autonomy, competencies, relatedness, individual nursing characteristics, relationships and support, and leadership styles/practices. It has been discovered that both direct and indirect nursing leadership behaviors affect nurses’ performance. A better understanding of the factors that motivate nurses to perform well and facilitating them in the work environment through leadership behaviors/styles can improve nurses’ performance. There is a need to increase research on nurse leadership and nurses’ performance in the current innovative and technologically integrated work environment to identify new factors of influence.
- What do we already know about this topic?
- Effective leadership in nursing can have a positive impact on nurse performance, job satisfaction, and patient outcomes.
- How does your research contribute to the field?
- It can provide new insights and understanding of how different leadership styles and practices impact nurse performance and patient outcomes
- What are your research’s implications toward theory, practice, or policy?
- To identify effective leadership practices that promote positive work environments, better nurse performance, and ultimately better patient outcomes, thus leading to improved patient contentment, safety, and care quality.
Introduction
Nurses are essential resources in hospitals as they spend more time with patients than any other healthcare personnel. Therefore, they play a significant role in ensuring quality care and patients’ safety by improving their performance. Despite accounting for 50% of the global healthcare workforce, 1 there is a severe shortage of nursing personnel in almost all countries. Developed countries such as the USA need an additional 275 000 nurses from 2020 to 2030. 2 According to the International Council of Nurses, there is a need for 13 million nurses globally to fill the shortage gap in the future. 3
The shortage of nurses has resulted in an increasing workload for existing nurses, significantly affecting their work life and performance, which can have a direct impact on the quality of care delivered. 4 Nursing performance is influenced by cognitive, physical, and organizational factors. 5 Various factors such as high workloads, lack of technological support, 6 skills and competencies (eg, problem-solving ability, nursing informatics competencies), 7 communication skills and confidence, 8 commitment, 9 quality of work life, 10 job stress, 11 and motivation 12 can significantly influence nursing performance. It is interesting to observe that most of these factors are a part of leadership management, focusing on providing training and support and addressing the issues affecting nurses.
Quality leadership was identified to be one of the major factors for promoting behaviors among the nurses for exhibiting greater responsibility and physical activity. 13 Similarly, workplace incivility from supervisors was identified to be negatively related to nursing performance. 14 Nursing leadership behaviors play a crucial role in shaping nursing performance, thereby achieving the organizational goals of ensuring the delivery of quality care and achieving better patient outcomes. 15 - 17 Considering the nursing leadership theories, transformational and transactional leadership styles 18 , 19 and their impact on nurses’ satisfaction, burnout, and resilience have received lot of attention. 17 , 18 , 20 However, most of the studies investigated the leadership styles influence on the factors affecting the nursing performance, but very few studies have focused on the leadership factors influencing the nurses’ motivation to perform well. An attempt in this aspect was made in a study 21 through the systematic review, but it only included studies till 2006. However, major changes have been observed in the factors influencing nursing performance in the past decade. The use of the internet and telecommunication technologies have significantly changed the quality of work of nurses, and led to the new forms of remote practices such as telenursing. 22 Furthermore, advanced innovative technologies such as artificial intelligence, intelligent systems such as IoTs 23 , 24 have significantly contributed to the nursing practice. 25 , 26 Additionally, due to the sudden surge of patients caused by the recent Covid-19 pandemic, nurses have experienced heightened levels of burnout, 27 which has significantly affected nurses work-life balance and their performance. 28 , 29 Furthermore, the COVID-19 pandemic has rendered the nursing shortage a critical issue on a global scale, according to the ICN study report 2023. 30 There are issues including understaffing and low job satisfaction, as well as an aging nursing workforce and a lack of young individuals entering the profession. The report highlighted that nurses’ shortage has grown significantly from 30.6 million in 2019 after the pandemic began. Furthermore, it identified that key research from surveys and reviews in the past 3 years, after the emergence of Covid-19 pandemic, there is a significant increase in nurses burn-out. This has resulted in burn-out nurses either leaving their employment or reducing their work hours, which has led to additional burden of work, increasing levels of stress among the resilient working nurses. 30 Therefore, significant changes in the factors that influence nurses’ motivation to perform well might have occurred. Considering these developments, it is necessary to extend the review conducted in Brady Germain and Cummings, 21 to identify the new developments in the research arena. For that, the purpose of this study is to conduct a systematic review for examining the factors related to nurses’ leadership and nurses’ performance. To achieve this objective, the following research questions are formulated.
- RQ1: What factors do nurses think affect their drive to excel in their work? The ambition and aptitude of the nurses to achieve their companies’ objectives of high-quality care and patient safety serve as the benchmarks for performance in this context.
- RQ2: Which leadership traits are associated with strong nurse performance? In this context, behaviors are described as the traits or tactics used by leaders to control nurses’ performance in order to accomplish organizational objectives, such as patient safety and high-quality care.
Materials and Methods
The protocol for this study is registered with PROSPERO (registration number: CRD42023387324), the registration date 15/01/2023.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 33 was used for conducting the systematic review of recent literature and reporting the findings relating to nursing leadership attributes and nursing performance.
Search Methods
Various databases, including CINAHL, Cochrane, EMBASE, HealthSTAR, Medline, and PsychINFO, were utilized to search for relevant studies. The search terms “nursing performance,” “nurse motivation,” “nursing leadership,” and “nursing leadership behaviors” were combined using Boolean operators “AND” and “OR.” To improve search sensitivity, keywords from the identified studies were also used in the search process. Only studies published in English were considered. Additionally, studies published within the last 20 years were included to ensure the search was current and covered new literature since the previous study by 23. Therefore, those studies before 2003 are excluded. Inclusion and exclusion criteria, as presented in Table 1 , were applied for selecting studies. Figure 1 provides a detailed overview of the search strategy used to select studies.
Inclusion and Exclusion Criteria.
| Inclusion | Exclusion |
|---|---|
| Experimental and quasi experimental studies that focus on nursing leadership and nursing performance | Opinion based articles; Studies that include nursing students as sample |
| Qualitative studies and reviews on the subject with a rigorous systematic methodology | Studies that included nurses who work in outpatient and home settings |

PRISMA flow diagram.
Quality Appraisal
Two methods were used to rate the methodological quality of the chosen studies. The PRISMA 31 methodological quality criterion, which contains 27 elements, was used to systematic reviews. TREND 32 was used to evaluate quasi-experimental studies. TREND 32 comprises 22 criteria. The last criterion received a “yes,” a “no,” or a “unclear” rating. The “yes” items were added up to create a total score for each study, which ranged from zero to the total number of items that were examined. Studies with low methodological quality were deemed to be omitted from the review if they received a score of less than or equal to 50% on the evaluated items. Studies were deemed to be of medium or high quality and included in the review if they scored more than 50% on the analyzed items.
Data Extraction
Quantitative studies were the source of data, which encompassed details such as the author, publication year, research aim, sample size, methodology employed, independent and dependent variables, measurement criteria, reliability and validity of the measures, analytical techniques, and findings. The number of studies examined and the key conclusions were retrieved for systematic reviews.
Search Outcomes
Initially, 1632 articles were identified from different electronic databases, and 16 articles were identified through manual searching of journals, resulting in a total of 1648 articles. After removing 587 duplicates, 1061 articles were screened for titles and abstracts. Out of these, 984 articles were excluded based on title and abstract assessment, and 77 articles were selected for full-text reviews. After reviewing the full-text articles, 64 articles did not meet the inclusion criteria and were excluded. Finally, 13 articles were deemed eligible for quality assessment. Two articles did not meet quality criteria and were excluded resulting in 11 articles that are included in this review (See Figure 1 ).
Study Characteristics
Table 2 exhibits the attributes of the studies that were incorporated in this review. It can be observed that 6 studies were published recently (1 study in 2020, 3 studies in 2021, and 2 studies in 2022). Majority of the participants in most of the studies were females and were aged above 30 years with high work experience.
Summary of Study Characteristics Included in This Review.
| Author | Study purpose | Study type | Sample | Measure of leadership/work factors | Measures of nurse performance | Instruments | Reliability and validity | Analysis | Outcomes | Level of evidence | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kim and Sim | To analyze the effect of nursing leadership on nursing practice behaviors | Quantitative | N = 284; 270 F, 14 M; Average age = 42.9 years | Conditions for work effectiveness including access to opportunities, resources, information, and support. | Time spent on nursing care, self-efficacy; relationship between empowerment and self-efficacy | Conditions for Work Effectiveness–II; Caring Efficacy Scale; Manager’s Activities Scale; Nurse Activity Scale | Reported as satisfactory | Multigroup path analysis | Nursing leadership contributed to the empowerment and self-efficacy on practice behaviors; Nursing leadership contributed to the 46% of the variance in nursing practice behaviors overall. | Primary evidence/information from surveys | TREND Statement: 18/22 |
| Caring efficacy | |||||||||||
| El-Azim et al | To examine the structural relationship among clinical nurses’ communication ability, self-leadership, self-efficacy, and nursing performance | Quantitative | 168 nurses (145 staff nurses; 23 nurse managers); 157 F, 11 M; More than 70% participants >30 years | Action oriented strategies, self-reward strategies, constructive thinking | Nursing attitudes, nursing competency, application of nursing process, Leading communication, interpretation ability, self-expression ability, understanding others’ perceptions, nursing ethics, communicating with patients, knowledge of clinical skills | The questionnaire consisted 68 items identified from previous studies, including 9 items on demographic and general characteristics, 16 items on communication ability, 13 items on self-leadership, 16 items on self-efficacy, and 14 items on nursing performance. | Skewness and kurtosis, Cronbach alpha values reported | The error mean square root (RMSEA), the incremental fit index (RMR), the fit index (GFI), the comparative fit index (CFI), and the non-standard fit index (TLI) | Significant effect was identified in the relationship between communication ability and self-leadership; communication ability and self-efficacy. Nurses’ communication ability affected nursing performance through self-efficacy | Primary evidence/information from surveys | TREND Statement: 20/22 |
| Ariani et al | To determine the relationship between head nurses’ leadership styles and nurses’ job performance | Quantitative | 110 staff nurses aged between 20 and 40 years | Transactional (Contingent rewards, management by exception) and transformation leadership (idealized influence, inspirational motivation, intellectual simulation, individual consideration) styles | Courtesy, respect, communication, comfort, responsiveness, team work, professionalism | Leadership Questionnaire; Nurses’ Performance Evaluation (Observation Checklist) | Cronbach’s alpha = 0.96; reliability value ( = .68, < .001) | Correlation analysis | No statistically significant relationship was found between leadership styles and nurses’ performance | Primary evidence/information from surveys | TREND Statement: 21/22 |
| Fing et al | To determine the effect of servant leadership on nurses’ innovative behavior and job performance | Quantitative | 885 staff nurses | Ethical, humanistic, empathic, mutual benefit and service-oriented approaches | Nursing competency, application of nursing process, Leading communication, interpretation ability, self-expression ability | Servant leadership questionnaire; Innovative work behavior scale; Nurses’ Performance Evaluation questionnaire | Reported as satisfactory | Descriptive tests; correlation analysis; and linear and hierarchical regression analyses | Nurse managers’ servant leadership behaviors were statistically significantly related with the nurses’ innovative behaviors and job performances | Primary evidence/information from surveys | TREND Statement: 14/22 |
| Wang et al | To analyze the link between supervisors’ transformational leadership and staff nurses’ extra-role performance as mediated by nurse self-efficacy and work engagement. | Quantitative | 280 nurses; 17 nurse managers; Women >70%; Mean age = 34 years | Inspirational motivation, Intellectual stimulation, Individualized consideration, Idealized attributes, Idealized behavior | Self-efficacy, work engagement, extra-role performance | Multifactor Leadership Questionnaire; self-constructed scale for self-efficacy and extra role performance | Reported as satisfactory | Path analysis; Structural Equation modeling (SEM) | Transformational leadership positively influenced work engagement and contributed to extra-role performance by improving elf-efficacy of nurses. | Primary evidence/information from surveys | TREND Statement: 19/22 |
| Kül and Sönmez | To determine the effect of the leadership style of nurse managers on nurse performances and job satisfaction of staff nurses | Quantitative | N = 70 (nurse managers and staff nurses), predominantly female | Transformational, transactional, laissez-faire, democratic, autocratic styles | Low/high performance; recognizing patients’ needs and providing appropriate care and solutions | Generic Job Satisfaction Scale, self-developed questionnaire for nursing performance. | Reported as satisfactory | Correlational analysis | All leadership styles were significantly correlated with job satisfaction and nursing performance; Only transformational, transactional, and democratic leadership styles were significantly correlated with nursing performance. | Primary evidence/information from surveys | TREND Statement: 14/22 |
| Ryan and Deci | To examine the influence of entrepreneurial leadership on nurses’ innovation work behavior and its dimensions. | Quantitative | 273 nurses; 80% F, 20% M; Average age = 33 years (range: 20-58 years) | Including innovation, driving innovation, risk-taking, passion for work | Idea exploration, idea generation. idea championing, idea implementation | Innovative work behavior questionnaire; Entrepreneurial Leadership questionnaire | IWB (α = .92) | Confirmatory Factor Analysis and Correlations | Entrepreneurial leadership had a significant positive impact on nurses’ innovation work behavior and most strongly improved idea exploration, followed by idea generation, idea implementation, and idea championing. | Primary evidence/information from surveys | TREND Statement: 20/22 |
| Salanova et al | Analyze the impact of work environment, nurses’ performance, behavior, problem-solving skills, and transformational role on sustainable nursing leadership | Quantitative | N = 205 (118 nurse managers, 54 nurses, 12 director nurses, 21 methodologist nurses); 196 F, 9 M; 90% >30 years | Knowledge and awareness | Caring and support, monitoring and controlling, planning and scheduling | Self-developed questionnaire | Reported as satisfactory | Correlation analysis, and multiple linear regression analysis. | Behavior and problem-solving, positively contributed to nursing leadership; Work environment and performance nurse manager did not positively contribute to nursing leadership; transformational ability majorly contributes to the sustainability of nursing leadership. | Primary evidence/information from surveys | TREND Statement: 16/22 |
| Bagheri and Akbari | To analyze the effect of the leadership on nurses’ performance | Quantitative | N = 66; 46 F, 20 M; 68% >40 years | Paternalistic leadership, laissez-faire leadership | Complying with standards, decision-making, ability to accept criticism and suggestions, caring and attentive | Self-developed questionnaire | Reported as satisfactory | Univariate analysis, bivariate analysis, and multivariate analysis | Paternalistic leadership style was identified to be dominant than laissez-faire leadership in improving the nursing performance. | Primary evidence/information from surveys | TREND Statement: 17/22 |
| Gupta et al | To examine the relationship between nurse managers’ transformational leadership and nurses’ job performance | Quantitative | N = 792 (73 nurse managers, 719 nurses) | Idealized influence, inspirational motivation, intellectual simulation, individual consideration | Self-efficacy, work engagement, psychological safety | Transformational leadership questionnaire; Self-developed questionnaire | Reported as satisfactory | Correlation analysis | Positive correlation existed between transformational leadership, psychological safety, and job performance | Primary evidence/information from surveys | TREND Statement: 19/22 |
| Leitch et al | To explore leadership factors that influence nurse performance and particularly, the role that nursing leadership behaviors play in nurses’ perceptions of performance motivation. | Systematic review | Eight studies were included in the review | Autonomy, working relationships, managing resources, individual consideration, caring attitudes | Nurses’ perceptions on performance such as empowerment | N/A | Quality Assessment and Validation Tool for Correlational Studies, Effective Public Health Practice Quality Assessment Tool, Critical Appraisal Skills Program Tool | Descriptive analysis | Nursing leadership behaviors were found to influence both nurses motivations directly and indirectly via other factors; autonomy, work relationships, resource accessibility, nurse factors, and leadership practices; | Secondary/Filtered information | PRISMA:22/27 |
Focusing on the leadership styles, 3 studies considered the effect of different leadership styles on nursing performance, 2 studies exclusively focused on transformational leadership, one each on sustainable leadership, entrepreneurial leadership, and servant leadership. There were 10 studies that have adopted quantitative approach of survey in data collection, and different analysis techniques were utilized in these studies. Only one systematic review was included that focused on the leadership attributes and nursing performance.
Theoretical Framework
Theories in research provides a rationale for developing hypothesis and testing the relationship between the variables, 44 and therefore it is important that the research studies should be guided by theoretical framework or a model that either confirmation of existing theory or generating new theories. Ten out of the 11 studies in this review were guided by a theoretical framework or a model. Six studies 33 - 37 ,45 in this review adopted leadership theories or developed a model for testing the leadership attributes on nursing performance. Social exchange theory and self-determination theories were used in Kül and Sönmez, 38 supporting the role of servant leadership in developing the innovative behavior of nurses (guided by social exchange) and motivating them in improving their performance by developing autonomy, competence and relatedness (self-determination theory: extrinsic motivation from leaders leading to intrinsic motivation among nurses). 39 Another study conducted by Salanova et al 40 emphasized the significance of social interactions in the work environment in improving self-efficacy by adopting social cognitive theory, where self-efficacy is considered as the primary personal resource, and transformational leadership as contextual resource for motivating nurses. In extending the leadership theories, another study 41 linked it with Innovative work behavior theory.
This theory contends that while functional competences give entrepreneurial nursing leaders the ability to inspire nurses to take innovative action while providing care, personal competencies enable them to establish an innovative vision. This builds confidence and commitment to adopting new ideas. 42 , 43 Wang et al 37 argued that leadership is a position that can be achieved by gaining skills, which contradicts leadership theories that suggest some people are born leaders. This also contradicts psychological theory that women have low aggressiveness and avoid leadership positions 46 , 47 However, recent studies focus on theories relevant to changes in the nursing industry, including the introduction of innovative technologies and new business models such as gig economy and eHealth. Many frameworks continue to focus on leadership styles such as transformational and transactional styles and relevant attributes that have been extensively researched over the past few decades. 21 However, new leadership attributes such as nursing informatics leadership, in light of growing influence of technology and industry policies in the quality care sector, have been neglected.
Measures of Nurse Performance
Twenty-two distinct measurement instruments were employed to evaluate the various factors that influence nursing performance in relationship with nursing leadership attributes. Five studies used questionnaires developed by authors for measuring nurses’ performance in relation to different aspects such as motivation, engagement, self-efficacy, performance, problem solving skills, and job satisfaction. Multifactor leadership questionnaires or its components were used in 3 studies focusing on different leadership styles and their impact on nursing performance as a part of the study model designed by respective authors. 34 , 35 , 40 Other major instruments used for measuring nurses’ performance related attributes include Caring Efficacy Scale, nurses’ activity scale, 45 Nurses performance evaluation checklist, 34 , 38 Innovative work behavior scale, 38 generic job satisfaction scale, 35 and innovative work behavior questionnaire. 41
Factors Influencing Nurses’ Performances
A total of 51 different factors that affected the nurses’ performance were identified from the studies included in the review ( Table 3 ). These factors were grouped into 6 categories including autonomy, competencies, relatedness, individual nurse characteristics, relationships and support, and leadership practices.
Factors Affecting Nurses’ Performance.
| Leadership factors | Findings | Work factors | Findings | Studies |
|---|---|---|---|---|
| Autonomy: Behaviors that foster or create autonomy, confidence among nurses, empowerment | Positive | Innovative behavior, competency, application of nursing process, Leading communication, interpretation ability, self-expression ability | Positive | Ariani et al |
| Time spent on nursing care, self-efficacy | Positive | Manojlovich | ||
| Nursing attitudes, application of nursing process, competency, Leading communication, interpretation ability, self-expression ability, understanding others’ perceptions, nursing ethics, communicating with patients, knowledge of clinical skills | Positive | Kim and Sim | ||
| Competencies: Skills that support nurses management and improve their performance | Positive | Idea exploration, idea generation, idea championing, idea implementation | Positive | Kül and Sönmez |
| Caring, supportive, monitoring and controlling, planning and scheduling | Positive | Ryan and Deci | ||
| Complying with standards, decision-making, ability to accept criticism and suggestions, caring and attentive | Positive | Salanova et al | ||
| Self-efficacy, work engagement | Positive | Bagheri and Akbari | ||
| Relatedness: relationship between nurses and nurse managers | Not Significant | Courtesy, respect, leading communication, comfort, responsiveness, team work, professionalism | Not Significant | El-Azim et al |
| Individual nurse characteristics | Positive | Extra-role performance | Positive | Fing et al |
| Psychological safety | Positive | Bagheri and Akbari | ||
| Relationships and support | Positive | Caring, supportive, monitoring and controlling, planning and scheduling | Positive | Ryan and Deci |
| Leadership styles/practices | Positive | Providing training and support, providing rewards, Adopting cooperative culture | Positive | Wang et al |
| Treating co-employees as family members, letting nurses to make their own decisions | Positive | Salanova et al | ||
| Humanistic, empathic, mutual benefit and service-oriented approaches | Positive | Ariani et al | ||
| Driving innovation, risk-taking, passion for work | Positive | Kül and Sönmez |
Three studies 33 , 38 , 45 examined the influence of autonomy related factors on nurses’ performance. Manojlovich 45 identified that strong nursing leadership behavior can contribute to the empowerment and self-efficacy on practice behaviors of the nurses, indicating that nursing leaders should provide more access to structural empowerment factors for nurses and exhibit unit-level nursing leadership. Kim and Sim 33 suggest that utilizing action-oriented and self-reward strategies, along with constructive thinking, can improve self-efficacy and empower individuals, leading to a significant improvement in their performance.
However, it is also observed that nursing performance can be affected by their communication abilities, indicating that in developing autonomy, communication skills play a significant role. Kül and Sönmez 38 identified that servant leadership attributes, such as being humanistic, empathetic, mutually beneficial, and service-oriented, can empower nurses to develop innovative behavior, which can improve their job performance. Innovative behaviors reflect an autonomy in nurses’ attitudes, where they autonomously take decisions in developing new ideas and new ways of delivering care, thereby improving the performance.
Competencies
Four studies 37 , 36 , 41 , 48 examined the influence of competencies related factors on the nurses’ performance. Few of these studies reflected new approaches in leadership and their impact on new areas of performance. For instance, Bagheri and Akbari 41 found that entrepreneurial leadership has positively influenced nurses’ innovation work behavior such as ideas exploration, generation, implementation, and championing, which can improve the overall performances and can support the achievement of organizational goals such as sustainability. Similarly, by creating a positive work environment and effectively managing resources and transformational leadership practices, nurse managers can significantly improve sustainability of nursing leadership. Moreover, Fing et al 36 found that competencies such as treating employees like family members, guiding them, and letting them make independent decisions have led to improvements in several areas that can impact nurses’ performance. These improvements include decision-making, the ability to accept criticism and suggestions. 36 Wang et al 48 found that leaders’ skills, such as idealized influence and intellectual stimulation, have a significant positive impact on nurses’ self-efficacy and work engagement.
Relatedness
Relatedness reflects how the nurse managers relate them to nurses and vice versa, which is reflected in their behavior toward each other. The study conducted by El-Azim et al 34 was the only study that did not find a significant statistical relationship between nursing leadership styles and nurses’ performance.
Individual Nurse Characteristics
Two studies have identified individual nursing characteristics related to nurses’ performance. The interest of nurses’ in taking up extra roles in addition to the existing roles supported by the nurse managers supported by transformational leadership practices through increased work engagement. 40 The findings of this study indicated that through supportive leadership practices, extra-role performance can be enhanced which in turn increases hospital efficacy. Wang et al 48 identified that psychological safety (a belief that nurses won’t be punished or humiliated for sharing ideas, concerns, and issues) could effectively improve nurses’ performance.
Relationships and Support
Wang et al 37 assessed the impact of nursing performance on nursing leadership along with other variables. They found that a caring and supportive work environment can positively affect nurses’ behavior and performance, and in turn, nursing leadership. This emphasizes the need for support from nursing leaders. 37
Leadership Styes/Practices
Although leadership practices were considered in most of the studies, significant approaches can be analyzed from 3 studies. Firstly, as discussed in the autonomy section, servant leadership approaches, such as humanistic, empathic, mutual benefit, and service-oriented approaches, can improve nurses’ competencies and skills, especially their ability to express themselves, communicate, and apply innovative ideas. Secondly, both transformational and transactional approaches, such as motivation, support, contingent rewards, and intellectual stimulation, can improve nurses’ satisfaction levels and job performance. 35 Thirdly, paternalistic leadership practices, such as treating nurses as family members, and laissez-faire practices, such as enabling nurses to make independent decisions, were identified as improving nurses’ performance. However, paternalistic approaches were found to be more influential than laissez-faire approaches. Fourthly, entrepreneurial leadership practices, such as driving innovation, risk-taking, and passion for work, were identified as promoting innovative behavior among nurses, which can improve their performance.
This study mainly focused on examining the link between nursing leadership and nurses’ performance by assessing the factors that nurses believed had an impact on their motivation to perform well; and the leadership behaviors that correlate with nurses’ performance. There has been a significant rise in the identification of number of factors that nurses perceive to be influencing their performance in the recent literature. This study has identified 51 such factors from research studies published since 2005, compared to a study conducted by Ronquillo et al 23 which included studies from 1995 to 2006, identifying 25 factors. This development indicates that significant progress can be observed in the research related to nurses’ leadership and nurses’ performance. One of the interesting findings in the review is that most of the studies (10 out of 11) were quantitative and adopted survey strategy for data collection; and only one study adopted systematic review approach, indicating the gaps in adoption of different methodological approaches in the research, which can contribute to diverse findings.
Most of the previous studies adopted social theories and the self-determination theory in assessing the relationship between nursing leadership and nurses’ performance. As a result, few studies mainly focused on the nurses’ approaches in providing quality care through social interaction, rather than on their personal attributes such as satisfaction, quality of life, and motivation. However, some studies attempted to develop theoretical models, 34 , 35 , 40 indicating the emergence of various constructs and relations between nursing leadership and nurses’ performance. One of the effective qualities of leaders is promoting autonomy among the team and making them self-reliant by developing skills and competencies to improve overall processes. Accordingly, from the findings ( Table 3 ), it was observed that the majority of the factors identified were in relation to leadership practices that focused on promoting autonomy and competencies among nurses
In the past few years, significant developments can be observed in the adoption of Industry technologies such as the Internet of Things, Artificial Intelligence, Cloud computing, block chain technology etc., 49 - 52 giving rise to new form of leadership such as nursing informatics leadership. 53 , 54 These developments can influence various factors within hospital settings, including organizational culture, workload, motivation, values in hospital settings that can directly or indirectly influence nursing performance. However, no studies were identified in this review which considered these developments in identifying the factors that influence nurses’ performance. Studies reviewed indicated that nursing leadership can influence autonomy, 33 , 38 , 45 relatedness, 34 competencies, 36 , 37 , 41 , 48 individual characteristics, 40 , 48 and relationships and support, 37 as perceived by nurses influencing their motivation to perform well. In addition, leadership practices were identified to be nurses’ abilities to perform well. Furthermore, leadership behaviors that support autonomy, inclusivity, transformation (improving skills, innovation abilities, and competencies), and staff prioritization (caring, paternalistic behavior, empathy) can result in high nursing performance. 33 , 38 , 45 It is important that nurse leaders share organizational goals to encourage staff, offer suggestions, and receive feedback on innovative practices for achieving goals in a cooperative and supportive work culture. The studies reviewed suggest leadership plays a crucial role in influencing nurses’ performance in various areas, such as innovation, decision-making, and work engagement. 36 , 37 , 41 , 48 Furthermore, new approaches to leadership, such as entrepreneurial leadership and transformational leadership practices, can positively impact nurses’ performance and support the achievement of organizational goals such as sustainability. 41 Therefore, it is important for nurse managers to continuously develop their leadership skills and create a positive work environment that supports nurses’ ability to perform well. 36 By doing so, nurse managers can help to create practice environments that promote nurses’ ability to perform their roles effectively, thus enhancing overall nursing performance.
While one study included in the review did not find any significant statistical association between nursing leadership styles and nurses’ performance, it suggested that further research is needed to better analyze the relationship between nursing leadership and nurses’ performance by adopting relatedness factors in the areas of advanced leadership approaches and providing performance appraisal. 34 This highlights the importance of considering relatedness factors in nursing leadership to support nurses’ performance and promote positive relationships between nurse managers and nurses.
The results of Salanova et al 40 study highlight the significance of nurse managers adopting transformational leadership practices to increase nurses’ interest in taking up extra roles, which can lead to improved hospital efficacy. Additionally, promoting psychological safety in the workplace can create a supportive work environment that encourages open communication and enhances nurses’ performance. 48 This indicates the nurses should have enough freedom with nurse managers for sharing their opinions without any hesitation or fear, which may benefit both of them.
Therefore, nursing leadership has a significant impact on nurses’ perceptions of the factors that influence their motivation to perform. This impact can be both direct and indirect. Therefore, it is essential to have competent nursing leaders to create practice settings that can foster nurses’ capacity to succeed. In other words, the link between nursing leadership and nurses’ success is critical, and it is necessary to prioritize leadership development in the nursing profession to achieve optimal patient outcomes.
As observed from the recent report by ICN, 30 the lack of strategic and systematic approach by the employers and policymakers is one of the key challenges associated with rising nursing problems. In this context, it may be implied that effective leadership approaches coupled with systematic management of nursing resources could be one of the effective ways to improve nursing performance, retention, and reduced burn-out rates. Accordingly, apart from the patient-related aspects, personal, co-worker, organizational, and societal related factors were identified to be the significantly contributing factors of nurses’ burn-out during the pandemic, 55 highlighting the issues with nurses’ leadership and organizational/employer approaches. In this context, a systematic review on interventions to reduce occupational stress and burn-out, 56 observed that the interventions were effective when they focus at individual level and organization directed, implying the strategic and systematic approach adopted by the employers and led by nursing leaders, with an individualized focus, signifying the relevance of transformational, motivational, and supportive leadership styles. For instance, spiritual intelligence among nursing leaders was identified to be influencing nursing managers’ competencies in managing stress and burn-out, 57 and similar strategies could be directed by employers to effectively manage nursing resources. Such streamlined approaches may be effective in not only improving nurses’ performance, but also in addressing the challenges such as nurses’ burn-out, retention, and increasing stress in the post-pandemic era.
Implications for Nurse Researchers
The findings from this review supports a theoretical model ( Figure 2 ) on factors that influences nurses’ motivation to perform well, which may be tested and evaluated in future research. Analyzing published research till date in this review has suggested that leadership practices that support autonomy, competencies, and relatedness through inclusive approaches reflect that nurses’ contributions are valued and this process resulted in increased motivation of nurses to perform well. In addition, leadership practices that support innovation (entrepreneurial), and cooperative culture (transformational) were identified to be more influencing in improving nurses’ motivation to perform better. Although, different leadership practices and their relationship with nurses’ performance were investigated, significant changes have been observed in the nursing work environment in the past few years. The introduction of innovative technologies and business models, such as the gig economy and online health services, is among the many changes. These changes can lead to new leadership practices and new factors that influences nurses’ performance, such as informatics competencies and skills, remote work culture. These are some areas that future researchers can investigate to identify new leadership practices and the factors that influence nurses’ performance. Furthermore, sustainability has become a core component of all organizations, including healthcare. Therefore, it is important to examine leadership behaviors that can have an impact on nurses’ abilities to help achieve sustainable organizational goals. Furthermore, unexpected disasters such as the recent Covid-19 pandemic has significantly increased the burden on nursing care. Leadership practices in such a highly demanding workload environment and their impact on nurses’ abilities to provide quality care and achieve better patient outcomes could be examined. Finally, it is evident from the review that most of the studies have adopted quantitative methods. Diverse methodological framework adoption can contribute to the quality of research. Therefore, future researchers should focus on adopting other frameworks such as qualitative, and mixed methods in conducting the research.

Proposed theoretical model.
Implications for Nurse Leaders
Nursing performance is a key factor influencing the sustainability of nursing leadership. 37 Therefore, nurse leaders must adopt various leadership practices and behaviors that improve nursing performance, especially those that increase nurses’ motivation to perform better. Leadership practices that encourage employees’ motivation can influence organizational practices and goals. 58 As nurse leaders carry huge workloads, their work effectiveness can be affected, 59 which create barriers and challenges in achieving optimal nursing performance and ultimately providing high-quality care. Addressing nurse leaders’ workload is therefore necessary to enhance their ability to influence nurses and improve overall nursing performance.
Limitations
This review has a few potential limitations. It can be observed that 10 out of the 11 studies reviewed adopted quantitative methods, reflecting the limitation of including diverse methodological studies. Furthermore, reporting bias may exist as published studies tend to over-report positive findings. Many studies used self-designed scales to measure nurses’ performance, and others used different tools, limiting the validity and generalizability of findings. Most of the studies in this review are cross-sectional correlation studies and may be prone to bias 44, but they are helpful in examining the relationship between nursing leadership practices, behaviors, and nurses’ performance, which is the main purpose of this study.
Conclusions
Providing quality care and ensuring patients’ safety are fundamental goals for all healthcare organizations. Since nurses are the primary healthcare providers who spend a significant amount of time with patients delivering care and services, they have a crucial role in achieving these objectives. Nurse leaders who manage the nursing resources are the key personnel who are responsible for overseeing the quality of care and patients’ safety, and therefore they need to encourage nurses’ in better understanding the patients’ needs and values. Strong nurse leaders are effective in implementing evidence-based practices to ensure that these objectives are achieved, as research showed that nursing leadership can both directly and indirectly influence nurses’ performance. The present review has identified 51 factors that nurses categorize under 6 domains, which they believe motivate them to perform effectively. These included autonomy, relatedness, competencies, individual nurse characteristics, relationships and support, and leadership practices/styles. Comprehending these actors is essential and necessary for nurse leaders to promote quality of care and to achieve organizational goals such as sustainability, growth and innovativeness. Therefore, nurse leaders should strive to understand and identify the factors that motivate nurses to perform well and accordingly should address/facilitate these factors through their behavior or leadership styles.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Our study did not require an ethical board approval because systematic reviews generally do not need ethics committee or institutional review board approval,

- Campaign supporters
- Nursing Now Programmes
- Nursing Now Groups
- Global activity map
- Case Studies
- Share your plans
- Nightingale Challenge
- Latest news
- Articles and coverage

- Career advice for aspiring leaders
- Voices of Nursing
Stories of nurse leaders

In tandem with our series of case studies on the Nursing Now ‘Young Nurses’, we are also sharing the stories of some of our nurse leaders.
“We will not be able to achieve UHC unless nurses are involved in decision-making […], in all aspects of health as leaders.”

“I could have taken an easier path to a different location or given up altogether – but I didn’t want to as it just felt right to become a member of this profession.”
Matt daley, rn, john burdett fellow, health education england, when did you first realise you were interested in health and healthcare.
Growing up, I was very squeamish and hated the thought of injury and the sight of blood, but I realised I was interested in health and healthcare whilst serving in the Royal Navy on-board HMS Ark Royal and HMS Illustrious during the Balkans War. During this time. I learnt about the need for humanitarian healthcare due to the conditions ashore. I had some experience in first aid, but wanted to be more involved in helping people directly by providing personal care and intervention. I had an aunt who was a nurse (still is!) and that was the role I aspired to, however, it took some time to achieve this academically and professionally.
How did your career in health begin?
Once I had made a decision to work in health, I was able to transfer my role to the Royal Navy Medical Branch and became a Medical Assistant in the wider general service. This allowed me to gain broad knowledge and experience in emergency, primary and secondary healthcare role settings. After this, I worked as a First Aid Instructor whilst I prepared to enter adult nursing.
I became a Registered Nurse (Adult) in Queen Alexandra’s Royal Naval Nursing Service in 2006, and since then I have worked on wards and intensive care units, with opportunities to work with the Ministry of Defence on innovation and research projects. I completed my military service in December 2013 after 23 years, and have mainly worked in Practice Development since then.
Who inspired you to become a nursing leader?
I have had the good fortune to be surrounded by many inspirational leaders who were compassionate, firm, principled and forgiving. During my time as a military intensive care nurse I liaised often with relatives, staff and wider organisations in very sensitive, highly emotional circumstances. During this time I was personally supported by my Chief Nursing Officer. This experience, and the support I received taught me about the value and impact of compassionate leadership. One particularly poignant time was when she accompanied a new member of the team through the final journey of a patient’s organ donation. Her example has stayed with me and continues to inspire me.
What obstacles did you encounter and how did you overcome them?
I have navigated my way through several career changes and sought new opportunities while striving to maintain family relationships, current role and deployments. I have also had to work on my confidence and willpower. Determination, persistence and self-belief have helped me to get thus far. I could have taken an easier path to a different location or given up altogether – but I didn’t want to as it just felt right to become a member of this profession.
What would you tell your younger self/ a nurse at the beginning of their career?
- Find an inspirational role model, if not from your close peers then look further afield.
- Remember, you are representative of the nursing profession and every nurse from the past, present and future. You have the power to make the profession in the image you want it to be.
- Have aspirations, follow them and believe in your abilities – nurses are bright, clever professionals that make a difference every day.
- Vision is everything, share it and make it a reality, whatever it is. Remember that you may be driving it by yourself for a while.
What are the qualities required to be a nurse leader?
From my experience of observing and interacting with different levels of nurse leadership, I think the qualities of compassion and kindness, combined with staying true to values and principles have demonstrated what I believe are the qualities to be a nurse leader – kind, firm and fair. To this I would add – having the will to drive these outwards into the workplace and influence the wider culture of organisations and the social culture of the communities where we live and work.
If you could change one thing about the health system in the UK, what would it be?
The one thing I would change would be the consistency of access to educational and career opportunities for promising young nurses and midwives. I would change the “system” so that newly qualified nurses and midwives with talent and ambition could be fast tracked into advanced leadership or clinical roles. This would ensure that we recognise and reward talented individuals who are the future of the nursing profession.
Why is it important, in your opinion, for young nurses to be involved in policy and decision making?
In my opinion, young nurses must be involved in policy and decision making in order to make their relevance known and build their influence as a body, alongside medical colleagues. Other professionals have a voice and influence, I think that young nurses should be prepared to establish themselves and bring their own profession forward into this arena. Nurses are at the very heart of healthcare and are present in every area – they understand the fundamental concerns of the patient, family and carers, so should be involved at the highest level to ensure that what is being decided meets the requirements now and later. I was taught to be the patients’ advocate in my profession, and I would expect my younger nurses to speak for me, my generation and future generations when I am no longer able.
How do you think that Nursing Now will make its mark on the future of nursing?
I want Nursing Now to make its mark on the future of Nursing by being the point when things changed for the profession. The global passion for involvement is so encouraging, and this I think is because there is a hunger for connection amongst nurses. I work in a Trust consisting of many nationalities and we are all passionate about delivering the same high-quality of care to our patients. Healthcare systems may be different but the reason the nurses are there is the same in any country, and it is this connection that makes us a very strong force for change globally. Conversation and collaboration are key to this change and growing out of this I would want to see the cross pollination of ideas that means countries work closer together to bring benefits to the profession and populace.
Why is it important for governments around the world to invest in nurses/ the nursing profession?
Investment in nursing ensures the profession has the skills, tools and knowledge to meet the needs of the community at home, as well as in GP practices and hospitals. Nurses are fundamental to a functioning health system in society, a lack of investment would be to the detriment of nursing skill and preventative health measures. It would also make nurses feel under-valued.
“My patients and students challenge, motivate and inspire me to live up to my commitment to nursing excellence everyday.”
Bongi sibanda, dnpc msc-anp fhea rn, advanced practice nurse consultant/educator, apn africa founder .
I always had a keen interest in health as a child. Growing up with many relatives who were in the healthcare industry, especially different nursing roles, was instrumental in my nursing choice. One relative, a community nursing sister used to drive around the city in a company Madza 323 seeing patients in their homes in the 90s, and by then l knew l just wanted to do that too!
I did my pre-registration nurse training in Zimbabwe and by the age of 20, l was already a Registered Nurse. It was one of the great foundations to healthcare practice and one l hold dear to where l am now. Post qualification l worked in a number of roles including mental health, casualty, critical care and clinical research; before practising in the UK from 2004.
Who inspired you along the way to become a nursing leader?
I have worked with a number of incredible leaders within healthcare and beyond and I am privileged to have family members who have held senior nursing roles too; they have all inspired me and held my hand along the way. However, my patients and students challenge, motivate and inspire me to live up to my commitment to nursing excellence everyday. I am truly grateful for this challenge that keeps me curious and looking for ways to serve better daily.
What difficulties did you encounter and how did you overcome them?
Being a nurse leader/academic from a BME background, especially in the area of advanced clinical practice is a challenge in itself in the UK and evidence tells us so. My experience has not been that different; I have had to work twice as hard as my colleagues, navigate prejudice and prove my worth in many clinical/academic roles. Fortunately, I am privileged to have many global leaders who have given me opportunities and supported my work along the way; as a result, l have been able to persevere and stay committed to excellence in nursing practice.
What would you tell your younger self/ a nurse at the beginning of his/her career?
It’s the best career choice young lady; relax and see how it all works out later!
Among other critical qualities of authenticity, commitment to excellence and emotional intelligence; nurse leaders must be well-versed with healthcare business and policy to achieve organisational goals and population outcomes. Therefore, the ability to grasp the bigger picture beyond healthcare industry and remaining curious on business strategy, policy and global issues cannot be underestimated.
If you could change one thing about the health system in your country, what would it be?
Well, l have a number of countries!
First in England and within my area of expertise – Unscheduled Care (Urgent Care and GP Out of hours services), I would like to see more integration of services and single commissioning. This would address a number of issues around commitment to workforce development, especially in advanced clinical practice by all stakeholders, reduce high expenditure on agency/locum staff and improve patient experience/journey in the system.
In Africa, the current reliance on donors and NGOs for the provision of core primary care services in some countries is unsustainable, not congruent with the Astana Declaration and needs to change. Therefore, in collaboration with colleagues, we are working across disciplines and with a number of regional organisations to strengthen primary health care systems and help governments towards achieving Universal Health Coverage (UHC). This includes advocating for the development of Family Nurse Practitioners who are well placed to provide high quality care to under-served /rural populations.
Why is it important, in your opinion, for young nurses to be involved in policy and decision making?
Not only is the future young with over 50% of the world population under the age of 30 years; young nurses are future healthcare leaders who will inherit the legacy of UHC 2030. Therefore we need them at the policy and decision making table now to help them carry this work forward. In my experience of working and mentoring young nurses, l have found them to be innovative with great minds. I have learnt a lot from them too. We must harness this opportunity for the future of our profession and positive patient outcomes.
The current Nursing Now work speaks volumes. The collaboration with WHO, ICN, and Nursing Now has already proved a success in a number of projects; facilitating nursing leaders to be more visible in policy and decision making tables. There is certainly more awareness on the complexity of nursing practice and the need for this to be recognised. The Nightingale Challenge will be one critical area that will make governments commit to investing in nursing and realise the need to do so.
Why is it important for governments around the world to invest in nurses/ the nursing profession?
Nurses are by far the largest workforce across the globe, providing more than 80% of primary care services in many countries. For UHC and health-related Sustainable Development Goals (SDGs) to be achieved; nursing education, scope of practice and leadership must be enhanced and this includes scaling up the number of nurses highly trained in clinical practice (Advanced Practice Nurses). The ageing population of current nursing workforce and the WHO projected shortfall of 18 million health workers means that governments around the world must commit to nursing investment if health services are to be delivered to populations.


How to Write a Good Nursing Application Essay (With Examples)
Wilson logan.
- May 19, 2024
- Nursing Writing Guides
Embarking on a nursing school journey? Becoming a nurse takes more than just desire—it requires a demonstration of commitment and insight into the field of nursing. A pivotal step in your application is crafting a compelling nursing application essay. This piece is your window to express your individuality, passion, and aspirations within the nursing field.

This essay not only showcases your writing prowess and critical thinking skills but also your ability to convey ideas clearly. Creating an outstanding nursing application essay that resonates with the admission committee can seem daunting. You might ponder over questions like: What should my focus be? How do I illustrate my enthusiasm for nursing?
Or even, how do I make a memorable impression on the admissions panel and steer clear of common pitfalls?
In this guide, we aim to address these queries and more. We’ll navigate you through crafting an impactful nursing application essay, coupled with insights, examples, and best practices to forge a personal and persuasive narrative. Embrace this advice, and script an essay that mirrors your unique path, your goals, and your dedication to the nursing vocation, positioning you as an ideal candidate for your chosen nursing program.
Nursing Essay Application Writing Service
- Experienced and Qualified Writers
- Personalized Attention
- Strict Quality Control
- Timely Delivery
- Confidentiality and Privacy
- Affordable Pricing
Understanding the Importance of a Nursing Application Essay
A nursing application essay stands as more than merely an academic composition. It plays a pivotal role in the nursing school admission process, where crafting a persuasive piece may distinguish you as an exceptional candidate among those who want to be nurses. The inclusion of personal experiences, achievements, objectives, and motivations behind your desire to become a nurse communicates to the admissions team your suitability for their program.
This essay acts as your personal voice throughout the admission journey. It offers a platform to directly address the admissions committee, narrate your story, and articulate your attraction to the nursing profession. The significance of this essay cannot be understated, as it often becomes the critical element in differentiating you from the pool of applicants, especially when you want to include experiences that underscore your suitability to become a nurse.
It mirrors your past experiences, future ambitions, and dedication to the principles upheld by the nursing profession.
To enhance the likelihood of your application’s acceptance, it is essential to excel in crafting your nursing school application essay. This necessitates dedicative planning. Focus on identifying key points you wish to include in your essay, encapsulating your personal journey, and integrating your achievements.
Initiate your essay with an engaging introductory statement to captivate your audience. It’s imperative to convey to the readers who you are and the significance of nursing to you.
The value of a nursing school essay extends beyond just satisfying an application criterion—it represents a chance to humanize your application. Picture your application as a canvas; your academic achievements and certificates illustrate your scholarly and technical expertise. However, the nursing essay adds dimension and vibrancy to this canvas, imbuing your application with life and allowing you to showcase your distinctiveness.
In the highly competitive realm of nursing school applications, your essay assumes a critical role in setting you apart from the competition. Amid numerous qualified applicants, your essay offers a window into your unique character, detailing your personal journey, challenges, successes, compassion, and enthusiasm for nursing.
Furthermore, it provides applicants with an opportunity to demonstrate their proficiency in coherent communication, an essential skill for nurses required to effectively interact with patients, families, and healthcare teams.
Creating a compelling nursing application essay that secures your admission to your desired nursing school or program demands meticulous planning, research, and creativity. In the forthcoming sections, we will furnish you with tips, examples, and best practices to aid you in developing a personal and impactful nursing school essay.
Preparation Before Writing
Embarking on your nursing school personal statement requires preliminary legwork to ensure you’re well-informed about the essay prompt and the nursing school of your choice. This crucial step will enable you to write a personal statement that resonates with the admissions committee’s specific criteria and expectations. Follow these essential steps:
Comprehending the Prompt
The inaugural step involves thoroughly understanding the prompt and the nursing application essay requirements. The prompt is essentially the question or statement your essay needs to address, focusing on your interest, motivation, and objectives in pursuing a nursing career. Familiar prompts include:
- Your motivation for choosing nursing as a career
- Your immediate and long-term nursing goals
- How the nursing program will facilitate your goal achievement
- Key qualities that define an exemplary nurse
- The experiences shaping your nursing career choice
Decipher the prompt by identifying pivotal words and phrases signifying the essay’s intended purpose, scope, and tone. If it necessitates a description or explanation, ensure you provide comprehensive and factual information. Conversely, prompts demanding analysis or evaluation require a critical and reasoned outlook, while persuasion calls for a compelling argument.
Adhere to the essay’s stipulated requirements, including word count, format, style, and submission deadline, to avoid penalties or disqualification. For any uncertainties regarding the prompt or requirements, engaging with the nursing school for further clarification is advisable.
Researching the Nursing School
The subsequent step involves detailed research into the nursing school or program of interest. This showcases your enthusiasm and familiarity with the specific nursing field and institution and ensures your essay is in consonance with the school’s mission, vision, and values.
Employ a variety of sources for your research, like the school’s official website, promotional materials, social platforms, alumni feedback, and online reviews. Interactions with the nursing school’s faculty, staff, or students can also offer deeper insights.
Key research areas should include:
- The history, reputation, and accreditation status of the nursing school or program
- The academic offerings, faculty expertise, and curriculum structure
- Details on the admissions criteria, selection process, and statistics
- Available facilities, resources, and extracurricular opportunities
- The institutional culture, values, and overarching goals
As you compile your findings, maintain detailed notes and source references to ensure proper citation and avoid plagiarism. Focus on integrating information that reinforces your main arguments while omitting any superfluous details that might detract from your message.
Crafting Your Essay
Once you’ve grasped the essay prompt and researched your chosen nursing school thoroughly, it’s time to embark on the writing process. Crafting an engaging nursing personal statement is no small feat—it demands meticulous planning, organization, and a touch of creativity. Follow these key steps to ensure your essay stands out:
Creating an Outline
Begin by drafting an outline, a crucial step that provides a structured framework for organizing your thoughts and arguments clearly and coherently. An effective outline helps prevent redundancy, irrelevant content, and omissions, typically featuring three main sections: the introduction, body, and conclusion.
The introduction should present who you are, your enthusiasm for nursing, and your core thesis statement—the primary message you wish to communicate to the admissions panel. This statement needs to be succinct, transparent, and precise.
For instance, a compelling thesis statement might be, “Driven by a genuine desire to aid others, my robust academic foundation, and a personal journey towards nursing, I am poised to pursue a nursing career.”
In the body, elaborate on your thesis with supportive evidence, examples, and anecdotes. Structure the body into several paragraphs, each spotlighting a distinct idea tying back to the thesis. Open each paragraph with a topic sentence introducing its main idea, and conclude with a sentence that summarizes the idea and transitions into the next section.
An example structure could include paragraphs dedicated to your passion for helping others, your educational background, and a defining personal experience.
The conclusion is your opportunity to reiterate your thesis, encapsulate your primary arguments, and make a memorable impression on the admissions committee. Summarize your points without introducing new ideas, highlighting the significance of what you’ve discussed. Conclude with a potent statement reflecting your enthusiasm, confidence, and appreciation, something akin to, “I am confident in my ability to thrive as a nurse and contribute significantly to the nursing profession. It would be a privilege to join your esteemed nursing school and gain insights from your distinguished faculty and staff.”
Writing an Engaging Introduction
The second step involves crafting a captivating introduction . This segment, being the admissions committee’s first point of contact with your essay, should seize their interest immediately. Employ strategies like a compelling hook—a question, a quote, an intriguing statistic, or a personal story. For instance, “Witnessing a car accident at the age of 12 profoundly transformed my perspective on life.”
Following your hook, offer necessary background information that frames your essay. Briefly introduce yourself, explain your interest in nursing, and your reasons for applying to the specific nursing school or program, invoking the school or program’s name to demonstrate your detailed interest and familiarity.
The introduction’s final element is your thesis statement, which should clearly, concisely, and specifically outline the main argument or message you aim to convey, along with a preview of the key points or ideas that will be further explored in the essay body.
Developing the Body of Your Essay
The body of your essay is where you flesh out your thesis statement with concrete evidence, engaging examples, and compelling narratives. Ensure each paragraph focuses on a singular idea relevant to your thesis, introduced via a topic sentence and concluded in a way that seamlessly leads to the subsequent point.
Employ a mix of sentence structures, lengths, and vocabulary to keep the essay dynamic and engaging. Use transitional phrases like “firstly,” “secondly,” “however,” and “consequently,” to ensure a coherent flow between paragraphs. Be mindful of the essay’s word count, format, style, and tone, adhering to the nursing school’s guidelines to maintain a professional and positive tone throughout.
Concluding with Impact
The conclusion is your final chance to influence the admissions committee. Reinforce your thesis statement and summarize the essay’s core points, underscoring their relevance and demonstrating how they align with the nursing program’s values and objectives. Avoid introducing new information; instead, solidify the arguments you’ve presented and their significance. Conclude with a powerful statement that encapsulates your main message, reaffirms your commitment and suitability for the program, and expresses gratitude for the committee’s consideration. For example, “Confident in my potential to excel in nursing and make meaningful contributions to patient care, I am eager to join your nursing school and absorb knowledge from your esteemed faculty. Thank you for considering my application.”
Personalize Your Essay
To ensure your essay captivates the admissions board, infusing it with your personal touch is crucial after you’ve laid down its structure, crafted an engaging introduction, built out the body, and concluded with impact. Making your essay uniquely yours involves shining a light on your distinctive traits, expressing your desire to become a nurse, and demonstrating your empathy and compassion.
Follow these steps to add that personalized flair:
Highlighting Your Unique Qualities
Begin by spotlighting the singular qualities that render you an excellent fit for the nursing program. Discuss your personality, strengths, skills, and achievements to illustrate your readiness and suitability for a career in nursing.
It’s also key to share stories of any hurdles you’ve overcome, showcasing how these experiences have molded your character and spurred growth. Use specific, relevant anecdotes to bring these qualities to life, employing confident and positive language. Remember to stay true to yourself, dodging the pitfalls of clichés and overstatements, while ensuring you’re not redundantly repeating your resume but instead revealing new facets of your profile.
Sharing Your Nursing Aspirations
The next phase involves sharing your ambitions within the nursing field, detailing your career objectives and what sparks your enthusiasm for nursing. Clarify why you want to become a nurse, your goals as a registered nurse, and how you aim to make a difference. Discuss any particular interests or specializations and their resonance with your chosen program.
Your narrative should convey a realistic, yet passionate vision, highlighting your excitement for nursing, its alignment with your principles, and your cognizance of the profession’s evolving landscape. This is the moment to express your eagerness for lifelong learning in nursing and how the program will bolster your career trajectory.
Showcasing Empathy and Compassion
Lastly, your essay should illustrate your empathy and compassion—fundamental traits of a nurse. Empathy reflects your capacity to understand others’ feelings, whereas compassion showcases your desire to assist and care. Narrate instances where you’ve exemplified these virtues in personal or professional scenarios, emphasizing their impact on your nursing ambition.
Utilize emotive and vibrant language supported by concrete examples to depict your compassionate actions and their transformative influence on your life and nursing philosophy , illustrating how they cement your ethical framework and inform your patient care approach.
Polishing Your Essay
After highlighting your unique qualities, sharing your nursing aspirations, and showcasing empathy and compassion within your essay, it’s crucial to refine it to perfection. Polishing includes seeking feedback, editing, and proofreading to enhance the essay’s content, structure, and style. Here are some tips to help you write a strong essay perfect for the application process.
Follow these steps to elevate your essay:
Seeking Feedback
Gathering external feedback is your initial step. This can be from friends, family, mentors, teachers, or professional editors. It’s a way to identify your essay’s strengths and shortcomings and offers suggestions for refinements. Feedback also provides a fresh perspective, akin to viewing your essay through the admissions committee’s eyes.
Choose a reviewer who is knowledgeable, honest, and supportive. Provide them with the essay’s prompt and requirements, and ask for an assessment based on:
- Content: Does your essay respond to the prompt and address key points? Does it offer ample evidence and stories to back your thesis? Does it reflect your personality, passion, and nursing ambitions?
- Structure: Is your essay logically organized with an engaging introduction, coherent body, and strong conclusion? Are transitions and sentences used effectively to connect ideas?
- Style: Does your essay adhere to a clear format (APA, MLA, Chicago) for citations and plagiarism prevention? Is the style formal and professional, free from slang, jargon, and contractions? Does it maintain a positive tone without negativity or exaggeration?
- Grammar: Are spelling, punctuation, capitalization, and grammar correct? Does the essay utilize varied sentence structures and word choices to enhance readability?
Upon receiving feedback, thank the contributor, review their insights carefully, remain open-minded, and view this as an opportunity to refine your essay. Avoid taking feedback personally; instead, see it as a means to enhance your work.
Editing and Proofreading
The subsequent step is editing and proofreading your essay to correct any errors or inconsistencies. While editing focuses on improving content, structure, and style, proofreading targets grammar, spelling, punctuation, and format accuracy.
During editing, concentrate on your essay’s overall quality. Ensure it fulfills the prompt, supports your thesis with relevant examples, portrays your aspirations and personality, maintains coherent organization with a compelling opening and conclusion, employs transitions effectively, follows a consistent citation format, and presents a formal style with a confident tone.
In proofreading, zoom in on details and accuracy. Verify grammar, spelling, punctuation, and format correctness, and ensure adherence to the nursing program’s requirements like word count and style guidelines.
Utilize tools and techniques like reading aloud, spell checkers, grammar checkers, style guides, dictionaries, thesauruses, peer reviews, professional services, and checklists fora thorough revision. Revise multiple times until your essay reaches its best version, ready to apply for nursing school.
Example Essays and Analysis
In this informative section, we present two exemplar nursing school personal statement examples that successfully encapsulate the ideals of engaging and effective writing, as previously explored. These samples serve as a beacon of inspiration, illustrating best practices for prospective nursing students aiming to craft compelling narratives of their own experiences and goals.
It’s crucial, however, to regard these essays as models rather than templates. The uniqueness of each essay stems from the personal stories and individual journeys of the writers. As such, your essay should be a mirror reflecting your personal aspirations, experiences, and character.
Sample Nursing Application Essay 1
The essay that follows was penned by Jane Doe, a hopeful applicant to the Accelerated Bachelor of Science in Nursing program at Northeastern University. The essay addresses the prompt, “Why do you want to pursue a career in nursing?” with a compelling narrative.
At the age of 12, a car accident unfolded before me, forever altering the trajectory of my life. A woman, engulfed by flames within her vehicle, screamed for help. I dashed to the closest phone booth, dialed 911, and soon, paramedics were on the scene, waging a battle against time and flames. Their success in rescuing the woman left an indelible mark on me, sparking a determination to emulate their bravery and compassion.
My name is Jane Doe. My application to the Accelerated Bachelor of Science in Nursing program at Northeastern University is driven by a lifelong fascination with human health, a profound desire to aid those in distress, and a rich tapestry of academic and professional experiences that have groomed me for a nursing career.
My passion lies in serving those who are vulnerable, providing care and comfort in their times of need. Volunteering across various health settings and participating in community engagement initiatives have enriched my skills in empathy, communication, and teamwork.
Furthermore, an extensive academic background in biology and psychology from Boston University, coupled with practical research experiences, has laid a solid foundational knowledge critical for a nursing career.
A defining moment came when, at 12, I witnessed my aunt suffer in a harrowing car accident. The compassionate care she received from her nurses during recovery illuminated the profound impact of nursing on patient and family alike, steering me toward this noble calling.
This essay encapsulates my unwavering passion for nursing, my academic preparedness, and a deeply personal inspiration. These elements not only shape my ambitions but also epitomize the qualities and drive necessary for success in the Accelerated Bachelor of Science in Nursing program at Northeastern University. It would be an honor to contribute to and learn within this esteemed nursing community.
Thank you for considering my application.
Sample Nursing Application Essay 2
Our next essay is by John Smith, who seeks to further his nursing career through the Master of Science in Nursing program at the University of California, Los Angeles, aiming to articulate his short-term and long-term nursing goals.
My journey towards nursing began in childhood, deeply influenced by a family legacy of nursing professionals. My mother’s battle with breast cancer and the exceptional care she received highlighted the profound role nurses play both in patient recovery and as pillars of support, solidifying my resolve to join their ranks.
As John Smith, an applicant to the Master of Science in Nursing program at UCLA, I bring a robust background in nursing, having earned a bachelor’s degree from the University of California, San Francisco, and garnered extensive hands-on experience in various clinical settings.
My immediate aspiration is to excel in the UCLA Master of Science in Nursing program as a step towards becoming a nurse practitioner, a role that promises both personal fulfillment and professional advancement. My vision extends to becoming a nursing educator and leader, dedicated to elevating nursing practice through teaching, research, and advocacy.
These goals reflect not only my aspirations but also my potential to contribute meaningfully to the UCLA program and the nursing profession at large. I am eager to embark on this next phase of my professional journey, guided by the exemplary faculty and peers at UCLA.
Thank you for your consideration.
Writing Techniques Demonstrated
The essays showcased here exemplify the core writing strategies discussed in prior sections. These include:
- Thoroughly addressing the essay prompt and adhering to its requirements.
- Conducting diligent research on the nursing program to tailor the essay with insightful knowledge.
- Structuring the essay coherently with a compelling introduction, a well-supported body, and a memorable conclusion.
- Infusing the narrative with unique personal insights and a clear demonstration of empathy and compassion.
- Meticulously refining the essay through thoughtful revisions and feedback to polish the final submission.
3 Typical Problems in Writing a Nursing Application Essay
Lack of focus.
When crafting a nursing application essay, one common pitfall is a lack of focus. Applicants often struggle to narrow down their ideas to a coherent narrative that effectively communicates their passion and qualifications for nursing. This can lead to an essay that feels scattered or unfocused, making it difficult for admissions committees to discern the applicant’s main message.
Too Much Information
Another issue is the tendency to include too much information. In an attempt to cover all their bases, applicants might overload their essays with too many details, from personal anecdotes to technical explanations of nursing concepts. This not only overwhelms the reader but also dilutes the impact of the most important points. Striking the right balance between being thorough and concise is key to a compelling essay.
Poor Writing Skills
Finally, poor writing skills can severely detract from an otherwise strong nursing application essay. Grammatical errors, awkward sentence structures, and improper formatting can distract from the content, making it hard for reviewers to focus on the applicant’s strengths. Investing time in proofreading and possibly seeking feedback from others can significantly improve the quality of the essay.
In this blog post, we’ve shared a detailed and actionable guide to crafting a standout nursing application essay. We’ve explored the importance of the nursing school application essay in the application process, offered tips to write an effective nursing school personal statement, and highlighted the best nursing programs’ expectations. Our advice on personal essay preparation, essay composition techniques, and steps to personalize your writing aims to help you craft a compelling nursing personal statement that articulates your desire to pursue a nursing degree.
- The significance and goals of the nursing application essay.
- Preparation steps, including comprehending the essay prompt and researching your chosen nursing school.
- Essay composition techniques, such as outlining, crafting an engaging introduction, developing a coherent body, and finishing with a memorable conclusion.
- How to inject personality into your essay by showcasing your unique traits, articulating your nursing ambitions, and demonstrating your empathy and compassion.
- Tips for refining your essay, such as soliciting feedback, and the importance of thorough editing and proofreading.
- A list of common pitfalls to avoid, like losing focus, providing excessive information, or showcasing inadequate writing skills.
- A review and analysis of two successful nursing application essays.
To clinch a spot in the best nursing programs, remember a well-written essay can serve as a winning nursing application essay. Your personal narrative takes center stage in the admissions landscape; it’s an influential piece that can sway the admission committee’s decision. With our guidelines and personal examples, we trust that writing your personal statement for nursing school will be an enriching and productive endeavor. So polish that strong essay—it’s an essential step toward your future nursing job.
Should you seek further assistance or inspiration, resources and professional services are available to help you craft a compelling nursing essay. Your application essay is a testament to your commitment to the field of nursing as you apply for nursing school. It’s crucial to apply the strength of your convictions and aspirations into the writing process, showcasing a personal narrative that resonates with the values and goals of the nursing program you’re eager to join.
Frequently Asked Questions on How to Write a Good Nursing Application Essay
1. how important is a nursing application essay for those who want to be a nurse.
A good essay is crucial for individuals aspiring to become nurses. It is typically a key component of the application process for nursing programs and provides applicants with the opportunity to showcase their passion, skills, and experiences.
2. What are some tips for writing a compelling nursing application essay?
When crafting your essay, consider using essay examples as a reference. Focus on highlighting your strengths, motivations to pursue nursing , and unique qualities that make you a strong candidate. Additionally, tailor your essay to each college application to demonstrate your genuine interest.
3. Why do you need to write a compelling nursing application essay?
To make your nursing application stand out among other applicants, it is imperative to create a compelling essay that showcases your passion for the field, your relevant experiences, and the reasons applying to nursing is important to you.
4. How can you make your nursing application essay more impactful with the use of examples?
Utilizing best examples in your essay can help illustrate your points and provide concrete evidence of your qualifications and attributes. Including specific scenarios or experiences can make your essay more compelling and memorable to reviewers.
5. What should you consider when making the decision to become a nurse and including it in your essay?
When discussing your decision to become a nurse in your application essay, reflect on your personal motivations, experiences that influenced your choice, and the qualities you possess that align with the nursing profession. This can help admissions committees understand your genuine passion for nursing.
6. Why are examples of nursing personal statement important in the nursing application process?
Nursing personal statement examples serve as valuable resources for applicants to understand the structure, tone, and content expectations for their own essays. They can also provide inspiration and guidance on how to effectively convey one’s story and aspirations.
7. What specific aspects should you highlight in your nursing application essay to showcase what you bring to the table?
Focus on application materials that emphasize your unique attributes, experiences in the healthcare field, skills, and qualities that make you a strong candidate for the nursing program
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Topics and Ideas
Related Posts
- Kathleen Masters Nursing Theories: A Framework for Professional Practice
- Rural Nursing Theory: A Guide for Nursing Students
- Barbara Resnick Nursing Theory: A Comprehensive Guide for Nursing Students
Important Links
Knowledge base.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org

Sign up to our Newsletter
How to write a personal statement for nursing school.

Reviewed by:
Jonathan Preminger
Former Admissions Committee Member, Hofstra-Northwell School of Medicine
Reviewed: 6/19/23
Writing a personal statement for nursing school can be a daunting task, but we’re here to help! Here’s everything you need to know about writing a personal statement for nursing school.
Writing your personal statement is a nerve-wracking experience, no matter what program you’re applying for . You may be wondering: “what are nursing schools looking for in a personal statement?” or, “how can I make my personal statement for nursing school stand out?” Lucky for you, we’ve got some answers.
Here we’ll cover everything you need to know about writing a personal statement for nursing school. We’ve included a breakdown of the components to include, examples of nursing school personal statements, and tips to improve your own.
Let’s get started!

Get The Ultimate Guide on Writing an Unforgettable Personal Statement

What Is a Nursing School Personal Statement?
When applying to nursing schools , you’ll most likely notice that most applications require a personal statement. A personal statement is a short essay, typically no longer than two pages, that tells your target schools a little bit about who you are.
Each school has different expectations for the length and contents of your personal statement, so make sure to check the specific requirements of your target schools. Some common topics include your personal goals for nursing school and why you want to become a nurse.

Nursing School Personal Statement Format
Before writing your personal statement for nursing school, you should plan out what you want to include. If your school does not ask you to answer a specific question with your essay, here is a list of what you should include in your nursing school personal statement.
An Introduction
The introductory paragraph should focus on what brought you to this point. Your school primarily wants to get to know you as a candidate through your personal statement. Your intro should include things like:
- How you first became interested in nursing
- What inspires you about becoming a nurse
- What you intend to achieve through a nursing degree
In this paragraph, your main goal is to introduce yourself and give the admissions committee a bit of background on your passion for nursing. Perhaps you have a family member who inspired you to pursue nursing, you grew up near a hospital, or you’ve struggled with health issues yourself - these are all great examples of an origin story.
Think to yourself: “If my journey into nursing school was a movie, how would it begin?”
Body Paragraph(s)
In the body paragraph(s) of your nursing school personal statement, you can include a bit about your achievements. However, this isn’t the place to simply list your achievements.
Think about how your experiences helped you to develop skills for nursing school . Include things like:
- How you’ve furthered your interest in nursing through experience (both in and out of school)
- How your achievements make you a good fit for the program
- Specific things about the program that interests you
The body portion of your essay should contain the majority of the information you want to include. Make sure to only include accomplishments if they help to explain how you’ll contribute to the program. Your CV will list any other achievements that don’t come into play here.
A Strong Conclusion
Your personal statement should end on a positive note. Think about summarizing your statement by looking toward the future. Include things like:
- Your future ambitions following nursing school
- What you’ll be able to contribute to the program
The end of your body paragraph(s) should mention what you hope to achieve in the future with your nursing degree and lead into your conclusion. The final sentences of your personal statement should further state your passion for your program and how you’ll be a great fit at your target school.
What Not to Write in a Personal Statement for Nursing School
Before getting into our tips and examples, let’s go over what not to include in your personal statement for nursing school. Here are some common mistakes to avoid when crafting your personal statement.
Keep it Simple
Your personal statement should be authentic and genuine, but make sure to keep the brief in mind while you’re writing. As mentioned above, a personal statement is typically no longer than two pages in length.
You should absolutely include some personal anecdotes; in fact, we encourage it! Just make sure to stick to the relevant parts of your story and not to elaborate too much on areas that are not relevant to your application.
Do Not Reiterate Your CV
Your personal statement is an essay, not a resume. Keep in mind that your application already contains all of your achievements on your CV, transcripts, and other application materials.
Your personal statement is about understanding your passion and motivations. You can use examples from your CV to further assert your interest in the program, but only if you can elaborate on how they’ve specifically helped you on your journey to nursing school.
Tips for Writing a Stellar Nursing Personal Statement
Let’s go over a few tips on how you can improve your personal statement. Using these tips can help to make your personal statement and essays for your nursing school application stand out while remaining authentic and genuine.
Create A Timeline
When writing your personal statement, your focus should be on telling your story. Creating a clear timeline of events can help to effectively tell the story of how you decided to apply for nursing.
Start with how you became interested in nursing, develop your story with experiences that have cultivated your knowledge, and conclude by talking about your program and your future goals. A timeline will make your essay easy to read and give the admissions committee a good idea of your journey so far.
Stick To the Brief
If your target school(s) give you a specific prompt for your personal statement, make sure to refer back to the prompt while writing your essay to ensure you’re staying on track.
For example, if your prompt asks you a question, be sure to answer the question at the beginning, the end, and throughout your essay. Your personal statement shouldn’t be vague or veer too far off course.
Speak From the Heart
It is crucial in your nursing personal statement to share what makes you unique . This is your chance to show the admissions committee why you’d be a perfect fit in their program and demonstrate what you bring to the table.
Include genuine experiences that have pushed you toward nursing throughout your life. Conveying your passions and motivations is critical in your personal statement for nursing school.
Do Your Research
One great way to make your nursing personal statement stand out is to do thorough research on your program and include it in your piece. Showing your passion for the specific program. you’re applying to can give you an edge over others and impress the admissions committee.
When you include your research, be sure to add it organically into your writing. Use your research as a way to connect your personal experiences to the program rather than simply listing information.
Nursing School Personal Statement Examples
Here are two nursing personal statement examples that were written successfully. We’ve also included explanations of how they are good examples to help you improve your own personal statement.
*Important note: Do not use our samples in your nursing school application. These examples are meant to serve as a guide when crafting your own original personal statement for nursing school.
Example #1: Indeed ’s Nursing School Personal Statement Sample
“I walked backward down the hill, my arms supporting the weight of the wheelchair as its wheels rolled slowly in reverse. Sunlight danced through the trees around us and shone in my grandmother's hair as she sat inside the wheelchair. I couldn't see my grandmother's face from that angle, but I could hear her laughing with joy as she enjoyed the outdoors for the first time in weeks. My grandmother came to live with my family two years ago after breaking her hip. Although she completed much of her recovery at our home, Nurse George came by every day to perform my grandmother's personal care tasks, monitor her vital signs and assist with her physical therapy exercises. George also taught me some basic patient care practices, such as how to support a wheelchair correctly while going downhill. I had never considered a career in nursing before, but George helped me see the rewards of helping people with their medical conditions and injuries. I am excited by this opportunity to apply to Fern Hill's College of Nursing because I appreciate your program's specialization in rehabilitation nursing. Being a part of my grandmother's recovery team has inspired me to pursue a nursing career that helps patients recover from injuries or medical conditions. I believe that your school's emphasis on assisting patients in regaining their independent skills can help me achieve these professional aspirations. Since realizing that I want to become a nurse, I have become a regular volunteer at Jefferson Rehabilitation Center. I mentor young people struggling with drug addictions and provide childcare for the children of rehabilitation patients. There is no feeling comparable to when a mentee or outgoing patient offers you a sincere "thank you." I can no longer imagine pursuing a career where I do not get to help people overcome their challenges and navigate their way to recovery. My experiences helping my grandmother and patients at Jefferson have taught me the value of empathy and communication. Frequently, my mentees simply want someone to listen to them. I do my best to give them a judgment-free space in which to share their stories. Whether the medical issue is emotional or physical, patients appreciate working with flexible and considerate people. I believe I embody these qualities by actively listening and letting patients talk at their own pace. I am ready to pursue a nursing career and learn about helping patients in a more professional and technical capacity. Fern Hill's College of Nursing is the ideal place to prepare for my future nursing career.”
Why this is a good example: In this example, the writer has done an excellent job of telling the story of how they became interested in nursing. They also develop a clear timeline of events from when they first thought about nursing to how they began developing their skills through volunteering.
Most importantly, the candidate mentions specific reasons why they’re interested in the program and how they feel they can contribute to the school and field.
Example #2: Johns Hopkins University Nursing Personal Statement Sample
“I grew up close to a hospital, where I watched patients go through the double doors for a variety of ailments. From a young age, this drove me to develop a strong interest in the field of medicine. I knew that I wanted to pursue a career in the future that would allow me to take care of those in need. Through my courses in the natural sciences as well as social studies, I have continued to develop my knowledge in the field in order to be ready to continue my education. Now, I am ready to take the next step in my education by applying for the Nursing program at Johns Hopkins University. Three years ago I completed a nursing shadowing internship that opened my eyes to many of the daily struggles of being a nurse. During my time in the clinic and on the wards, I had the opportunity to work In the critical care and trauma ward as well as In obstetrics and geriatrics. These various experiences showed me the diverse role that nurses play in a healthcare setting, and emphasized the importance of empathy and dedication to patient care. Johns Hopkins University Is known worldwide for its focus on patient wellness and medical research. As a nursing student at Hopkins, I hope to not only further the institution's goal of providing exceptional patient care, but also to assist with the many clinical trials ongoing at the hospital that pave the way for new treatments. Through hands-on training with knowledgeable staff, I know that I will be able to make the most of my nursing training at Johns Hopkins and become a nursing professional that is capable of enhancing patient wellness in a healthcare setting.”
Why this is a good example: In this example, the writer develops a clear timeline and clearly defines their relevant information. The writer covers when they first became interested in nursing, courses they’ve taken, and what experiences have made them get serious about the profession.
Finally, they include why they are specifically interested in the program at Johns Hopkins and conclude by adding what they will add to the program as a student.
FAQs: How to Write a Personal Statement for Nursing School
Here are some answers to frequently asked questions about nursing school personal statements.
1. Do All Nursing Schools Require A Personal Statement?
Almost all nursing schools require a personal statement, which can typically be described as a short essay (2 pages or less) that explains who you are and why you want to attend the school’s nursing program.
2. Is a Personal Statement for Nursing School an Essay?
Yes, a personal statement is a short essay that briefly describes your past, present, and future experiences in relation to nursing.
3. How Long Should A Nursing Personal Statement Be?
Each nursing school has different length requirements, which can typically be found in the prompt. If no length is specified, two pages or less is recommended.
4. What Should I Include In My Nursing School Personal Statement?
Your nursing personal statement should include:
- Why you want to become a nurse
- What inspires you about nursing
- Elaborate on the experiences you’ve had that have taught you about nursing
- Program-specific reasons for your interest in the school
- How you intend to contribute to the program and the field of nursing
If your school’s personal statement asks a specific question, that question should be answered throughout your essay.
5. Does Nursing Require Essays?
Yes, most nursing program applications require personal statement essays, and some require secondary (or supplemental) essays as well.
6. When Should I Write My Personal Statement for Nursing School?
You should begin writing your personal statement(s) for nursing school as soon as you receive the prompt. Make sure to give yourself an adequate amount of time to complete all sections of your application before the deadline.
7. How do you Start a Personal Statement for Nursing School?
To start a compelling nursing personal statement, there are a few different writing techniques you can use. You can start by introducing yourself, start by talking about how you became interested in nursing, or you can start “in the action” by cutting right into your story.
Final Thoughts
Your personal statement for nursing school should be genuine, heartfelt, and express how you will make an excellent addition to your target school’s nursing program through a series of examples.
Each personal statement you write should be adjusted to suit the individual program you are applying for. Sending a general personal statement with every application you submit is impersonal and not recommended. Make sure to follow your brief closely and map out your essay before writing it to ensure you include all of the relevant information.

Schedule A Free Consultation
You may also like.

Pharmacy Schools That Don’t Require PCAT
%20(1).png)
Average GPA & DAT Scores for Dental Schools in the US (2024)

Just added to your cart

Leading and Managing Nursing Care Reflective Essay Sample for Adult Nursing
Reflective portfolio based on three reflective narratives of 1500 each related to practice; the issue of professional values like emotional intelligence, resilience, and prioritisation using one model for all narratives.
Emotional Intelligence
The model utilised to undertake this and the other reflective analysis in this commentary is the Gibbs’ reflective cycle. As Johns (2017) point out, there are a lot of reflective models that might be used, but the Gibbs’ model has been selected because it provides a structure and helps with the consideration of numerous factors that might drive deeper, more insightful learning (Howatson-Jones, 2016). Chang and Daly (2015) argue that the Gibbs’ model may only encourage basic reflection, but I have personally found that for me it helps me to explore a depth and range of factors, as highlighted by Howatson-Jones, 2016) and this is why it was selected. The Gibbs model has six stages and each is considered in turn under a new heading.
Description
Emotional intelligence is defined by Ashkanasy et al. (2016) as being a group of capabilities that help in working with emotions. It is the ability to be aware of one’s emotions and to control them and express them effectively, with care and utilising empathy (Goleman et al., 2013). As explained by Quinn and Hoffe (2018) emotional intelligence is considered to be an important ability in nursing, not least due to the fact that care should be patient centred. If a person cannot manage their emotions or be empathic, it would be challenging to offer patient centred care, arguably.
As a nurse, I am well aware of the need for emotional intelligence in my interactions with others, whether colleagues, partners in the multidisciplinary team or patients. In the situation faced, I was overseeing the activities of a student nurse on placement. We were working with a female patient, Mrs B (patient’s name anonymised for confidentiality purposes) who had been hospitalised as a result of a suspected heart attack. Mrs B was being extremely rude to the student nurse who was trying to undertake basic checks of vital signs. The nurse was exhibiting signs of distress. I temporarily reassigned another nurse to take over the task, and took the student nurse, Ms G aside for a conversation to understand what was going on. It transpired that until that point, the nurse had only experienced grateful behaviour and fear from patients and had not had to handle a rude patient before.
I suggested to her that the patient was actually being rude because she was very frightened, and we discussed strategies for handling conversations with this type of patients.
Hire A Writer - Plagiarism-Free Essay Writing Service
Thoughts and Feelings
My initial thoughts and feelings around the situation were that the student nurse was acting ineffectively, but taking a quick step back from the scenario, I realised that actually she was doing her job and addressing the tasks assigned to her but struggling with emotional intelligence towards a verbally abusive patient. I was able to empathise with Ms G because I remembered being in a similar scenario in the early days of my care career. As argued by Prezerakos (2018) a review of the evidence suggests that emotional intelligence is critical to effective nursing care. My thoughts were initially happy and somewhat pleased with myself in being able to share helpful information based on experience with a more junior colleague. This feeling was quickly replaced by the realisation that emotional intelligence is not easy to manage on a personal level, and an acknowledgement that I have to continually work on this area in order to provide a supportive environment where quality and safe care can occur, per the requirements of the Nursing and Midwifery Council (2018) Code of practice.
The positive of this situation is in my emotional intelligence capabilities both with respect to Mrs B and Ms G, recognising that the patient was actually very frightened, and also acknowledging and dealing with the fact that Ms G was not seeing this and was taking the rude behaviour personally. Another positive was that while Ms G was visibly impacted by what was happening she did not let it affect the care that she was offering. It was not good that Ms G was responding in such a way as to be impacted, and not understanding that the patient was scared, and this can be seen as a negative. However, nurse leaders must be aware that not everyone that works in the field will have the same levels of emotional intelligence or capability to apply this even when experienced in the role. In addition, the emotional burden of nursing can be considerable and especially if nurses are facing other challenges with their resilience (Roussel, 2013).
Studies have been undertaken that indicate that emotional intelligence capabilities can have a positive impact on patient safety, such as that by Codier and Codier (2017). Examining the scenario that occurred, it is easy to see how a person that was less resilient than Ms G might have reacted differently to the rude behaviour, which could have compromised the safety of the patient. Bennett and Sawatzky (2013) outline how leaders in nursing must develop emotional intelligence in order to improve patient care. From analysing the situation in greater depth, as Beydler (2017) argues, nurse leaders that build up their own emotional intelligence abilities have can help others to improve theirs through acting in an emotionally intelligent and empathic manner towards their team. Indeed, as Roussel (2013, p. 61) argues, when moving into a leadership situation in nursing, the nursing leader must create “a supportive and positive work environment to help nurses cope with the stress of managing their own and others’ emotions concurrently.”
I like to think that this is what I do. However, looking back with hindsight, I know the incident with Mrs B and Ms G happened on a good day when I was energised, had a good night sleep and when we were not especially busy on the ward. There were staff to reassign to the specific role, and I was able to spend time with Ms G, coaching to help with her personal development. However, there are days when I am not as resilient, and the challenge lies in being able to be emotionally intelligent for myself, my team and the patients under my care on those days too. While I know that as Yoder-Wise et al. (2019) outlines that I must take care of my own resilience and I make every effort to do so, resilience is an attribute that depends on my own personal resources, as pointed out by Foster et al. (2020). There are days where I have lower levels of energy, where as a team we are stretched due to a lack of resources and being emotionally intelligent on those days is naturally harder.
Developing an environment where emotional intelligence can flourish can be concluded as being concerned with both developing emotional intelligence attributes in others, while not overlooking one’s own emotional intelligence capabilities. It is encouraging to be able to say that emotional intelligence can be impacted through training and development. There is no doubt that it can. However, one element that cannot be ignored with regard to time spent on training and personal development as a leader is the fact that there are barriers such as time constraints, in addition to the pressure of the job, and sometimes limited staffing levels as well (Mansel and Einion, 2019). Moreover, maintaining one’s own emotional intelligence on days that are particularly challenging personally is likely to be extremely difficult at times. Despite these challenges, personal development of both myself and others in this area is essential in the provision of safe and effective care and meeting the needs of the NMC (2018) Code.
Action Plan
One step that can be taken that I believe would be beneficial with respect to this type of scenario, is taking proactive measures to help in the development of emotional intelligence. This could be achieved perhaps through role play, as highlighted by Price and Harrington (2015). While it is acknowledged that there are times when this type of personal development opportunity would be difficult to enact with the team due to time pressures, there are also times when it could be possible to undertake this type of development. As Ellis (2018) also argues, coaching is an alternative form of personal development that can be utilised, acting as a supportive role model through working with more junior members of staff, questioning and encouraging their own reflection with regard to building the capability of emotional intelligence. However, clearly aside from helping shape emotional intelligence in others, there is a need for my effective self-management such that I can be highly emotionally intelligent at work and act as a role model for the expected and desired behaviours so that I can gain and maintain credibility as a leader. In achieving this, one step that I might take is being mindful about my own stress and fatigue levels and how these might impact on the working day. The Royal College of Nursing offers a healthy workplace toolkit which might prove helpful in this regard (2020).
Conflict Management
This reflection focuses on the issue of conflict management within the specific setting of the multidisciplinary team. It will again utilise the Gibbs reflective cycle for this purpose. As Taberna et al. (2020) explains, multidisciplinary teams are comprised of different professionals that come together to cooperate and collaborate in order to ensure that all aspects of a patient’s care are considered when addressing the service user’s needs.
Description of What Happened
Nurses have a number of roles to play as part of a multidisciplinary team. Pertino et al. (2014) outline some of these as ensuring that the patient receives effective care, adequate investigations, diagnosis and treatment, and managing and capturing data pertinent to the care as well. All professionals that are involved in multidisciplinary team work have the ability to offer value to making sure that the patient receives the optimal care with their needs met, which is argued to make a difference with regard to patient outcomes (Fitzpatrick and Kazer, 2011). As well as delivering improved outcomes, as Schober (2016) indicates, multidisciplinary teams have been an important component in recent health and social care policy due to their importance in ultimately lowering the costs of care through avoiding duplication and making sure that patient needs do not fall through the cracks between different care agencies.
Conflict is defined as being “A clash or a struggle that occurs when one’s balance among feelings, thoughts, desires and behaviour is threatened,” (Rigolosi, 2012, p. 213). In the particular scenario faced, I was part of a multidisciplinary team dealing working with a patient, Mr F (name anonymised to protect the patient’s confidentiality) with complex health and social care needs. In the process of meeting to examine and pinpoint the specific care needs for this individual and to ensure nothing was missed, I experienced a situation of conflict with one of the other professionals on the team, the social worker, Mrs P. The conflict arose due to the way in which we communicated with each of us misunderstanding what the other was saying. This led to the process not working as efficiently as it could. While it quickly became clear that both of us had the patient’s best interests central to what we were saying and trying to do, the conflict could have been avoided.
My initial reaction to Mrs P was one of anger, though I did not directly express this. However, I did demonstrate my frustration with how I responded to her, because from what she was saying, it made it sound as if she was unconcerned about how the patient’s ongoing care would be managed. The assumption that I made, based on the language used by Mrs P was also that she was asserting that we had not provided Mr F with adequate care, and this irritated me, as it felt like a direct attack on my professionalism and the care that I offer to patients. It also felt like an attack on my team, initially, and my immediate response was to step in and defend them. The reality was, as Huber (2014) reports sometimes can happen, the conflict initially seemed bigger and more insurmountable than it actually was, and the problem was primarily one of communication rather than misalignment in what we fundamentally thought. While this was a relief, it did not change the fact that my first response was of anger and frustration, rather than calmly taking steps to resolve the differences faced, and this is something that I need to work on in order to be a more effective nurse leader.
Evaluation of the Positives and Negatives
Examining the positives of the situation, the conflict between myself and Mrs P was resolved fairly quickly, which was good. Brinkert (2010) argues that it is important to be proactive when faced with conflict in order to manage it effectively, and the ways in which I did this included asking more questions of Mrs P and actively listening to her answers. I also paraphrased back to her my understanding of her meaning which was where the source of the conflict and the misinterpretation was pinpointed by her. However, as Borkowski and Meese (2020) indicate, conflict creates costs in healthcare. While in this case no harm was done, and ultimately myself and Mrs P have a better relationship as a result of clearing up our misunderstanding, some time was still wasted on the conflict, rather than on resolving the issue at hand. It might be considered that this created unnecessary costs. Managing my response so that it addressed the conflict more effectively in the first instance would have been more appropriate in this scenario.
The NMC (2018) Code requires that as a part of prioritising people, there is a need to work in a partnership to deliver effective care. Stanley (2016, p. 223) argues that, “Successful conflict management requires clinical leaders who demonstrate key conflict resolution principles,” and in addition to this, it is opined by Huber (2014) that it is best to work towards win-win resolutions in managing conflict effectively. Huber (2014) expresses the fact that when leaders work towards win-win scenarios they are more likely to focus on addressing problem solving. On reflection, my initial response was not working towards win-win with Mrs P. Thinking deeper about why this occurred, a factor compounding the communication challenges faced between myself and Mrs P was cultural difference between us, as Borkowski and Meese (2020) highlight can occur. Borkowski and Meese (2020) present evidence that in the healthcare environment, few employees realise the impact of cultural factors in leading to conflict between them, but this can indeed sometimes be the cause of conflict.
Conflict is likely on multidisciplinary teams for other reasons as well, not least due to the fact that everyone working on the team may have a slightly different agenda (Fulford et al., 2012). Looking at this in closer detail, on a very simplistic level, doctors may be focused on a curative solution while a physiotherapist may take a perspective of trying to prevent an issue from occurring again. While these sorts of differences may not seem that great, as Fulford et al. (2012) argue, different professional values can influence perspectives and communication and can lead to conflict. Instead of jumping to conclusions, as an effective nurse leader it would have been better to recognise the differences and identify a way to handle the conflict more appropriately as Murray (2017) outline is required. In particular, there is a need to focus on working towards shaping conflict towards positive outcomes.
Conflict is likely in any working environment and particularly in one as complex as a healthcare environment, but as outlined by Patton (2014). However, when conflict is dysfunctional and negative it can ultimately compromise patient care outcomes, and it also has the potential to detrimentally impact on job satisfaction and wellbeing of employees and colleagues (Patton, 2014). In terms of what else can be learned from this situation, reflecting on conflict from a wider perspective, clearly this can occur in a range of different ways, not just with people on the multidisciplinary team, but also with colleagues and team members, particularly where culture and personalities differ. The important aspect of conflict management to focus on is managing it for a constructive outcome, focusing on building good and solid working relationships with others, and ensuring the conflict is steered away from being damaging to relationships, and ultimately, even more importantly to patient outcomes.
It is also important to consider that conflict is likely to come about as part of the storming phase of team development as highlighted in the model of group development proposed by Tuckman (Harris and Roussel, 2010). As Harris and Roussel (2010) argue, resistance can occur during the storming phase when the group is working out how to work together, and interpersonal conflicts can occur during this time. While the Tuckman model is imperfect in that it suggests that the process of group development is linear only (Harris and Roussel, 2010), this storming element of group development is nonetheless important to keep in mind as a factor that can lead to conflict, which nurse leaders must manage.
With regard to addressing conflict, one step that is important in my action plan is working to better understand what people that I am working with are saying rather than jumping to incorrect conclusions and allowing myself to become frustrated. One of the ways that this might be best achieved which would have certainly helped in the scenario outlined, and potentially in other future situations to, is building up my cultural competence.
As outlined by Koutoukidis and Stainton (2020) having a good awareness of different cultures, and the beliefs, attitudes and values of those helps with nurses being able to develop better communication skills. Indeed, they argue that cultural sensitivity allows individuals to be more responsive with regard to the needs of people of different cultures (Koutoukidis and Stainton, 2020). This will also help me in selecting language to use that is less likely to provoke unnecessary conflict when working with people of different cultures and professional backgrounds.
Ashkanasy, N.M., Zerbe, W.J. and Hartel, C.E.J. (2016) Managing Emotions in the Workplace , Oxford: Routledge
Beydler, K.W. (2017) “The role of emotional intelligence in perioperative nursing and leadership: Developing skills for improved performance,” AORN Journal , 106 (4) 317-323
Bennett, K. and Sawatzky, J.A. (2013) “Building emotional intelligence: A strategy for emerging nurse leaders to reduce workplace bullying,” Nursing Administration Quarterly , 37 (2) 144-151
Borkowski, N. and Meese, K.A. (2020) Organisational Behaviour in Health Care , 4 th Edition, London: Jones & Bartlett Learning
Brinkert, R. (2010) “A literature review of conflict communication causes, costs, benefits and interventions in nursing,” Journal of Nursing Management , 18 (1) 145-56
Chang, E. and Daly, J. (2015) Transitions in Nursing , London: Elsevier Health Sciences
Codier, E. and Codier, D. (2017) “Could emotional intelligence make patients safer?” American Journal of Nursing, 117 (7) 58-62
Ellis, P. (2018) Leadership, Management and Team Working in Nursing , Exeter: Learning Matters
Fitzpatrick, J. and Kazer, M. (2011) Encyclopaedia of Nursing Research , New York: Springer
Foster, K., Marks, P., O’Brien, a. and Raeburn, T. (2020) Mental Health in Nursing , London: Elsevier Health Sciences
Fulford, K.W.M., Peile, E. and Carroll, H. (2012) Essential Values Based Practice , Cambridge: Cambridge University Press
Goleman, D., Boyatzis, R.E. and McKee, A. (2013) Primal Leadership: Unleashing the Power of Emotional Intelligence, Boston: Harvard Business Press
Harris, J. and Roussel, L. (2010) Clinical Nurse Leader Role, London: Jones & Bartlett Learning
Howatson-Jones, L. (2016) Reflective Practice in Nursing , Exeter: Learning Matters
Huber, D. (2014) Leadership and Nursing Care Management , London: Elsevier Health Sciences
Johns, C. (2017) Becoming a Reflective Practitioner , 5 th Edition, London: John Wiley & Sons
Koutoukidis, G. and Stainton, K. (2020) Tabbner’s Nursing Care , London: Elsevier Health Sciences
Mansel, B. and Einion, A. (2019) “It’s the relationship you develop with them: emotional intelligence in nurse leadership: a qualitative study,” British Journal of Nursing , 28 (21)
Murray, E. (2017) Nursing Leadership and Management , Philadelphia: F.A. Davis
NMC (2018) The Code , London: NMC
Patton, C. (2014) “Conflict in healthcare: A literature review,” The Internet Journal of Healthcare Administration , 9 (1) 1-11
Pertino, A., Gaino, R., Tartara, D. and Candeo, M.G. (2014) “Role of nurses in a multidisciplinary team for prevention, diagnosis, treatment and follow-up of osteonecrosis of jaw (ONJ),” Annali Di Stomatologia , 5 (2) 31-32
Prezerakos, P.E. (2018) “Nurse managers’ emotional intelligence and effective leadership: A review of the current evidence,” Open Nursing Journal , 12 (10 86-92
Price, B. and Harrington, A. (2015) Critical thinking and Writing for Nursing Students , Exeter; Learning Matters
Quinn, J.F. and Hoffe, S. (2018) The Importance of Emotional Intelligence in Healthcare , USA: ASTD
RCN (2019) “Stress and fatigue,” RCN, accessed 16/03/21: https://www.rcn.org.uk/clinical-topics/patient-safety-and-human-factors/professional-resources/stress-and-fatigue
Rigolosi, E.L.M. (2012) Management and Leadership in Nursing and Health Care , New York: Springer
Roussel, L. (2013) Management and Leadership for Nurse Administrators , London: Jones & Bartlett Learning
Schober, M. (2016) Introduction to Advanced Nursing Practice , New York: Springe
Stanley, D. (2016) Clinical Leadership in Nursing and Healthcare , London: John Wiley & Sons
Taberna, M., Moncayo, F.G., Jane-Salas, E., Antonio, M., Arribas, L., Vilajosana, E., Torres, E.P. and Mesia, R. (2020) “The multidisciplinary team (MDT) approach and quality of care,” Frontiers in Oncology, 10 (1) 85
Yoder-Wise, P.S., Waddell, J. and Walton, N. (2019) Leading and Managing in Canadian Nursing, London: Elsevier Health Sciences
- Share Share on Facebook
- Tweet Tweet on Twitter
- Pin it Pin on Pinterest
Leave a comment
Please note, comments must be approved before they are published
- Choosing a selection results in a full page refresh.
- Press the space key then arrow keys to make a selection.
What are your chances of acceptance?
Calculate for all schools, your chance of acceptance.
Your chancing factors
Extracurriculars.
Tips for Writing Your Nursing Program College Essays
This article was written based on the information and opinions presented by Giebien Na in a CollegeVine livestream. You can watch the full livestream for more info.
What’s Covered:
The importance of your college essays, general advice for writing your nursing essays.
If you know you want to be a nurse, you probably have quite a few reasons for that. Instead of merely relying on your academic and test performances to tell your story, you get the opportunity in your essays to share exactly why you’re so passionate about nursing. Writing about this can be a clarifying and even exciting process. This article explains why college application essays matter and how you should write about why you want to become a nurse.
Grades and test scores matter when you’re applying to college, but your essays can help improve your chances of admission. They’re how you can express your experiences and make your desire to become a nurse clear and personal.
If your prospective school doesn’t have supplemental essays, it’s a good idea to include your interest in nursing in your Common App essay . This could mean that you end up with two different drafts of the essay: one for if there are supplemental essays where you can discuss your interests in nursing and one for if there are not. You’ll change them out depending on whether you also have to respond to specific prompts about why you want to pursue nursing. This may not sound like much fun, but it will help you be admitted to your school of choice.
It might seem exciting to apply to a place where you don’t have to write extra essays—it’s less work! If you don’t do that additional work, though, you’ll have fewer chances to explain yourself. You might not be able to share exactly why you think that you’re the right fit for a certain college or program.
If you are writing supplemental essays for the colleges that you’re interested in, you can include more details about your passion for nursing. You’ll often be asked, “why this major?” or “why this school?” When you have those opportunities to share your specific reasons, you can let yourself get personal and go deep into your passion. Use that space to share important details about who you are.
Start Broad
When writing essays entirely about why you want to pursue nursing , try to start from a broad interest, then slowly work your way to telling specific personal stories and goals.
When first thinking about your general interest in nursing, ask yourself what attracts you to the work of being a nurse. This can lead to powerful potential responses. Maybe you like taking care of people in the community. Perhaps you’ve always known that you wanted to make a difference in the healthcare profession, but you don’t want to be a doctor. You’d rather make patients’ healthcare experiences as comfortable and pleasant as possible.
After you’ve described these broad, overarching motivations for wanting to go into nursing, consider any personal experiences that have made you want to be a nurse. Think about moments you’ve had during hospital visits or checkups or an anecdote from a time that you decided to volunteer in a healthcare role. Once you’ve written these stories, you can end the essay by discussing your planned major and career goals.
Discuss Your Future Goals
If you know what your end goal is, be sure to include it. You can write about becoming a registered nurse or maybe a nurse practitioner. It doesn’t have to be set in stone , but sharing a final ambition can help anchor your personal narrative. Writing about the future that you want can help the admissions officer reading your essay see how you view yourself. If they can do this, they’ll better understand your values and motivations and see you as a real candidate for their school.
You don’t have to follow this pattern exactly. For example, it can be powerful to begin your essay in the middle of the action—you can dive right into an anecdote and get the reader interested in your story from the jump.
While you should avoid dramatization, starting with a few clear, memorable scenes or a line or two of dialogue can make for an instantly interesting essay. All of this helps you show your passion, rather than simply explaining what intrigues you about a nursing career.
Once you’ve led with your narrative, though, remember to ground it in clear reasons for your intended career and what you want your future to look like. A good essay will be balanced between the past, present, and future. It’s how a college will see who you are and everything that you have to offer.
Related CollegeVine Blog Posts

How to Conduct a Nursing Head-to-Toe Assessment
This article has been reviewed by our panel of experienced registered nurses:
- Tyler Faust, MSN, RN
- Chaunie Brusie, BSN, RN
- Kathleen Gaines, MSN, RN, BA, CBC
What is a Head-to-Toe Assessment?
How to conduct a head-to-toe assessment.
- Head-to-Toe Assessment Order
- How to Prepare
- Equipment Checklist
How Long Are Head-to-Toe Assessments?

A head-to-toe assessment is a physical examination or health assessment, and it is one of the many important components of understanding a patient’s needs and problems. This assessment is performed during every shift and sometimes multiple times to determine if there have been any changes in your patient’s status.
We've put together a step-by-step guide to what happens in a nursing head-to-toe assessment and how nurses should understand the physical, emotional, and mental aspects of someone’s body systems.
Head-to-Toe Assessment Experts
We interviewed two healthcare experts to learn their best practices for conducting head-to-toe assessments. Terri Zucchero , PhD, RN, FNP-BC, is a nurse practitioner in Boston, and Angela Haynes Ferere, DNP, FNP-BC, MPH, serves as the DABSN Program Director at Nell Hodgson Woodruff School of Nursing at Emory University in Atlanta.
A head-to-toe assessment is an evaluation of all the body's systems to give you a picture of the patient's health needs and problems. “This baseline examination determines knowledge about patient health needs, current health status and patient goals for personal health outcomes, including health promotion and wellness counseling,” Zucchero says.
There are several types of assessments that can be performed:
1. Complete Health Assessment
A complete health assessment is a detailed examination that typically includes a thorough health history and a comprehensive head-to-toe physical exam. This type of assessment may be performed by registered nurses for patients admitted to the hospital or in community-based settings such as initial home visits. Advanced practice registered nurses (APRN) such as nurse practitioners (NP) also perform complete assessments when doing annual physical examinations.
2. Problem-Focused Assessment
A problem-focused assessment is an assessment based on certain care goals . For example, a nurse working in the ICU and a nurse that does maternal-child home visits have different patient populations and nursing care goals, she says. These assessments are generally focused on a specific body system such as respiratory or cardiac. While the entire body is important there is usually not enough time for a detailed full-body assessment.
Step 1: Establish Trust
When beginning an assessment, Zucchero says, “Establishing a personal relationship of trust and respect between the patient and the nurse is vital.” She adds that it is important throughout an assessment to assess how the patient is doing, and make sure they are properly draped and comfortable. You'll want to introduce yourself to the patient and explain the assessment process
Step 2: Confirm the patient’s ID
Step 3: note the patient's appearance and status.
“During an assessment, the first thing that should be noted is the patient’s overall appearance or general status,” Zucchero says. “This includes level of alertness, state of health/comfort/distress, and respiratory rate. This is done even prior to taking vital signs.”
Step 4: Assess the ABCs
Prior to starting a detailed assessment, you'll want to assess the ABCs - airway, breathing, and circulation.
Usually, the assessment begins with the least invasive to most invasive, allowing time for the patient to become more comfortable with the examiner. It also increases the likelihood that the examiner will not forget a system during the exam.
Step 5: Look for Abnormalities
Differentiating normal from abnormal is an important skill, Zucchero explains.
Some examples of major abnormal findings are changes in normal respiratory rate that indicates respiratory distress, or a change in skin color such as pallor that may indicate anemia or jaundice that typically indicates liver problems.
Generally, the human body is bilaterally symmetrical. When you are examining a patient, make note of any unusual asymmetry. If a patient is weaker on one side than another, or has a limited range of motion, or one side seems limper or otherwise different from the other side, there could be an underlying neurological or musculoskeletal issue.
The Order of a Head-to-Toe Assessment
|
|
|
|
| Assess pain using the appropriate pain scale for the patient |
|
| |
|
| |
|
|
|
|
| |
|
| |
|
| |
|
| |
|
| |
| score | |
|
|
How to Prepare for Head-to-Toe Assessments
“Like all clinical settings, standard precautions (formerly universal precautions) should always be practiced with each and every patient to protect both the nurse and patient,” states Zucchero. “The primary goal of standard precautions is to prevent the exchange of blood and body fluids and includes hand hygiene, use of personal protective equipment, and safe handling and cleaning of potentially contaminated equipment or surfaces.”
Techniques Used During Physical Assessment
There are four techniques utilized during a physical assessment including, inspection, palpation, percussion, and auscultation. It’s important to note that not all four techniques will be utilized during every assessment.
For example, APRNs will regularly palpate during an exam; however, a bedside med-surg nurse may not have a reason to. It is important that nursing students and nurses know each technique, how to utilize them, when to use them, and why they are important.
This is the first technique used in any assessment. You will want to fully inspect your patient before completing other aspects of the physical assessment. Utilize visual examination to inspect different areas of the body. You will want to note the overall appearance and color.
This is the act of touching a patient to determine abnormalities on or in the body. There are two different techniques used for palpation: light and deep palpation.
Light palpation is gentle and gives information about skin texture and moisture, fluids, muscle guarding, and some superficial tenderness the patient may be experiencing.
Deep palpation explores the internal structures of the body to a depth of four to five centimeters.
Nurses will palpate different body parts for sound vibrations. The most common is palpating the abdomen. Palpation can confirm the presence of air, fluid, and/or solids. It also is utilized to determine organ size, shape, and position.
Auscultation
The final method used during a physical assessment is auscultation, or listening with a stethoscope to the different body systems of your patient. You will want to listen for lung sounds, heart sounds, and bowel sounds. APRNs can also be expected to listen to the neck for bruits.
Head-to-Toe Assessment Equipment Checklist
Depending on the type of assessment conducted, the nurse may need specific equipment.
Basic equipment includes:
- Thermometer
- Blood pressure cuff
- Height wall ruler
- Tape measure,
- Stethoscope
Additional equipment for more comprehensive examinations would include,
- Ophthalmoscope
- Reflex hammer
- Tongue depressor
- Sterile sharp object (like toothpick or pin)
- Sterile soft object (like cotton ball)
- Something for the patient to smell (like an alcohol swab)
Ferere explains that the duration of the exam is directly correlated to the patient’s overall health status.
“Health patients with limited health histories may be completed in less than 30 minutes,” she says. “Many health practices have patients complete health history and pre-visit forms prior to presentation for a comprehensive visit. Review of these forms in advance can certainly reduce the required visit time.”
Find Nursing Programs
What 4 techniques are used in a head-to-toe assessment.
- The four techniques that are used for physical assessment are inspection, palpation, percussion, and auscultation.
How do you do a head-to-toe assessment?
- To perform a thorough head-to-toe assessment, it is recommended that you start with an overall inspection of the patient and then move to the head, ears, eyes, nose and throat. Then, move your way down the body systematically. You will need to include the four techniques of inspection, palpation, percussion, and auscultation throughout the assessment.
What is the purpose of a head-to-toe assessment?
- The purpose of a head-to-toe assessment is to get a baseline understanding of your patient. This assessment can be used in case there is an emergency or a change in their physical or emotional behavior. It also can be used to help diagnose a disease or illness.
What should the nurse begin by assessing when performing a head-to-toe assessment?
- This will depend on the patient. Typically, the first thing a nurse should do is look or inspect. Use your eyes to look at your patient’s skin, breathing, and outward appearance before moving on to more invasive aspects of the assessment. However, it is best to start at the head for a systematic top-to-bottom approach.
*This website is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

How to Write an Admission Essay for Nursing School

The nursing school admission process is rigorous. One of the critical requirements for new applicants is an application essay, and writing a compelling nursing essay will give you a major head start over other nursing school candidates.
Once you have figured out why you want to be a nurse, all your memories, accomplishments, ambitions, and goals will align. Therefore, writing an essay on why you are interested in becoming a nurse and selecting a specific nursing college or university allows the admissions team to understand why they should choose you over other candidates.
A well-written, organized, and polished nursing school essay automatically increases your chances of acceptance. With thousands of applications destined for assessment and judgment by the admissions committee, you would want to make your application essay for the nursing school admission stand out.
We have admission essay-writing experts and consultants who, luckily, have compiled this intensive guide to help you write an intentional, focused, and perfect essay for nursing school.
Note: If you are in a hurry or you need direct assistance in writing your nursing college essay, please place an order and let our expert essay writers craft for you an original, engaging, and compelling nursing essay!
What Is a Nursing School Essay?
A nursing school essay is a written piece that demonstrates your interest in a nursing career and elaborates why you are the perfect fit for a specific nursing program.
Most nursing schools (colleges and universities) require aspiring students to write an application essay for nursing school admission. It is a personal essay submitted as part of the application process, which the admission officers review to determine if you can be accepted.
A good nursing school essay shows your interest in the nursing field, your chosen career path, why you want to pursue your nursing education through a specific nursing school program, and why you believe you should be accepted into the institution. It has to show why the entire process is crucial to you and why you are a worthy candidate to select for the nursing school program.
Sometimes, it is the only hope one has left, especially if the competition is stiff. Imagine a situation where the application materials such as grades, resumes, test scores, or recommendation letters are all qualified; a nursing school essay will be the only means to select the best out of the rest fairly.
Writing a perfect nursing essay will demonstrate that you are ready to go down the thorny path of training to become a nurse. Nursing education entails research and writing assignments, and a well-written essay demonstrates your readiness.
Helpful Information to Include in a Nursing Admission Essay
You are probably wondering what goes into an application essay for nursing school admission. Well, your nursing essay will answer an essay prompt from the university. Most colleges will specify the essay questions for college of nursing applicants for various levels of study (MSN, DNP, BSN, Ph.D., or ADN).
Below are some examples of what might be expected:
- Your goals and ambitions for a successful nursing career
- How do you plan to achieve your academic goals
- The specific reasons why you want to join the nursing field
- Reasons you are selecting the particular nursing school or program
- Personal accomplishments that set you apart as the right candidate
- Experiences and encounters that make you love nursing career
- Plans for the future once accepted
- Experience with medical training or patient care
- Character traits aligned to being a nurse
- How you are prepared to become a successful nurse
- Academic, personal, and career interests
- Any other reasons to convince the admissions committee to approve your admission
In some quarters, a nursing school application essay might be a statement of purpose, personal essay, or letter of intent. It is a chance to plead with the admissions committee to accept you into your dream nursing college or program. Having looked at what goes into it, it is also essential to cover the steps to writing a perfect and comprehensive admission essay for nursing school.
Structure of a Nursing School Essay
A nursing essay for admission into a nursing program or school follows the typical format of an academic essay. It is organized into three main sections: introduction, body, and conclusion.
Introduction
- This is the opening paragraph that has to impress your readers (admissions officers)
- It can make or break your admission essay or personal statement
- It should be direct to the point
- It is a roadmap that helps the readers to know what to expect as your story grows.
- Open it using an enticing quote, event, anecdote, or statement
- You are allowed to use personal pronouns such as I in the introduction and the rest of the essay
- It has 2- 3 and sometimes five paragraphs
- Elaborates the introduction
- Every paragraph has a unique opening sentence that is a mini-thesis statement.
- Bears the best ideas yielded in your brainstorming session
- It can be as long as your word limit allows but contributes to at least 70-80% of the word count
- Focuses on quality over quantity
- Has one idea or experience per paragraph
- You should mention the skills you intend to develop and how they will help you become a successful nurse
- Connect the skills and experiences to the program and your future career
- Summarize and emphasize the main ideas
- It should be captivating and insightful
- Conveys a sense of closure to the readers
- Invites the readers to reflect on the ideas in your essay
- Creates one last lasting impression on the readers
Outline for a Nursing School Essay
A good nursing school essay outline should give you directions that help you visualize what the essay will look like in its final draft.
If you are writing a nursing essay, having the outline is the first thing you do after brainstorming (as shown in the steps).
It helps you to figure out how to arrange the ideas and points in the essay for a better flow. You can develop each section independently, regardless of the sequence, and still have a quality essay.
In most cases, the outline is meant for personal consumption, especially when writing a personal statement. However, if you are writing a nursing essay on a given nursing topic , you might be required to write an outline, annotated bibliography , and the nursing essay , and each will be graded separately.
Given the structure, you can outline your nursing school essay as follows:
Introduction paragraph
- Hook (quote, statement, or anecdote)
- Background information
- Thesis statement
- Transition sentence
Body paragraph 1
- Topic sentence
- Evidence, data, and facts
- Transition to the second body paragraph
Body paragraph 2
- Transition to the third body paragraph
Body paragraph 3
- Transition to the conclusion
Conclusion
- Summary of the main ideas
- Restate the thesis statement
- Last impression (call to action to the admissions committee)
Steps for Writing a Nursing School Essay
Optimizing your application essay increases your chance of getting accepted into the nursing program or nursing school. The essay should elaborate on your person (who you are as an individual) by providing a comprehensive perspective of your career ambitions, goals, and plans related to your passion for nursing. You should elaborate to the admissions committee why you are a good fit for their nursing program. Students at the ADN, BSN, ABSN (Accelerated BSN), MSN, DNP, or Ph.D. might be required to write an admission or personal essay, and here are the five steps to make it successful.
- Read the prompt
- Brainstorm for ideas
- Plan your essay
- Write the first draft
- Edit and Polish your Essay
Let's explore all these steps before delving into the tips to help you write the essay better.
Read the Prompt
If you are considering applying to a specific nursing school, you need to begin by researching the application process to know when you will be expected to submit your application essay.
In most cases, the nursing schools have essay prompts and instructions for the potential nursing candidates published on their websites. The prompts might vary depending on the programs you are interested in pursuing and the institutional preferences. Therefore, it is vital to begin by locating the nursing school essay guidelines. A quick search online can help, or you will also find it enclosed in the email sent to you by the school's admissions committee.
Read the instructions thoroughly with a specific focus on the essay question, word limit, and topics you must cover. If you apply to many nursing schools, you should locate and read each prompt before moving to the next steps.
Reading and understanding the instructions is the first step in writing an excellent application essay. Besides, it helps you to customize the essay to the requirements and not the other way around.
Brainstorm for Ideas
Now that you know what is expected of you, you need to decide what to include in your nursing essay to make it stand out. For this, get into an idea-generation marathon where you brainstorm ideas based on the prompt and the requirements.
Give every idea a thoughtful consideration and make shorthand notes so that you have all the ideas condensed. Consider your ambitions, accomplishments, drive, passion, preferences, strengths, weaknesses, character traits, and other attributes that might relate to your urge to pursue nursing as a career.
Also, research the nursing program and relate it to your personal ambitions and desires. Such information will help you spot the specific things you like about it. You can then tailor your experiences and encounters to the requirements. Look at the program's website and examine 2-3 aspects that stand out. This will help you focus on what you have that makes you the best pick for the program. You can also reference experiences, events, or traits related to the program.
Consider the environment and people around you and relate them to your desire to become a nurse.
Experiences, encounters, and events can inspire ideas to pen into your nursing school essay.
You can also research some well-written examples of nursing personal statements and essays to get inspired when brainstorming ideas for yours. Besides, you can also ask people in your network, such as family, friends, or peers, for ideas that can stand out and then choose the best.
To get the most robust ideas, rate them depending on how best they answer the prompt; this is the fodder for the entire application essay. Choose 3-5 strongest points and make them the central focus of your essay.
Plan your Essay
As a nurse, planning is everything, even when it comes to clinical decision-making. And because you are destined for this noble career, planning your personal essay won't hurt. Instead, it helps you know what to put and where to engage the admission officers from the beginning to the end of your nursing school essay.
With the ideas in mind, create a rough outline and adjust it until you are fully satisfied that your thoughts, facts, and opinions are well-organized. The outline will help you to structure your essay, avoid derailing it, and write a draft that bears all the quality ideas.
A good step is to organize the essay into paragraphs that align with the word count (often given as the minimum or maximum number of words, exact number of words, or characters).
Include an introduction to give your readers a clear understanding of the focus of your essay. Yes, a good nursing essay has a thesis statement that shows your central claim or the main idea you are focusing on the entire essay.
You should include the body paragraphs, each with a topic sentence supporting the thesis and a series of supporting facts such as examples, evidence, and illustration.
Finally, include a conclusion as the last paragraph that reverberates the thesis, summarizes the essay, and has a call to action to the admissions committee.
Write the First Draft
After the outline, you must begin writing your essay sentence by sentence and paragraph after paragraph. Whatever approach you take, ensure that every detail covered in the outline ends up in your essay as long as it is valid.
Write the introduction paragraph by giving a hook or attention grabber. You can begin with a quote from a famous nurse or a scholarly nursing article. You can also state facts or give statistics if they matter to your application. You should also elaborate on your selected topic, especially if the prompt provides options. End your first paragraph with a thesis statement that describes the focus of your nursing school essay. The introduction should account for 10-15% of the word count.
Each body paragraph has a unique, unmistakable, and concise topic sentence followed by supporting details and a concluding sentence that transitions to the next paragraph. Ensure that you have at least two body paragraphs considering that you can write either a three-paragraph or a five-paragraph nursing essay. Collectively, the body section should be 70-80% of the essay's word count. The body paragraphs should outline your encounters, experiences, and events and how they relate to the specific nursing program.
The final part is the conclusion, where you summarize the main ideas in the essay. for this, avoid the clich� conclusion starters such as "in conclusion," "to sum up," or "in summary." Instead, use conclusion opening sentences that demonstrate to your reader that the essay has ended � it gives the best closure and helps close the information loop in your essay. Rephrase your thesis and summarize the main ideas before appealing to the admissions committee to accept you into their nursing program. It should be 10-15% of the word count, like the introduction paragraph.
Edit and Polish the Essay
Now that you are done with your first draft, it is only the beginning, and you are far from being done. You need to take a break to cool down your frustrations, anxiety, and adrenaline developed when writing. It is a chance to establish an objective mind to look at things from a broader perspective when you settle for editing and proofreading.
If you are not good with editing and proofreading, you can hire a professional proofreading and editing expert to look at your essay and suggest changes to make. You can also use friends and family as a second and third eye to see what you cannot see. Using their feedback will help you optimize the essay for better results. You can incorporate the suggestions and proceed to editing and proofreading.
As for editing and proofreading, you can take advantage of tools such as Grammarly, Ginger, Hemingway Editor, and other editing and proofreading tools available by students and professionals. Revise the essay until it meets the requirements and addresses the prompt. If anything, do not be afraid to do away with an entire paragraph or a few paragraphs that don't make sense.
It is better to start over again than submit a subpar nursing school essay that will be a laughingstock of the admissions committee. The only way to entertain the admissions officers is to write an outstanding nursing school essay that will automatically dial you into the nursing program of your choice. Best of luck!
Example of Nursing School Essay Prompts
- Discuss your interest and understanding of the clinical nurse leader role. What's your story? And what experiences have contributed to your interest?
- The DNP program aims to prepare nurse leaders at the highest level of nursing practice to improve patient outcomes and translate research into practice. Describe experiences that exhibit your formal leadership role or informal leadership skills.
- How will the program help you achieve your academic and career goals?
- What experiences have influenced your interest in pursuing a clinical specialty you have chosen?
- The DNP program aims to prepare nurse leaders at the highest level of nursing practice to improve patient outcomes and translate research into practice. Describe experiences that exhibit your leadership skills.
- Why have you chosen to pursue a nursing research doctorate?
- How does becoming a nurse fulfill your ambitions?
- What does becoming a nurse mean to you?
- What drives you to become a nurse?
- Why do you want to become a nurse?
- What is your nursing philosophy?
- What was your reason for choosing nursing as a career? Do you have any additional information that you would like the admissions committee to know about you that has not been previously considered in the application?
- What are your professional goals? How will this accelerated nursing program help you materialize those goals?
- Discuss a specific leadership position (e.g., manager, director, associate dean) you wish to attain within three to five years after completing the DNP program.
Note: Some of these prompts have been rephrased from the Rush University Website . They keep changing depending on the preferences of the admissions committee. Inquire with your university or college of nursing to get specific directions on the most current prompts and instructions.
Related Reading: Ideas for a nursing capstone project.
Tips for Writing an Effective Nursing School Admission Essay
When grades, test scores, and other material entries don't count , a nursing school essay, referred to as a personal statement, suffices. In this case, a great nursing school can only be your hope for getting into nursing school. If you want to get ahead of the competition, these proven tips will significantly help you.
1. Plan Well
To pen an excellent nursing school essay that gets you accepted, you need to plan the essay.
Read the instructions, brainstorm as you take notes, research widely, and create an outline.
And even when done, the purpose is to have a reverse outline to help you score the essay against the requirements. Planning helps you to know what attention-grabbing statement to begin the essay with, the sequence of the body paragraph ideas for a logical flow, and what specifics to include in the conclusion.
Having an outline will help you save time when writing the first draft and help you to stay focused when writing.
2. Show, Don't Tell!
All effective nursing school essays express your personality, experiences, and encounters while convincing the admissions officers that you are the best fit for the program.
You should not focus on telling your story alone. Instead, show how your account relates to the prompt.
Discuss experiences, encounters, and events but show how they have impacted your choice of the program and desire to become a nurse.
If you are applying to a specific program, enlighten your readers on why you are specifically interested in the program and what that means.
It could be the hybrid learning model that entails both online and classroom learning or the history or reputation the school has, parental preferences (if they were a graduate), mentor recommendation, etc.
3. Choose Information Wisely
Ensure that every idea or information in your essay is unique, authentic, and original. Don't just write fictitiously.
If you have no past experiences directly related to nursing, you can introduce them and twist them to fit the context.
Impress the admissions committee with your wits, not just a summary of what others have written online.
Standing out in your presentation of facts will always carry the day. Genuinely share your story about what made you want to become a nurse.
4. Avoid Excuses
Even if you don't have appealing past encounters with medicine, hospitals, or anything related to nursing, tell your story as it is.
Do not excuse yourself for telling the truth. After all, you are on your journey to becoming a nurse; all you are seeking is training to develop the knowledge and skills.
If you have cared for your family members at home, babysat your siblings, or have compassion for the suffering, these are the most authentic stories you have, and they can spell meaning on your ambition. Therefore, prove your strong candidature by stating things as they are without clutching at things that do not matter.
5. Let it Flow!
Instead of forcing things such as humor or stories, write plainly about your experiences, encounters, and past events that made you want to become a nurse.
Most "why I want to be a nurse" essays don't have to have any humor. If it clicks well and is good, if it doesn't, don't force it.
As well, avoid exaggerating things when writing your nursing school essay. You should focus on making it as interesting, engaging, and convincing as can be but be truthful.
Avoid mixing up stories. A good way is to focus each paragraph on the main point that relates to your thesis.
6. Show you care about People and Yourself
Nursing is a noble career that entails caring for oneself as you care for others. Your full-time attention and job will be to care for people to help them achieve better health outcomes.
You must show empathy, selflessness, and determination to be a nurse. You can bring examples of when you took care of others and yourself.
Let the committee know that even when training as a nurse, you understand self-care as much as you understand caring for others.
7. Bring in Current Issues
If there is a chance that you can introduce nursing concepts or ideas from current events, it will beef up your nursing school essays.
Get facts from well-established nursing organization websites such as the American Nurses Association, National League of Nursing, Emergency Nurses Association, Sigma Theta Tau, or National Black Nurses Association, etc.
Intrigue your readers by understanding the challenges and opportunities in the nursing field.
You can relate your application to nursing shortages, medical errors, nursing burnout, continuing education, evidence-based practice, etc.
8. Briefly Explain your Qualifications
Since you have already provided material such as transcripts, resumes, and test scores, it is imperative to briefly expound on the qualifications without going into details. Tell them about your experiences, your education, and how you have set yourself up for success in nursing school . For instance, elaborate on how volunteering and internships helped you develop a sense of becoming a nurse or how they developed skills you will apply in nursing school.
9. Share your plans
Everybody has plans. You have short, medium, and long-term goals as you prepare to enter nursing school. You should include them in your essay and demonstrate how the program or school will help you achieve them. Admission officers are always wowed by hearing about goals, especially if they relate to their schools or programs. As you do this, be very specific with the goals and how you intend to achieve them.
All set, but before You Go �
As you contemplate entering nursing school, you must understand that it will never be a walk in the park. There is so much to learn within the specified time frame, and you must show your preparedness. A nursing school personal essay is one of the ways to do so.
Related Article:
- Writing a nursing philosophy ( a student's guide)
- Writing a nursing student resume (a guide)
Lucky for you, our nursing admission essay writers have shared insights, tips, and steps that can help you write an exceptional application essay for any nursing school or program. If you follow them, you will write a seamless admission essay that increases your chances of getting into the nursing school of your dreams.
We wish you luck in your endeavors and promise that were available in case you need a well-written, organized, and plagiarism-free admission essay tailored to your experiences and the specific nursing school or program requirements.
Struggling with
Related Articles

How to Write a Quality Improvement (QI) Report | An Ultimate Guide

iHuman Tips and Tricks for Success

Writing a Nursing Research Paper that Meets Professor's Requirements
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Home — Essay Samples — Education — Nursing Scholarship — Running Head: Nursing Care Study
Running Head: Nursing Care Study
- Categories: Nursing Scholarship
About this sample

Words: 2777 |
14 min read
Published: Jun 5, 2019
Words: 2777 | Pages: 6 | 14 min read
Table of contents
Patient and chart information, medical history and health assessment, chronological development of clients number one medical diagnosis, current signs and symptoms, textbook information, compare and contrast, systems review, head and neck, reproductive system, post menopausal, neurological, cranial nerves:.
- Optic nerve test not done due to client's inability to comply.
- Pupils constricted even in dim light, and do not constrict further as a result of test.
- Intact. Down and inward movement of eye observed.
- Intact. Muscles of mastication feel equally strong, bilaterally.
- Intact. Lateral movement of eye observed.
- Intact. Mobility and symmetry observed with movement of facial muscles with facial expressions observed.
- Could not hear whispered word test, tuning fork in Weber test, or tuning fork in Rinne test until tuning fork placed next to external auditory meatus, bilaterally.
- Uvula does not rise when client says "ahhh."
- Sternomastoid and trapezius muscles are equal in size bilaterally, with equal resistance to force applied to side of chin. Shoulders move equally in strength against resistance.
- Tongue protrudes midline with no tremors.
Integumentary
Medical and surgical history, social habits, family composition/family health problems, diet therapy, physical and cognitive ability, nursing diagnosis/problems/need, short-term goal, long-term goal, interventions.

Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Education

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 994 words
1 pages / 432 words
2 pages / 819 words
1 pages / 565 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nursing Scholarship
As I am approaching to conclude my current academic program, my wish is to proceed for further studies with a keen interest in healthcare administration. But that would depend if I happen to get a scholarship to pursue my [...]
Nursing is a profession that requires compassion, dedication, and a strong desire to help others. It is a field that demands both technical expertise and emotional intelligence. Throughout my academic and professional journey, I [...]
Nursing is a profession that requires continuous growth and development to provide the best care for patients. Setting and reflecting on goals is an essential part of this process, as it allows nurses to strive for excellence [...]
The article, “Longitudinal Association of Registered Nurse National Nursing Specialty Certification and Patient Falls in Acute Care Hospitals” from Nursing Research Journal, Volume 64, 2015, addresses quality of care and patient [...]
Education is a critical part in society in the current day and age. Many students pursue such important concepts for a brighter future. However, various obstacles exist, which potentially destroy the dreams of many talented [...]
My student status at JJc is that I' am a returning and part time student. I plan on staying at JJC for about two years to get my associates in Early Childhood Education, after i get my associates i would like to attend a 4 year [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Head-to-Toe Assessment: Complete Physical Assessment Guide

Assessment is the first and most critical phase of the nursing process . Incorrect nursing judgment arises from inadequate data collection and may adversely affect the remaining phases of the nursing process : diagnosis, planning, implementation , and evaluation . Get the complete picture of your patient’s health with this comprehensive head-to-toe physical assessment guide.
Table of Contents
What is head-to-toe assessment, 1. general appearance/survey, 2. chief complaint, 3. health history, 4. assessment of the integument, 5. assessment of the head and neck, 6. assessment of the eye and vision, 7. assessment of the ear, 8. assessment of the mouth, throat, nose, sinus, 9. assessment of the thoracic and lung, 10. assessment of the breast and lymphatic system, 11. assessment of the heart and neck vessels, 12. assessment of the peripheral vascular system, 13. assessment of the abdomen, 14. assessment of the female genitalia, 15. assessment of the male genitalia, 16. assessment of the anus, rectum, prostate, 17. assessment of the musculoskeletal system, 18. assessment of the neurologic system.
A head-to-toe assessment is a comprehensive physical assessment data collection method to gather patient data and determine the patient’s health status. It involves examining the entire body from head to toe in a systematic and thorough manner to identify health issues the patient may be experiencing.
At the end of the head-to-toe assessment, the nurse or healthcare provider should have gathered information that can help the patient’s treatment plan and have a clear understanding of the patient’s overall physical health and any potential issues that may need to be addressed.
For more information about assessment, please visit: The Nursing Process: A Comprehensive Guide .
Assessment Techniques
To make your head-to-toe assessment systematic, you need to know about the four basic assessment techniques. These techniques are inspection, palpation, percussion, and auscultation.
- Inspection involves using the senses of vision, smell , and hearing to observe and detect any normal or abnormal findings.
- Palpation consists of using parts of the hand to touch and feel for the following characteristics: texture, temperature, moisture, mobility , consistency, the strength of pulses, size, shape, and degree of tenderness.
- Percussion involves tapping body parts to produce sound waves. These sound waves or vibrations enable the examiner to assess underlying structures.
- Auscultation involves the use of a stethoscope to listen for heart sounds, movement of blood through the cardiovascular system , movement of the bowel , and movement of air through the respiratory tract.
Using COLDSPA mnemonic
The COLDSPA mnemonic is a useful memory aid for exploring each symptom of health concern.
| Character | Describe the sign or symptom (appearance, feeling, sound, smell, or taste) |
| Onset | When did it begin? |
| Location | Where is it? Does it radiate? Does it occur anywhere else? |
| Duration | How long does it last? Does it recur? |
| Severity | How bad is it? How much does it bother you? |
| Pattern | What makes it better or worse? |
| Associated factors | What other symptoms occur with it? How doe it affect you? |
History of Present Health Concerns
This section takes into account several aspects of the health problem and asks questions whose answers can provide a detailed description of the concern.
Past Health History
These are questions to elicit data related to the client’s past, strengths, and weaknesses in their health history.
Family Health History
- The family history should include as many generic relatives as the client can recall; in addition to genetic predisposition, it is also helpful to see other health problems that may have affected the client by virtue of having grown up in the family and being exposed to these problems.
Lifestyle and Health Practices
These questions are used to assess how the clients are managing their lives, their awareness of health, and unhealthy living patterns. These are usually open-ended questions to promote dialogue with the client.
Physical Assessment Guide
This section is where we’ll start the head-to-toe assessment. We’ll start with the general survey and identify the patient’s chief complaint, then the assessment of each body system.
NOTE: Remember to use the COLDSPA mnemonic (Character, Onset, Location, Duration, Severity, Patterns, and Associated Factors) to investigate and collect information for each symptom the client shares.
The general appearance or general survey is the first step in a head-to-toe assessment. The information gathered during the general survey provides clues about the overall health of the client. The general survey includes the overall impression of the client, mental status exam, and vital signs.
The chief complaint is the main reason why a client is seeking medical attention. It is the symptom or problem that is most concerning to the patient and is the focus of their visit. It is typically the first thing the healthcare provider asks about when seeing a patient, as it helps to provide context and background for the rest of the assessment and treatment.
The health history is an excellent way to begin the assessment process because it lays the groundwork for identifying nursing problems and provides a focus for the physical examination. The importance of health history lies in its ability to provide information that will assist the examiner in identifying areas of strength and limitation in the individual’s lifestyle and current health status.
The skin, hair , and nails are external structures that serve a variety of specialized functions. Diseases and disorders of the skin, hair, and nails can be local or they may be caused by an underlying systemic problem. To perform a complete and accurate assessment, the nurse needs to collect data about current symptoms, the client’s past and family history, and lifestyle and health practices.
History of present health concern
- Are you experiencing any current skin problems such as rashes, lesions, dryness, oiliness, drainage, bruising, swelling , or increased pigmentation? What aggravates the problem? What relieves it?
- Describe any birthmarks, tattoos, or moles, changes in their color, size, or shape.
- Have you noticed any change in your ability to feel pain , pressure, light touch, or temperature changes? Are you experiencing any pain , itching, tingling, or numbness?
Hair and Nails
- Have you had any hair loss or change in the condition of your hair? Describe.
- Have you had any change in the condition or appearance of your nails ? Describe.
Past health history
- Describe any previous problems with skin, hair, or nails, including any treatment or surgery and its effectiveness.
- Have you ever had any allergic skin reactions to food, medications, plants, or other environmental substances?
- Have you had a fever , nausea, vomiting , GI, or respiratory problems?
- For female clients: Are you pregnant? Are your menstrual periods regular?
Family history
- Has anyone in your family had a recent illness, rash, other skin problems, or allergy ? Describe.
- Has anyone in your family had skin cancer ?
Lifestyle and health practices
- Do you sunbathe? How much sun or tanning booth exposure do you get? What type of sun protection do you use?
- In your daily activities, are you regularly exposed to chemicals that may harm the skin?
- Do you spend long periods of time sitting or lying in one position?
- Have you had any exposure to extreme temperatures?
- What are your daily routine for skin, hair, and nail care?
- What kinds of foods do you consume in a typical day? How much fluid do you drink each day?
- Do skin problems limit any of your normal activities?
- Describe any skin disorder that prevents you from enjoying your relationships.
- How much stress do you have in your life? Describe.
- Do you perform a skin self-examination once a month?
Skin Physical Assessment
Physical assessment of the skin, hair, and nails provides the nurse with data that may reveal local or systemic problems.
Inspection of the skin
- Inspect general skin coloration. Keep in mind that the amount of pigment in the skin accounts for the intensity of color as well as hue.
- Inspect for color variations. Inspect localized parts of the body, noting any color variation.
- Check skin integrity . Especially carefully in pressure point areas (e.g. sacrum, hips, elbows); if any skin breakdown is noted use a scale to document the degree of skin breakdown.
- Inspect for lesions. Observe the skin surface to detect abnormalities; note color, shape, and size of lesion; if you suspect a fungus, shine a Wood’s light (an ultraviolet light filtered through a special glass) on the lesion.
Palpation of the skin
- Palpate skin to assess texture. Use the palmar surface of the three middle fingers to palpate skin texture.
- Palpate to assess thickness. If lesions are noted when assessing skin thickness, put gloves on and palpate the lesions between the thumb and finger; observe the drainage or other characteristics.
- Palpate to assess moisture. Check under skin folds and in unexposed areas.
- Palpate to assess temperature. Use the dorsal surfaces of the hands to palpate the skin.
- Palpate to assess mobility and turgor. Ask the client to lie down; using two fingers, gently pinch the skin on the sternum or under the clavicle.
- Palpate to detect edema . Use your thumbs to press down on the skin or the feet or ankles to check for edema .
Inspection and Palpation of the hair
- Inspect the scalp and hair. Have the client remove any hair clips, hair pins, or wigs, then inspect the scalp and hair for general color and condition.
- Inspect and palpate for cleanliness, dryness or oiliness, parasites, and lesions. At 1-inch intervals, separate the hair from the scalp and inspect and palpate the hair and scalp for cleanliness, dryness, or oiliness, parasites, and lesions; wear gloves if lesions are suspected or if hygiene is poor.
- Inspect the amount and distribution of scalp, body, axillae, and pubic hair. Look for unusual growth elsewhere in the body.
Inspection of the nails
- Inspect nail grooming and cleanliness. Normal findings would be the nails should be clean and manicured.
- Inspect nail color markings. Normal findings should be pink tones should be seen; some longitudinal ridging is normal.
- Inspect shape of nails. There is normally a 160-degree angle between the nail base and the skin.
Palpation of the nails
- Palpate nail to assess texture. Nails are hard and basically immobile.
- Palpate to assess texture and consistency. Note whether the nail plate is attached to the nailbed.
- Test capillary refill. Test capillary refill in nailbeds by pressing the nail tip briefly and watching for color change.
Head and neck assessment focuses on the cranium , face, thyroid gland, and lymph node structures contained within the head and neck.
- Do you experience neck pain ?
- Do you experience headaches? Describe.
- Do you have any facial pain? Describe.
- Do you have any difficulty moving your head or neck?
- Have you noticed any lumps or lesions on your head or neck that do not heal or disappear? Describe their appearance and location.
- Have you experienced any dizziness, lightheadedness, spinning sensation, or loss of consciousness? Describe.
- Have you noticed a change in the texture of your skin, hair, or nails?
- Have you noticed changes in your energy level, sleep habits, or emotional stability?
- Have you experienced any palpitations, blurred vision, or changes in bowel habits?
- This portion of the health history focuses on questions related to the client’s past, from the earliest beginnings to the present.
- Describe any previous head or neck problems you have had. How were they treated? What were the results?
- Have you ever undergone radiation therapy for a problem in your neck region?
- Is there a history of head and neck cancer in your family?
- Is there a history of migraine headaches in your family?
This is a very important section of the health history because it deals with the client’s human responses.
- Do you smoke or chew tobacco? If yes, how much?
- Do you wear a helmet when riding a horse, bicycle, motorcycle, or other open sports vehicle? Do you wear a hard hat for hazardous occupations?
- What is your typical posture when relaxing, during sleep , and when working?
- In what kinds of recreational activities do you participate? Describe the activity.
- Have any problems with your head or neck interfered with your relationships with others or the role you occupy at home or at work?
Head and Face
- Inspect the head. Inspect for size, shape, and configuration.
- Inspect for involuntary movement. Head should be held still and upright.
- Inspect the face. Inspect for symmetry, features, movement, expression, and skin condition.
- Palpate the head. Palpate for consistency; the head is normally hard and smooth without lesions.
- Palpate the temporal artery. This should be located between the top of the ear and the eye.
- Palpate the temporomandibular joint. To assess the temporomandibular joint, place your index finger over the front of each ear as you ask the client to open your mouth .
- Inspect the neck. Observe the client’s slightly extended neck for position, symmetry, and lumps or masses. Shine a light from the side of the neck across to highlight any swelling.
- Inspect the movement of the neck structures. Ask the client to swallow a small sip of water. Observe the movement of the thyroid cartilage and thyroid gland.
- Inspect the cervical vertebrae. Ask the client to flex the neck (chin to chest, ear to shoulder, twist left to right and right to left, and backward and forward.
- Inspect range of motion. Ask the client to turn the head to the right and to the left (chin to shoulder), touch each ear to the shoulder, touch chin to chest, and lift the chin to the ceiling.
- Palpate the trachea . Place your finger in the sternal notch. Feel each side of the notch and palpate the tracheal rings. The first upper ring above the smooth tracheal rings is the cricoid cartilage.
- Palpate the thyroid gland. Locate key landmarks with your index finger and thumb; ask the client to swallow as you palpate
Auscultation
- Auscultate the thyroid gland only if you find an enlarged thyroid gland during inspection or palpation. Place the bell of the stethoscope over the lateral lobes of the thyroid gland; ask the client to hold his breath (to obscure any tracheal breath sounds while you auscultate).
Lymph nodes of the head and neck
- Palpate the preauricular nodes, postauricular nodes, occipital nodes. There should be no swelling or enlargement and no tenderness.
- Palpate the tonsillar nodes. Palpate the tonsillar nodes at the angle of the mandible on the anterior edge of the sternomastoid muscle .
- Palpate the submental nodes , which are a few centimeters behind the tip of the mandible.
- Palpate the superficial cervical nodes in the area superficial to the sternomastoid muscle.
- Palpate the posterior cervical nodes in the area posterior to the sternomastoid and anterior to the trapezius in the posterior triangle.
- Palpate the deep cervical chain nodes deeply within and around the sternomastoid muscle.
- Palpate the supraclavicular nodes by hooking your fingers over the clavicles and feeling deeply between the clavicles and sternomastoid muscles.
To perform a thorough assessment of the eye, one needs a good understanding of the external structures of the eye, the internal structures of the eye, the visual fields and pathways, and the visual reflexes.
When interviewing a client about eye health and vision, remember to investigate and analyze any reported symptoms or signs further.
Visual Problems
- Describe any recent changes in your vision. Were they sudden or gradual?
- Do you see spots or floaters in front of your eyes?
- Do you experience blind spots? Are they constant or intermittent?
- Do you see halos or rings around lights?
- Do you have trouble seeing at night?
- Do you experience double vision?
- Do you have any eye pain or itching? Describe.
- Do you have any redness or swelling in your eyes?
- Do you experience excessive watering or tearing of the eye? One eye or both eyes?
- Have you had any eye discharge? Describe.
- Have you ever had problems with your eyes or vision?
- Have you ever had eye surgery?
- Describe any past treatments you have received for eye problems. Were these successful? Were you satisfied?
- Is there a history of eye problems or vision loss in your family?
- Are you exposed to conditions or substances in the workplace or home that may harm your eyes or vision? Do you wear safety glasses during exposure to harmful substances?
- Do you wear sunglasses during exposure to the sun?
- What types of medication do you take?
- Has your vision loss affected your ability to care for yourself? To work?
- When was your last eye examination?
- Do you have a prescription for corrective lenses? Do you wear them regularly? If you wear contacts, how long do you wear them? How do you clean them?
Evaluation of Vision
- Test distant visual acuity. Position the client 20 feet from the Snellen or E chart and ask her to read each line until she cannot decipher the letters or their direction.
- Test near visual acuity. Use this test for middle-aged clients and others who complain of difficulty reading. Give the client a hand-held vision chart to hold 14 inches from the eyes. Have the client cover one eye with an opaque card before reading from top to bottom.
- Test visual fields for gross peripheral vision. To perform the confrontation test, position yourself approximately 2 feet away from the client at eye level. Have the client cover his left eye while you cover your right eye. Look directly at each other with your uncovered eyes. Next fully extend your left arm at midline and slowly move one finger upward from below until the client sees your finger.
External eye structures
Inspection and Palpation
- Inspect the eyelids and eyelashes. Note the width and position of palpebral fissures. Assess the ability of eyelids to close. Note the position of the eyelids in comparison with the eyeballs. Observe for redness, swelling, discharge, or lesions.
- Observe the position and alignment of the eyeball in the eye socket. Eyeballs are symmetrically aligned in sockets without protruding or sinking.
- Inspect the bulbar conjunctiva and sclera . Have the client keep her head straight while looking from side to side and then up toward the ceiling. Observe clarity, color, and texture.
- Inspect the palpebral conjunctiva. Put on gloves for this assessment procedure. First, inspect the palpebral conjunctiva of the lower eyelid by placing your thumbs bilaterally at the level of the lower bony orbital rim and gently pulling down to expose the palpebral conjunctiva.
- Inspect the lacrimal apparatus . Assess the areas over the lacrimal glands (lateral aspect of upper eyelid) and the puncta (medial aspect of lower eyelid).
- Inspect the cornea and lens. Shine a light from the side of the eye for an oblique view. Look through the pupil to inspect the lens.
- Test pupillary reaction to light. Test for direct response by darkening the room and asking the client to focus on a distant object.
- Test accommodation of pupils. Hold your finger or a pencil about 12 to 15 inches from the client. Ask the client to focus on your finger or pencil and to remain focused on it as you move it closer toward the eyes.
- Palpate the lacrimal apparatus. Put on disposable gloves to palpate the nasolacrimal duct to assess for blockage. Use one finger and palpate just inside the lower orbital rim.
Internal eye structures
- Inspect the optic disc. Keep the light beam focused on the pupil and move closer to the client from a 15-degree angle. You should be very close to the client’s eye (about 3 to 5 cm), almost touching the eyelashes. Note the shape, color, size, and physiologic cup.
- Inspect the retinal vessels. Remain in the same position as described previously. Inspect the sets of retinal vessels by following them out to the periphery of each section of the eye. Note the number of sets of arterioles and venules.
- Inspect retinal background. Remain in the same position described previously and search the retinal background from the disc to the macula, noting the color and the presence of any lesions.
- Inspect the fovea (sharpest area of vision) and macula. Remain in the same position described previously. Shine the light beam toward the side of the eye or ask the client to look directly into the light. Observe the fovea and the macula that surrounds it.
- Inspect the anterior chamber. Remain in the same position and rotate the lens wheel slowly to +10, +12, or higher to inspect the anterior chamber of the eye.
Beginning when the nurse first meets the client, the assessment of hearing provides important information about the client’s ability to interact with the environment.
- If the client complains of or reports a history of ear infections or suspects hearing loss, collect as much related data as possible.
Changes in Hearing
- Describe any recent changes in your hearing.
- Are all sounds affected by this change, or just some sounds?
Other Symptoms
- Do you have any ear drainage? Describe the amount and any odor.
- Do you have any ear pain? If so, do you have an accompanying sore throat , sinus infection , or problem with your teeth or gums?
- Do you experience any ringing or crackling in your ears?
- Do you ever feel like you are spinning or that the room is spinning? Do you ever feel dizzy or unbalanced?
- Have you ever had any problems with your ears such as infections, trauma, or earaches?
- Describe any past treatments you have received for ear problems. Were these successful? Were you satisfied?
- Is there a history of hearing loss in your family?
- Do you work or live in an area with frequent or continuous loud noise? How do you protect your ears from the noise?
- Do you spend a lot of time swimming or in the water? How do you protect your ears?
- Has your hearing loss affected your ability to care for yourself? To work?
- Has your hearing loss affected your socializing with others?
- When was your last hearing examination?
- How do you care for your ears?
External ear structures
- Inspect the auricle , tragus, and lobule. Note size, shape, and position. Observe for lesions. discolorations, and discharge.
- Palpate the auricle and mastoid process. Normally the auricle, tragus, and mastoid process are not tender.
Internal ear structures
- Inspect the external auditory canal. Use the otoscope. A small amount of odorless cerumen is the only discharge normally present.
- Inspect the tympanic membrane (eardrum). Note color, shape, consistency, and landmarks.
- Perform Weber’s test if the client reports diminished or lost hearing in one ear. Strike a tuning fork softly with the back of your hand and place it in the center of the client’s head or forehead. Ask whether the client hears the sound better in one ear or the same in both ears.
- Perform the Rinne test. The Rinne test compares air and bone conduction. Strike a tuning fork and place the base of the fork on the client’s mastoid process. Ask the client to tell you when the sound is no longer heard. Move the prongs of the tuning fork to the front of the external auditory canal. Ask the client to tell you if the sound is audible after the fork is moved.
- Perform the Romberg test. Ask the client to stand with feet together and arms at the sides and eyes open and then with eyes closed.
Subjective data related to the mouth, throat, nose, and sinus can aid in detecting diseases and abnormalities that may affect the client’s activities of daily living .
Tongue and Mouth
- Do you experience tongue or mouth sores or lesions? Are they painful? How long have you had them? Do they recur? Is it single, or do you have many?
- Do you experience redness, swelling, bleeding , or pain in the gums or mouth? How long has this been happening? Do you have any toothache? Have you lost any permanent teeth?
Nose and Sinuses
- Do you have pain in your sinuses?
- Do you experience any nosebleeds? How much bleeding ? What color is the blood?
- Do you experience frequent clear or mucous drainage from your nose?
- Can you breathe through both of your nostrils? Do you have a stuffy nose at times during the day or night?
- Do you have seasonal allergies? Describe the timing of the allergies and symptoms.
- Have you experienced a change in your ability to smell or taste?
- Do you have difficulty chewing or swallowing food? How long have you had this? Do you have any pain?
- Do you have a sore throat? How long have you had it? Describe. How often do you get sore throats?
- Do you experience hoarseness ? How long?
- Have you ever had any oral, nasal, or sinus surgery? Do you have a history of sinus infections? Describe your symptoms. Do you use nasal sprays?
- Is there a history of mouth, throat, nose, or sinus cancer in your family?
- Do you smoke or use smokeless tobacco? If so, how much? Are you interested in quitting this habit?
- Do you drink alcohol? How much and how often?
- Do you grind your teeth?
- Describe how you care for your teeth or dentures. How often do you brush and use dental floss? When was your last dental examination?
- If the client wears braces: How do you care for your braces? Do you avoid any specific types of foods? Describe your usual dietary intake for a day.
- If the client wears dentures: How do your dentures fit?
- Do you brush your tongue?
- How often are you in the sun? Do you use lip sunscreen products?
- Inspect the lips. Observe lip consistency and color.
- Inspect the teeth and gums. Ask the client to open their mouth. Note the number, color, condition, and alignment of the teeth.
- Inspect the buccal mucosa. Use a penlight and tongue depressor to retract the lips and cheeks to check color and consistency. Also, note Stenson’s ducts (parotid ducts) located on the buccal mucosa across from the second upper molars.
- Inspect and palpate the tongue. Ask the client to stick out the tongue. Inspect for color, moisture, size, and texture. Observe for fasciculations (fine tremors), and check for midline protrusions. Palpate any lesions present for induration.
- Assess the ventral surface of the tongue. Ask the client to touch the tongue to the roof of the mouth, and use a penlight to inspect the ventral surface of the tongue.
- Inspect for Wharton’s ducts. These are openings from the submandibular salivary glands located on either side of the frenulum on the floor of the mouth.
- Observe the sides of the tongue. Use a square gauze pad to hold the client’s tongue to each side. Palpate for any lesions, ulcers, or nodules for induration.
- Check the strength of the tongue. Place your fingers on the external surface of the client’s cheek. Ask the client to press the tongue’s tip against the inside of the cheek to resist pressure from your fingers.
- Check the anterior tongue’s ability to taste by placing drops of sugar and salty water on the tip and sides of the tongue with a tongue depressor.
- Inspect the hard (anterior) and soft (posterior) palates and uvula. Ask the client to open the mouth wide while you use a penlight to look at the roof. Observe color and integrity.
- Note odor . While the mouth is wide open, note any unusual or foul odor.
- Assess the uvula. Apply a tongue depressor to the tongue and shine a penlight into the client’s wide-open mouth. Note the characteristics and positioning of the uvula. Ask the client to say “Aaah” and watch for the uvula and soft palate to move.
- Inspect the tonsils . Using the tongue depressor to keep the mouth open wide, Inspect the tonsils for color, size, and presence of exudate or lesions. Tonsils should be graded.
- Inspect the posterior pharyngeal wall. Keeping the tongue depressor in place, shine the penlight on the back of the throat. Observe the color of the throat, and note any exudate or lesions.
- Inspect and palpate the external nose. Note nasal color, shape, consistency, and tenderness.
- Check the patency of airflow through the nostrils by occluding one nostril at a time and asking the client to sniff.
- Inspect the internal nose. To inspect the internal nose, use an otoscope with a short wide-tip attachment. Use your non-dominant hand to stabilize and gently tilt the client’s head back. Insert the short wide tip of the otoscope into the client’s nostril without touching the sensitive nasal septum.
- Palpate the sinuses. Palpate the frontal sinuses by using your thumbs to press up on the brow on each side of the nose. Palpate the maxillary sinuses by pressing with thumbs up on the maxillary sinuses.
- Percuss the sinuses. Lightly tap over the frontal sinuses and over the maxillary sinuses for tenderness.
Transillumination
- Transilluminate the sinuses . Transilluminate the frontal sinuses by holding a strong, narrow light source snugly under the eyebrows. Use your other hand to shield the light. Transilluminate the maxillary sinuses by holding a strong, narrow light source over the maxillary sinus and asking the client to open his or her mouth.
Subjective data related to the thoracic and lung assessment provide many clues about underlying respiratory problems and associated nursing diagnoses , as well as clues about the risk for the development of lung disorders.
Difficulty of breathing
- Do you ever experience difficulty breathing? Describe the difficulty.
- Do you experience any other symptoms when you have difficulty breathing?
- Do you have difficulty breathing when resting, or do any specific activities cause the difficulty?
- Do you have difficulty breathing when you sleep ? Do you use more than one pillow or elevate the head of the bed when you sleep ?
- Do you snore when you sleep ? Have you been told that you stop breathing at night when you snore?
- Do you have chest pain ? Is the pain associated with a cold, fever, or deep breathing ?
- Do you have a cough? When and how often does it occur?
- Do you produce any sputum when you cough? If so, what color is the sputum? How much sputum do you cough up? Has this amount increased or decreased recently? Does the sputum have an odor?
- Do you wheeze when you cough or when you are active?
GI symptoms
- Do you have gastrointestinal symptoms such as heartburn, frequent hiccups, or chronic cough?
- Have you had prior respiratory problems?
- Have you ever had any thoracic surgery, biopsy , or trauma?
- Have you been tested for or diagnosed with allergies?
- Have you ever had a chest x-ray, tuberculosis (TB) skin test, or influenza immunization? Have you had any other pulmonary studies in the past?
- Have you recently traveled outside of the country? Have you been in close contact with anyone known or suspected to have SARS ?
- Is there a history of lung disease in your family?
- Did any family members in your home smoke when you were growing up?
- Is there a history of other pulmonary illnesses/disorders in the family?
- Have you ever smoked cigarettes or other tobacco products? Do you currently smoke? At what age did you start? How much do you smoke, and how much have you smoked in the past? What activities do you usually associate with smoking? Have you ever tried to quit?
- Are you exposed to any environmental conditions that affect your breathing? Where do you work? Are you around smokers?
- Do you have difficulty performing your usual daily activities? Describe any difficulties.
- What kind of stress are you experiencing at this time? How does it affect your breathing?
- Are you currently taking medications for breathing problems or other medications that affect your breathing? Do you use any other treatments at home for your respiratory problems?
- Have you used any herbal medicines or alternative therapies to manage colds or other respiratory problems?
Posterior thorax
- Inspect for nasal flaring and pursed lip breathing. Nasal flaring is not observed in normal findings.
- Observe the color of the face, lips, and chest. The client has an evenly colored skin tone without unusual or prominent discoloration.
- Inspect the color and shape of the nails. Pink tones should be seen in the nailbeds. There is normally a 160-degree angle between the nail base and the skin.
- Inspect configuration. While the client sits with her arms at her sides, stand behind her and observe the position of the scapulae and the shape and configuration of the chest wall.
- Observe the use of accessory muscles. Watch as the client breathes and does not use it.
- Inspect the client’s positioning. Note the client’s posture and ability to support weight while breathing comfortably.
- Palpate for tenderness and sensation. Palpation may be performed with one or both hands; however, the sequence of palpation is established. Start toward the midline at the level of the left scapula and move your hand from left to right, comparing findings bilaterally. Move systematically downward and out to cover the lateral portions of the lungs at the bases.
- Palpate for crepitus. Crepitus, also called subcutaneous emphysema , is a crackling sensation that occurs when air passes through fluid or exudate. Use your fingers and follow the above sequence when palpating.
- Palpate surface characteristics. Use gloves and your fingers to palpate any lesions you noticed during the inspection.
- Palpate for fremitus. Following the above sequence, use the ball or ulnar edge of one hand to assess for fremitus (vibrations of air in the bronchial tubes transmitted to the chest wall.
- Assess chest expansion. Place your hands on the posterior chest wall with your thumbs at the level of T9 or T10 and press together a small skin fold.
- Percuss for tone. Start at the apices of the scapulae and percuss across the tops of both shoulders. Then percuss the intercostal spaces across and down, comparing sides. Percuss the lateral aspects at the bases of the lungs, comparing sides.
- Percuss for diaphragmatic excursion. Ask the client to exhale forcefully and hold their breath. Beginning at the scapular line, percuss the intercostal spaces of the right posterior chest wall. Percuss downward until the tone changes from resonance to dullness. Next, ask the client to inhale deeply and hold it. Percuss the intercostal spaces from the mark downward until resonance changes to dullness.
- Auscultate for breath sounds. To begin, place the diaphragm of the stethoscope firmly and directly on the posterior chest wall at the apex of the lung at C7. Ask the client to breathe deeply through his or her mouth for each area of auscultation in the auscultation sequence so you can best hear inspiratory and expiratory sounds.
- Auscultate for adventitious sounds. Adventitious sounds are sounds added or superimposed over normal breath sounds and heard during auscultation.
- Auscultate voice sounds. Bronchophony: Ask the client to repeat the phrase “ninety-nine” while you auscultate the chest wall.
Other Assessment Techniques
- Egophony: Ask the client to repeat the letter E while you listen over the chest wall.
- Whispered Pectoriloquy: Ask the client to whisper the phrase “one-two-three” while you auscultate the chest wall.
Anterior thorax
- Inspect for shape and configuration. Have the client sit with her arms at her sides. Stand in front of the client and assess shape and configuration.
- Inspect the position of the sternum. Observe the sternum from an anterior and lateral viewpoint. Watch for sternal retraction.
- Inspect the slope of the ribs. Assess the ribs from an anterior and lateral viewpoint.
- Observe the quality and pattern of respiration. Note breathing characteristics as well as rate, rhythm, and depth.
- Inspect intercostal spaces. Ask the client to breathe normally and observe the intercostal spaces.
- Observe for use of accessory muscles. Ask the client to breathe normally and observe for use of accessory muscles.
- Palpate for tenderness, sensation, and surface masses. Use your fingers to palpate for tenderness and sensation. Start with your hand positioned over the left clavicle and move your hand left to right, comparing findings bilaterally. Move your hand systematically downward toward the midline at the level of the breasts and outward at the base to include the lateral aspect of the lung.
- Palpate for fremitus. Using the sequence for the anterior chest above, palpate for fremitus using the same technique as for the posterior thorax.
- Palpate anterior chest expansion. Place your hands on the client’s anterolateral wall with your thumbs along the costal margins and pointing toward the xiphoid process.
- Percuss for tone. Percuss the apices above the clavicles. Then percuss the intercostal spaces across and down, comparing sides.
- Auscultate for anterior breath sounds, adventitious breath sounds, and voice sounds. Place the diaphragm of the stethoscope firmly and directly on the anterior chest wall. Auscultate from the apices of the lungs slightly above the clavicles to the bases of the lungs at the sixth rib. Listen at each site for at least one respiratory cycle. Follow the sequence for anterior auscultation.
This chapter covers the examination of non-pregnant women’s breasts. Remember, if the client reports any symptoms, you need to explore further by performing a symptom analysis using the following guide.
- Have you noticed any lumps or swelling in your breasts? If so, where? when did you first notice? has the lump grown or has the swelling increased? Is the lump or swelling associated with other problems? Does the lump or swelling change during your menstrual cycle ?
- Have you noticed any lumps or swelling in the underarm area?
- Have you noticed any redness, warmth, or dimpling of your breasts? Any rash on the breast, nipple, or axillary area?
- Have you noticed any change in the size or firmness of your breasts?
- Do you experience any pain in your breasts? If so, where? Does it occur at any specific time during your menstrual cycle?
- is there a certain activity that seems to initiate the pain?
- Do you have any discharge from the nipples? If so, describe its color, consistency, and odor, if any. When did it start? Which nipple has the discharge?
- Have you had any prior breast disease? Have you ever had breast surgery, a breast biopsy, breast implants, or breast trauma? If so, when did this occur? What was the result?
- How old were you when you began to menstruate? Have you experienced menopause ?
- Have you given birth to any children? At what age did you have your first child?
- When was the first and last day of your menstrual cycle?
- Is there a history of breast cancer in your family? Who?
- Are you taking any hormones, contraceptives, or antipsychotic agents?
- Do you live or work in an area where you have excessive exposure to radiation, benzene, or asbestos?
- What is your typical daily diet?
- How much alcohol do you drink each day?
- How much coffee, tea, and cola do you consume each day?
- Do you engage in any regular exercise? If so, what type of bra do you wear when you exercise?
- How important are your breasts to you in relation to a positive feeling about yourself and your physical appearance? Do you have any fears regarding breast disease?
- Do you examine your own breasts? Describe when you do this. Have you noted any changes in your breasts such as a lump, swelling, skin irritation, or dimpling, nipple pain or retraction, redness or scaliness or nipple of breast skin, or discharge? If yes, have you reported this to your healthcare provider?
- Have you ever had your breasts examined by a physician? When was your last examination?
- Have you ever had a mammogram ? If so, when was your last one?
Female breasts
- Inspect size and symmetry. Have the client disrobe and sit with arms hanging freely. Explain what you are observing to help ease client anxiety .
- Inspect color and texture. Be sure to note the client’s overall skin tone when inspecting the breast skin. Note any lesions.
- Inspect superficial venous pattern. Observe the visibility and pattern of breast veins.
- Inspect the areolas. Note the color, size, shape, and texture of the areolas of both breasts.
- Inspect the nipples. Note the size and direction of the nipples of both breasts. Also note any dryness, lesions, bleeding, or discharge.
- Inspect for retraction and dimpling. To inspect the breasts accurately for retraction and dimpling, ask the client to remain seated while performing several different maneuvers. Ask the client to raise her arms overhead, then press her hands against her hips. Next, ask her to press her hands together.
- Palpate texture and elasticity. Smooth, firm, elastic tissue is a normal finding.
- Palpate tenderness and temperature. A generalized increase in nodularity and tenderness may be a normal finding associated with the menstrual cycle or hormonal medications.
- Palpate for masses . Note location, size in centimeters, shape, mobility, consistency, and tenderness. Also, note the condition of the skin over the mass.
- Palpate the nipples. Wear gloves to compress the nipple gently with your thumb and index finger. Note any discharge.
- Palpate mastectomy or lumpectomy site. If the client has had a mastectomy or lumpectomy, it is still important to perform a thorough examination. Palpate the scar and any remaining breast and axillary tissue for redness, lesions, lumps, swelling, or tenderness.
- Inspect and palpate the axillae. Ask the client to sit up. Inspect the axillary skin for rashes or infections. Hold the client’s elbow with one hand, and use the three fingerpads of your other hand to palpate firmly the axillary lymph nodes . First, palpate high into the axillae, moving downward against the ribs to feel for the central nodes. Continue to move down the posterior axillae to feel for the posterior nodes.
Male breasts
- Inspect and palpate the breasts, areolas, nipples, and axillae. Note any swelling, nodules, or ulceration. Palpate the flat disc of underdeveloped breast tissue under the nipple.
Subjective data collected about the heart and neck vessels helps the nurse to identify abnormal conditions that may affect the client’s ability to perform activities of daily living and to fulfill his role and responsibilities.
Chest pain and Palpitations
- Do you experience chest pain ? When did it start? Describe the type of pain, location, radiation, duration, and how often you experience the pain. Rate the pain on a scale of 0 to 10, with 10 being the worst possible. Does the activity make the pain worse? Did you have perspiration with the chest pain?
- Do you experience palpitations?
- Do you tire easily? Do you experience fatigue ? Describe when the fatigue started. Was it sudden or gradual? Do you notice it at any particular time of the day?
- Do you have difficulty breathing or shortness of breath ?
- Do you wake up at night with an urgent need to urinate? How many times at night?
- Do you experience dizziness?
- Do you experience swelling ( edema ) in your feet, ankles, or legs?
- Do you have frequent heartburn? When does it occur? What relieves it? How often do you experience it?
- Have you been diagnosed with a heart defect or a murmur?
- Have you ever had rheumatic fever ?
- Have you ever had heart surgery or cardiac balloon interventions?
- Have you ever had an electrocardiogram? When was the last one performed? Do you know the results?
- Have you ever had a blood test called a lipid profile? Based on your last test, do you know what your cholesterol levels were?
- Do you take medications or use other treatments for heart disease? How often do you take them? Why do you take them?
- Do you monitor your own heart rate or blood pressure ?
- Is there a history of hypertension , myocardial infarction , coronary heart disease, elevated cholesterol levels, or diabetes mellitus in your family?
- Do you smoke? How many packs of cigarettes per day and for how many years?
- What type of stress do you have in your life? How do you cope with it?
- Describe what you usually eat in a 24-hour period.
- How much alcohol do you consume each day/week?
- Do you exercise? What type of exercise and how often?
- Describe your daily activities. How are they different from your routine 5 or 20 years ago? Does fatigue , chest pain, or shortness of breath limit your ability to perform daily activities? Describe. Are you able to care for yourself?
- Has your heart disease had any effect on your sexual activity?
- How many pillows do you use to sleep at night? Do you get up to urinate during the night? Do you feel rested in the morning?
- How important is having a healthy heart to your ability to feel good about yourself and your appearance? What fears about heart disease do you have?
Neck Vessels
- Observe the jugular venous pulse. Inspect the jugular venous pulse by standing on the right side of the client. The client should be in a supine position with the torso elevated 30 to 45 degrees. Ask the client to turn the head slightly to the left. Shine a tangential light source onto the neck to increase visualizations of pulsations as well as shadows.
- Evaluate jugular venous pressure. Evaluate jugular venous pressure by watching for the distention of the jugular vein .
Auscultation and Palpation
- Auscultate the carotid arteries. Auscultate the carotid arteries if the client is middle-aged or older or if you suspect cardiovascular disease. Place the bell of the stethoscope over the carotid artery and ask the client to hold his or her breath for a moment so breath sounds do not conceal any vascular sounds.
- Palpate the carotid arteries. Palpate each carotid artery alternately by placing the pads of the index and middle fingers medial to the sternocleidomastoid muscle on the neck.
- Inspect pulsations. with the client in a supine position with the head of the bed elevated between 30 and 45 degrees, stand on the client’s right side and look for the apical impulse and abnormal pulsations.
- Palpate the apical pulse. Remain on the client’s right side and ask the client to remain supine. Use the palmar surfaces of your hand to palpate the apical impulse in the mitral area.
- Palpate for abnormal pulsations. Use your palmar surfaces to palpate the apex, left sternal border, and base.
- Auscultate heart rate and rhythm. Place the diaphragm of the stethoscope at the apex and listen closely to the rate and rhythm of the apical impulse.
- If you detect an irregular rhythm, auscultate for a pulse rate deficit. This is done by palpating the radial pulse while you auscultate the apical pulse. Count for a full minute.
- Auscultate to identify S1 and S2. Auscultate the first heart sound (S1 or “lub”) and the second heart sound (S2 or “dub”). Use the diaphragm of the stethoscope to best hear S1. Use the diaphragm of the stethoscope to hear S2 and ask the client to breathe regularly.
- Auscultate for extra heart sounds. Use the diaphragm first, then the bell, to auscultate over the entire heart area. Note the characteristics of any extra sound heard. auscultate during the systolic pause.
- Auscultate for murmurs. Use the diaphragm and the bell of the stethoscope in all areas of auscultation because murmurs have a variety of pitches. Also, auscultate with the client in different positions because some murmurs occur or subside according to the client’s position.
- Auscultate with the client assuming other positions. Ask the client to assume a left lateral position . Use the bell of the stethoscope and listen at the apex of the heart. Ask the client to sit up, lean forward, and exhale. Use the diaphragm of the stethoscope and listen over the apex and along the left sternal border.
It is important for the nurse to ask questions about the symptoms that the client may consider inconsequential. It is also important for the nurse to ask about personal and family history of vascular disease. It is especially important to evaluate aspects of the client’s lifestyle and health factors that may impair peripheral vascular health.
- Have you noticed any color, temperature, or texture changes in your skin?
- Do you experience pain or cramping in your legs? Describe the pain (aching, stabbing). how often does it occur? Does it occur with activity? Does it wake you from sleep?
- Do you have any leg veins that are ropelike, bulging, or contorted? Do you have any sores or open wounds on your legs? Where are they located? Are they painful?
- Do you have any swelling (edema) in your legs or feet? At what time of day is swelling worst? Any pain with swelling?
- Do you have any swollen glands or lymph nodes? If so, do they feel tender, soft, or hard?
- For male clients: Have you experienced a change in your usual sexual activity? Describe.
- Describe any problems you had in the past with the circulation in your arms and legs.
- Have you had any heart or blood vessel surgeries or treatments such as coronary artery bypass grafting, repair of an aneurysm, or vein stripping?
- Do you have a family history of diabetes, hypertension , coronary heart disease, or elevated cholesterol or triglyceride levels?
- Do you (or did you in the past) smoke cigarettes or use any form of tobacco? How much and for how long?
- Do you exercise regularly?
- For female clients: Do you take oral or transdermal contraceptives?
- Describe the degree of stress you normally have.
- How have problems with your circulation affected your ability to function?
- Do leg ulcers or varicose veins affect how you feel about yourself?
- Do you regularly take medications prescribed by your physician to improve your circulation?
- Do you wear support hose to treat varicose veins?
- Observe arm size and venous pattern; also look for edema. Arms are bilaterally symmetric with minimal variation in size and shape. No edema or prominent venous patterning.
- Observe the coloration of the hands and arms. Color varies depending on the client’s skin tone, although color should be the same bilaterally.
- Palpate the client’s fingers, hands, and arms, and note the temperature. Skin is warm to the touch bilaterally from fingertips to upper arms.
- Palpate to assess capillary refill time. Compress the nailbed until it blanches. release the pressure and calculate the time it takes for the color to return.
- Palpate the radial pulse. Gently press the radial artery against the radius. Note elasticity and strength.
- Palpate the ulnar pulses. Apply pressure with your first three fingertips to the medial aspects of the inner wrists.
- Palpate the brachial pulses if you suspect arterial insufficiency. Do this by placing the first three fingertips of each hand at the client’s right and left medial antecubital creases.
- Palpate the epitrochlear lymph nodes. Take the client’s left hand in your right hand as if you were shaking hands. Flex the client’s elbow about 90 degrees. Use your left hand to palpate behind the elbow in the groove between the biceps and triceps muscles.
- Perform the Allen test. The Allen test evaluates the patency of the radial or ulnar arteries. The test begins by assessing ulnar patency. Have the client rest the hand palm side-up on the examination table and make a fist. Then use your thumbs to occlude the radial and ulnar arteries. Note that the palm remains pale. Release the pressure on the ulnar artery and watch for color to return to the hand.
Inspection , Palpation , and Auscultation
- Observe skin color while inspecting both legs from the toes to the groin. Ask the client to lie supine. Then drape the groin area and place a pillow under the client’s head for comfort .
- Inspect the distribution of hair. Hair covers the skin on the legs and appears on the dorsal surface of the toes.
- Inspect for lesions or ulcers. Legs are free of lesions or ulcerations.
- Inspect for edema. Inspect the legs for unilateral and bilateral edema. Note veins, tendons, and bony prominences.
- Palpate edema. If edema is noted during inspection, palpate the area to determine if it is pitting or nonpitting. Press the edematous area with the tips of your fingers, hold for a few seconds, then release.
- Palpate bilaterally for the temperature of the feet and legs. Use the backs of your fingers. Compare your findings in the same areas bilaterally.
- Palpate the superficial inguinal lymph nodes. First, expose the client’s inguinal area, keeping the genitals draped. Feel over the upper medial thigh for the vertical and horizontal groups of superficial inguinal lymph nodes.
- Palpate the femoral pulses. Ask the client to bend the knee and move it out to the side. Press deeply and slowly below and medial to the inguinal ligament. Release pressure until you feel the pulse.
- Auscultate the femoral pulses. If arterial occlusion is suspected in the femoral pulse, position the stethoscope over the femoral artery and listen for bruits.
- Palpate the popliteal pulses. Ask the client to raise the knee partially. Place your thumbs on the knee while positioning your fingers deep in the bend of the knee. Apply pressure to locate the pulse.
- Palpate the dorsalis pedis pulses. Dorsiflex the client’s foot and apply light pressure lateral to and along the side of the extensor tendon of the big toe.
- Palpate the posterior tibial pulses. Palpate behind and just below the medial malleolus. Palpating both posterior tibial pulses at the same time aids in making comparisons.
- Inspect for varicosities and thrombophlebitis . Ask the client to stand because varicose veins may not be visible when the client is supine and not as pronounced when the client is sitting. As the client is standing, inspect for superficial vein thrombophlebitis.
- Check for Homan’s sign. First, flex the client’s knee about 5 degrees, place your hand under the client’s calf muscle, and quickly squeeze the muscle against the tibia . Ask the client to report any pain or tenderness.
The nurse may collect subjective data concerning the abdomen as part of a client’s overall health history interview or as a focused history for a current abdominal complaint. The data focus on symptoms of particular abdominal organs and the function of the digestive system along with aspects of nutrition, usual bowel habits, and lifestyle.
Abdominal Pain
- Are you experiencing abdominal pain?
- How would you describe the pain? How bad is the pain (severity) on a scale of 1 to 10, with 10 being the worst?
- How did (does) the pain begin?
- Where is the pain located? Does it move or has it changed from the original location?
- When does the pain (timing and relation to particular events)?
- What seems to bring on the pain (precipitating factors) make it worse (exacerbating factors), or make it better (alleviating factors)?
- Is the pain associated with any other symptoms such as nausea, vomiting , diarrhea , constipation , gas, fever, weight loss , fatigue , or yellowing of the eyes or skin?
Indigestion
- Do you experience indigestion? Describe.
- Does anything, in particular, seem to cause or aggravate this condition?
Nausea and Vomiting
- Do you experience nausea? Describe. Is it triggered by any particular activities, events, or other factors?
- Have you been vomiting ? Describe the vomitus. Is it associated with any particular trigger factors?
- Have you noticed a change in your appetite? Has this change affected how much you eat or your normal weight?
Bowel Elimination
- Have you experienced a change in bowel elimination patterns? Describe.
- Do you have constipation? Describe. Do you have any accompanying symptoms?
- Have you experienced diarrhea? Describe. Do you have any accompanying symptoms?
- Have you experienced any yellowing of your skin or whites of your eyes, itchy skin, dark urine , or clay-colored stools?
- Have you ever had any of the following gastrointestinal disorders: ulcers, gastroesophageal reflux, inflammatory or obstructive bowel disease, pancreatitis , gallbladder or liver disease, diverticulosis, or appendicitis ?
- Have you had any urinary tract diseases such as infections, kidney disease or nephritis, or kidney stones?
- Have you ever had viral hepatitis ? Have you ever been exposed to viral hepatitis?
- Is there a history of any of the following diseases or disorders in your family: colon , stomach , pancreatic, liver, kidney, or bladder cancer, liver disease, gallbladder disease, or kidney disease?
- Do you drink alcohol? How much? How often?
- What types of foods and how much food do you typically consume each day? How much caffeine do you think you consume each day?
- How much and how often do you exercise? Describe your activities during the day.
- What kind of stress do you have in your life? How does it affect your eating or elimination habits?
- If you have a gastrointestinal disorder, how does it affect your lifestyle, and how do you feel about yourself?
Always follow this sequence when assessing the abdomen: inspection, auscultation, percussion, and palpation. Changing the order can alter the frequency of bowel sounds and make your findings less accurate.
- Observe the coloration of the skin. Abdominal skin may be paler than the general skin tone because this skin is so seldom exposed to the elements.
- Note the vascularity of the abdominal skin. Scattered fine veins may be visible.
- Note any striae. Old, silvery, white striae or stretch marks from past pregnancies or weight gain are normal.
- Inspect for scars . Ask about the source of a scar, and use a centimeter ruler to measure the scar’s length. Document the location by quadrant and reference lines, shape, length, and specific characteristics.
- Assess for lesions and rashes. The abdomen is free of lesions or rashes. Flat or raised brown moles, however, are normal and may be apparent.
- Inspect the umbilicus. Note the color of the umbilical area. Observe the umbilical location. Assess the contour of the umbilicus.
- Inspect abdominal contour. Look across the abdomen at eye level from the client’s side from behind the client’s head, and from the foot of the bed. Measure abdominal girth as indicated.
- Assess abdominal symmetry. Look at the client’s abdomen as she lies in a relaxed supine position.
- Inspect abdominal movement when the client breathes. Abdominal respiratory movement may be seen, especially in male clients.
- Observe aortic pulsations. A slight pulsation of the abdominal aorta , which is visible in the epigastrium, extends full length in thin people.
- Observe for peristaltic waves. Normally peristaltic waves are not seen, although they may be visible in very thin people as slight ripples on the abdominal wall.
- Auscultate for bowel sounds. Use the diaphragm of the stethoscope and make sure that it is warm before you place it on the client’s abdomen.
- Auscultate for vascular sounds. Use the bell of the stethoscope to listen for bruits over the abdominal aorta and renal, iliac, and femoral arteries.
- Auscultate for a friction rub over the liver and spleen. Listen over the right and left lower rib cage with the diaphragm of the stethoscope.
- Percuss for tone. Lightly and systematically percuss all quadrants.
- Percuss the span or height of the liver by determining its lower and upper borders. To assess the lower border, begin in the RLQ at the mid-clavicular line and press upward. Note the change from tympany to dullness. To assess the upper border, percuss over the upper right chest at the MCL and percuss downward, noting the change from lung resonance to liver dullness.
- Percuss the spleen. Begin posterior to the left mid-axillary line (MAL), and percuss downward, noting the change from lung resonance to splenic dullness.
- Perform blunt percussion on the liver. Percuss the liver by placing your left hand flat against the lower right ribcage. Use the ulnar side of your right fist to strike your left hand.
- Perform light palpation. Using the fingertips, begin palpation in a non-tender quadrant, and compress to a depth of 1cm in a dipping motion. Then gently lift your fingers and move to the next area.
- Deeply palpate all quadrants to delineate abdominal organs and detect subtle masses. Using the palmar surface of the fingers, compress to a maximum depth (5 to 6 cm). Perform bimanual palpation if you encounter resistance or assess deeper structures.
- Palpate for masses. Note their location, size, shape, consistency, demarcation, pulsatility, tenderness, and mobility. Do not confuse a mass with a normally palpated organ or structure.
- Palpate the umbilicus and surrounding area for swellings, bulges, or masses. Umbilicus and the surrounding area are free of swellings, bulges, or masses.
- Palpate the aorta. Use your thumb and first finger or two hands and palpate deeply in the epigastrium, slightly to the left of the midline. Assess the pulsation of the abdominal aorta.
- Palpate the liver. Note consistency and tenderness. To palpate bimanually, stand at the client’s right side and place your left hand under the client’s back at the level of the eleventh to twelfth ribs. Lay your right hand parallel to the right costal margin. Ask the client to inhale, then compress upward and inward with your fingers.
- Palpate the spleen. Stand at the client’s right side, reach over the abdomen with your left arm, and place your hand under the posterior lower ribs. Pull up gently. Place your right hand below the left costal margin with the fingers pointing toward the client’s head. Ask the client to inhale and press inward and upward as you provide support with your other hand.
- Palpate the kidneys. To palpate the right kidney, support the right posterior flank with your left hand and place your right hand in the RUQ just below the costal margin at the MCL.
- Palpate the urinary bladder . Palpate for a distended bladder when the client’s history or other findings warrant. Begin at the symphysis pubis and move upward and outward to estimate bladder borders.
When interview topics turn to the reproductive system and female genitalia, keep in mind the sensitivities of the client as well as your own feelings regarding body image , fear of cancer, sexuality, and the like.
Before proceeding with the interview, keep both the topic of the health history and the client’s culture clearly in mind. In some cases, your gender may interfere with accurate results.
Menstrual Cycle
- What was the date of your last menstrual period? Do your menstrual cycles occur on a regular schedule? How long do they last? Describe the typical amount of blood flow you have with your periods. Any clotting ?
- What other symptoms do your experience before or during your period?
- How old were you when you started your period?
- Have you stopped menstruating, or have your periods become irregular? Do you have any spotting between periods? What symptoms have you experienced?
- Are you still having periods? Have your periods changed?
- Are you experiencing any symptoms of menopause?
- Are you on a hormone replacement therapy regimen? If so, what type and dosage? Are you satisfied with HRT?
- What are your concerns about going through menopause?
Vaginal discharge, pain, masses
- Are you experiencing vaginal discharge that is unusual in terms of color, amount, or odor?
- Do you experience pain or itching in your genital or groin area?
- Do you have any lumps, swelling, or masses in your genital area?
- Do you have any difficulty urinating? Do you have any burning or pain with urination? Has your urine changed color or developed an odor? Have you noticed any blood in your urine?
- Do you have difficulty controlling your urine?
Sexual Dysfunction
- Do you have any problems with your sexual performance?
- Have you recently had a change in your sexual activity pattern or libido?
- Do you experience problems with fertility?
- Describe any prior gynecologic problems you have had and the results of any treatment.
- When was your last pelvic examination by a healthcare provider? Was a Pap test performed? What was the result?
- Have you ever been diagnosed with a sexually transmitted disease? If so, what? How was it treated?
- Have you ever been pregnant? How many times? How many children do you have? Is there any chance that you might be pregnant now? Any miscarriages or abortions?
- Have you ever been diagnosed with diabetes?
- Is there a history of reproductive or genital cancer in your family? What type? How is the family member related to you?
- Do you smoke?
- How many sexual partners do you have?
- Do you use contraceptives? What kind? How often?
- Do you have any genital problems that affected your life?
- What is your sexual preference?
- Do you feel comfortable communicating with your partner about your sexual likes and dislikes?
- Do you have any fears related to sex? Can you identify any stress in your current relationship that relates to sex?
- Do you have concerns about fertility? If you have trouble with fertility, how has this affected your relationship with your partner or family?
- Do you perform monthly genital self-examinations?
- How do you feel about going through menopause?
- Do you take estrogen replacement therapy?
- Have you ever been tested for HIV ? What was the result? Why were you tested?
- What do you know about toxic shock syndrome?
- What do you know about STDs and their prevention?
- Do you wear cotton underwear and avoid tight jeans?
- After a bowel movement or urination, do you wipe from front to back?
- Do you douche frequently?
External female genitalia
- Inspect the Mons Pubis. Wash your hands and put on gloves. As you begin the examination, note the distribution of pubic hair. Also, be alert for signs of infestation.
- Observe and palpate inguinal lymph nodes. There should be no enlargement or swelling of the lymph nodes.
- Inspect the labia majora. Observe the labia majora and perineum for lesions, swelling, and excoriation.
- Inspect the labia minora, clitoris, urethral meatus, and vaginal opening. Use your gloved hand to separate the labia majora and inspect for lesions, excoriation, swelling, and/or discharge.
- Palpate Bartholin’s glands. If the client has labial swelling or a history of it, palpate Bartholin’s glands for swelling, tenderness, and discharge. Place your index finger in the vaginal opening and your thumb on the labia majora. With a gentle pinching motion, palpate from the inferior portion of the posterior labia majora to the anterior portion.
- Palpate the urethra . If the client reports urethral symptoms or urethritis, or if you suspect inflammation of Skene’s glands, insert your gloved index finger into the superior portion of the vagina and milk the urethra from the inside, pushing up and out.
Internal female genitalia
- Inspect the size of the vaginal opening and the angle of the vagina. Insert your gloved index finger into the vagina, noting the size of the opening. Then attempt to touch the cervix. Next, while maintaining tension, gently pull the labia majora outward. Note hymenal configuration and transections.
- Inspect the vaginal musculature. Keep your index finger inserted in the client’s vaginal opening. Ask the client to squeeze around your finger. Use your middle and index fingers to separate the labia minora. Ask the client to bear down.
- Inspect the cervix. With the speculum inserted in position to visualize the cervix, observe the cervical color, size, and position. Also, observe the surface and the appearance of the os. Look for discharge and lesions as well.
- Inspect the vagina. Unlock the speculum and slowly rotate and remove it. Inspect the vagina as you remove the speculum. Note the vaginal color, surface, consistency, and any discharge.
When interviewing the male client for information regarding his genitalia, keep in mind that this may be a very sensitive topic for the client and for the examiner as well. Moreover, the examiner should be aware of his own feelings regarding body image , fear of cancer, and sexuality.
- Do you have pain in your penis, scrotum, testes, or groin?
- Have you noticed any lesions on your penis or genital area? If so, do the lesions itch, burn, or sting? Please describe the lesions.
- Have you noticed any discharge from your penis? If so, how much? What color is it? What type of odor does it have?
- Lumps, swelling, masses
- Do you have any lumps, swelling, or masses in your scrotum, genital, or groin area? Have you noticed a change in the size of the scrotum?
- Do you have a heavy, dragging feeling in your scrotum?
- Do you experience difficulty urinating? How many times do you urinate during the night?
- Have you noticed any change in the color, odor, or amount of your urine?
- Do you experience any pain or burning when you urinate?
- Do you ever experience urinary incontinence or dribbling?
- Have you recently had a change in your pattern of sexual activity or sexual desire?
- Do you have difficulty attaining or maintaining an erection? Do you have any problem with ejaculation? Do you have pain with ejaculation?
- Do you have or have you had any trouble with fertility?
- Describe any prior medical problems you have had, how they were treated, and the results.
- When was the last time you had a testicular examination by a physician? What was the result?
- Have you ever been tested for HIV , human papillomavirus, herpes simplex, chlamydia, gonorrhea, and/or trichomoniasis ? What were the results? Why were you tested?
- Is there a history of cancer in your family? What type and which family member(s)?
- What kind of birth control method do you use, if any?
- Are you satisfied with your current level of activity and sexual functioning?
- Do you have concerns regarding your fertility? If you experience fertility troubles, how has this affected your relationship?
- Are you currently exposed to chemicals or radiation? Have you been exposed in the past?
- Describe the activity you perform on a typical day. Do you do any heavy lifting?
- Do you perform testicular self-examinations?
- When was the last time you performed this examination?
- Inspect the base of the penis and pubic hair. Sit on a stool with the client facing you and standing. Ask the client to raise his gown or drape. Note pubic hair growth pattern and any excoriation, erythema, or infestation at the base of the penis and within the pubic hair.
- Inspect the skin of the shaft. Observe for rashes, lesions, or lumps.
- Palpate the shaft. Palpate any abnormalities noted during the inspection. Also, note any hardened or tender areas.
- Inspect the foreskin. Observe the color, location, and integrity of the foreskin in uncircumcised men.
- Inspect the glans. Observe for size, shape, lesions, or redness.
- Palpate the urethral discharge. Gently squeeze the glans between your index finger and thumb.
- Inspect the size, shape, and position. Ask the client to hold his penis out of the way. Observe for swelling, lumps, or bulges.
- Inspect the scrotal skin. Observe color, integrity, and lesions or rashes. To perform an accurate inspection, you must spread out the scrotal folds of the skin. Lift the scrotal sac to inspect the posterior skin.
- Palpate the scrotal contents. Palpate each testis and epididymis between your thumb and first two fingers. Note size, shape, consistency, nodules, and tenderness.
- Continue examination of a scrotal mass by auscultating with a stethoscope. Normal findings are not expected. Bowel sounds may be auscultated over a hernia but will not be heard over a hydrocele .
- Transilluminate the scrotal contents. If an abnormal mass or swelling was noted in the scrotum, transillumination should be performed. Darken the room and shine a light from the back of the scrotum through the mass. Look for a red glow.
Inguinal area
- Inspect for inguinal or femoral hernia. Inspect the inguinal and femoral areas for bulges. Ask the client to turn their head and cough or to bear down as if having a bowel movement, and continue to inspect the areas.
- Palpate for inguinal hernia and inguinal nodes. Ask the client to shift his weight to the left for palpation of the right inguinal canal and vice versa. Place your right index finger into the client’s right scrotum and press upward, invaginating the loose folds of skin. Palpate up the spermatic cord until you reach the triangular-shaped, slitlike opening of the external inguinal ring. Try to push your finger through the opening and, if possible, continue palpating up the inguinal canal.
- Palpate inguinal lymph nodes. If nodes are palpable, note size, consistency, mobility, or tenderness.
- Palpate for femoral hernia. Palpate on the front of the thigh in the femoral canal area. Ask the client to bear down or cough. Feel for bulges. Repeat on the opposite thigh.
- Inspect and palpate for scrotal hernia. Ask the client to lie down; note whether the bulge disappears. If the bulge remains, auscultate it for bowel sounds. Finally, gently palpate the mass and try to push it upward into the abdomen.
The data gathered during subjective assessment provide clues to the client’s overall health and whether he is at risk for diseases and disorders of the anus, rectum, or prostate.
Bowel Patterns
- What is your usual bowel pattern? Have you noticed any recent changes in the pattern? Any pain while passing a bowel movement?
- Do you experience constipation?
- Do you experience diarrhea? Is your diarrhea associated with any nausea or vomiting ?
- Do you have trouble controlling your bowels?
Itching and Pain
- Do you experience any itching or pain in the rectal area ?
- What is the color of your stool ? Hard or soft? Have you noticed any blood on or in your stool ? If so, how much?
- Have you noticed any mucus in your stool ?
- Have you ever had anal or rectal trauma or surgery? Were you born with any congenital deformities of the anus or rectum? Have you had prostate surgery? Have you had hemorrhoids or surgery for hemorrhoids?
- When was the last time you had a stool test to detect blood?
- Have you ever had a proctosigmoidoscopy?
- When was the last time you had a digital rectal examination (DRE) by a physician?
- Have you ever had blood taken for a prostate screening, which measures the level of prostate-specific antigen in your blood? When was the test, and what was the result?
- Is there a history of polyps, colon , rectal cancer, or prostate cancer in your family?
- Do you use any laxatives, stool softeners, enemas, or other bowel movement-enhancing medications?
- Do you engage in anal sex?
- Do you take any medications for your prostate?
- How much high-fiber food and roughage do you consume every day? Do you eat foods high in saturated fats?
- Do you engage in regular exercise?
- Do you use calcium supplements?
- For postmenopausal women: Do you use hormone replacement therapy?
- Has any anal or rectal problem affected your normal activities of daily living ?
Anus and rectum
- Inspect the perianal area. Spread the client’s buttocks and inspect the anal opening and surrounding area.
- Inspect the sacrococcygeal area. Inspect this area for any signs of swelling, redness, dimpling, or hair.
- Palpate the anus. Inform the client that you are going to perform the internal examination at this point. Lubricate your gloved index finger; ask the client to bear down. As the client bears down, place the pad of your index finger on the anal opening. When you feel the sphincter relax, insert your finger gently with the pad facing down.
- Palpate the rectum. Insert your finger further into the rectum as far as possible. Next, turn your hand clockwise. This allows palpation of as much rectal surface as possible. Note tenderness, irregularities, nodules, and hardness.
- Palpate the peritoneal cavity. This area may be palpated in men above the prostate gland in the area of the seminal vesicles on the anterior surface of the rectum. In women, this area may be palpated on the anterior rectal surface in the area of the rectouterine pouch Note tenderness or nodules.
Prostate gland
- In male clients, palpate the prostate. The prostate can be palpated on the anterior surface of the rectum by turning the hand fully counterclockwise so the pad of your index finger faces toward the client’s umbilicus. Note the size, shape, and consistency of the prostate, and identify any nodules or tenderness.
- Inspect the stool. Withdraw your gloved finger. Inspect any fecal matter on your glove. Assess the color, and test the feces for occult blood. Provide the client with a towel to wipe the anorectal area.
Assessment of the musculoskeletal system helps to evaluate the client’s level of functioning with activities of daily living.
- Have you had any recent weight gain?
- Describe any difficulty that you have chewing. Is it associated with tenderness or pain?
- Describe any joint, muscle, or bone pain you have. Where is the pain? what does the pain feel like? When did the pain start? When does it occur? How long does it last? Any stiffness, swelling, or limitation of movement?
- Describe any past problems or injuries you have had to your joints, muscles, or bones. What treatment was given? Do you have any after-effects from the injury or problem?
- When were your last tetanus and polio immunizations?
- Have you ever been diagnosed with diabetes mellitus , sickle cell anemia , systemic lupus erythematosus, or osteoporosis ?
- For middle-aged women: Have you started menopause? Are you receiving estrogen replacement therapy?
- Do you have a family history of rheumatoid arthritis , gout, or osteoporosis?
- What activities do you engage in to promote the health of your muscles and bones?
- What medication are you taking?
- Do you smoke tobacco? How much and how often?
- Do you drink alcohol or caffeinated beverages? How much and how often?
- Describe your typical 24-hour diet. Are you able to consume milk or milk-containing products? Do you take any calcium supplements?
- Describe your activities during a typical day. How much time do you spend in the sunlight?
- Describe any routine exercise that you do.
- Describe your occupation.
- Describe your posture at work and at leisure. What type of shoes do you usually wear?
- Do you have difficulty performing normal activities of daily living? Do you use assistive devices to promote your mobility?
- How have your musculoskeletal problems interfering with your ability to interact or socialize with others? Have they interfered with your usual sexual activity?
- How did you view yourself before this musculoskeletal problem, and how do you view yourself now?
- Has your musculoskeletal problem added stress to your life? Describe.
- Observe gait. Observe the client’s gait as the client enters and walks around the room.
- Assess for the risk of falling backward in the older or handicapped client by performing the “nudge test”. Stand behind the client and put your arms around the client while you gently nudge the sternum.
Temporomandibular joint
- Inspect and palpate the TMJ. Have the client sit, and put your index and middle fingers just anterior to the external ear opening. Ask the client to open the mouth as widely as possible; move the jaw from side to side; and protrude and retract the jaw.
- Test range of motion. Ask the client to open the mouth and move the jaw laterally against resistance. Next, as the client clenches the teeth, feel for the contraction of the temporal and masseter muscles to test the integrity of cranial nerve V.
Sternoclavicular joint
- With the client sitting, inspect the sternoclavicular joint for location in midline, color, swelling, and masses. Then palpate for tenderness or pain.
Cervical, thoracic, lumbar spine
- Observe the cervical, thoracic, and lumbar curves from the side and then from behind. Have the client standing erect with the gown positioned to allow an adequate view of the spine. Observe for symmetry, noting differences in height of the shoulders, the iliac crests, and the buttock areas.
- Palpate the spinous processes and the paravertebral muscles on both sides of the spine for tenderness or pain.
- Test ROM of the cervical spine. Test ROM of the cervical spine by asking the client to touch the chin to the chest and to look up at the ceiling.
- Test ROM of the thoracic and lumbar spine. Ask the client to bend forward and touch the toes. Observe for symmetry of shoulders, scapula, and hips.
- Test for back and leg pain. If the client has low back pain that radiates down the back, perform Lasegue’s test (straight leg raising) to check a herniated nucleus pulpous. Ask the client to lie flat and raise each relaxed leg independently to the point of pain. At the point of pain, dorsiflex the client’s foot.
- Measure leg length. If you suspect the client has one leg longer than the other, measure them. Ask the client to lie down with their legs extended. With a tape, measure the distance between the anterior superior iliac spine and the medial malleolus, crossing the tape on the medial side.
Shoulders, arms, elbows
- Inspect and palpate shoulders and arms. With the client standing or sitting, inspect anteriorly and posteriorly symmetry, color, swelling, and masses. Palpate for tenderness, swelling, or heat.
- Test ROM. Ask the client to stand with both arms straight down at the sides. Nest, ask him to move the arms forward and then backward with elbows straight. Then have the client bring both hands together overhead, elbows straight, followed by moving both hands in front of the body past the midline with elbows straight.
- Inspect for size, shape, deformity, redness, or swelling. Inspect elbows in both flexed and extended positions.
- Test ROM. Ask the client to flex the elbow and bring the hand to the forehead, straighten the elbow, hold the arm out, turn the palm down, then turn the palm up.
Hands, wrists, fingers
- Inspect wrist size, shape, symmetry, color, and swelling. Then palpate for tenderness and nodules. Palpate the anatomic snuffbox (the hollow area on the back of the wrist at the base of the fully extended thumb.
- Test ROM. Ask the client to bend their wrist down and back. Next, have the client hold the wrist straight and move the hand outward and inward.
- Test for carpal tunnel syndrome. Perform Phalen’s test. Ask the client to place the backs of both hands against each other while flexing the wrists 90 degrees downward. Have the client hold this position for 60 seconds
- Inspect size, shape, symmetry swelling, and color. Palpate the fingers from the distal end proximally, noting tenderness, swelling, bony prominences, nodules, or crepitus of each interphalangeal joint.
- Test ROM. Ask the client to spread the fingers apart, make a fist, bend the fingers down and then up, move the thumb away from other fingers, and touch the thumb to the base of the small finger.
- With the client standing, inspect the symmetry and shape of the hips. Palpate for stability, tenderness, and crepitus.
- Test ROM. With the client supine, ask the client to: Raise the extended leg; flex the knee up to the chest while keeping the other leg extended; move an extended leg away from the midline of the body as far as possible and then toward the midline of the body as far as possible. Bend the knee and turn the leg inward and then outward.
- With the client supine and then sitting with knees dangling, inspect for size, shape, symmetry, swelling, deformities, and alignment. Observe for quadricep muscle atrophy.
- Test for swelling. The bulge test helps detect a small amount of fluid in the knee. With the client in the supine position, use the ball of your hand firmly to stroke the medial side of the knee upward. three to four times, to displace any accumulated fluid. Then press on the lateral side of the knee and look for a bulge on the medial side of the knee.
- Perform the ballottement test. With the client in a supine position, firmly press your non-dominant thumb and index finger on each side of the patella. Then with your dominant fingers, push the patella down on the femur .
- Test ROM. Ask the client to bend each knee up toward the buttocks or back, straighten the knee, and walk normally.
- Test for pain and injury. With the client in the supine position, ask the client to flex one knee and hip. Then place your thumb and index finger of one hand on either side of the knee. Use your other hand to hold the heel of the foot up. Rotate the lower leg and foot laterally. Slowly extend the knee, noting pain or clicking.
Ankles and feet
- With the client sitting, standing, and walking , inspect position, alignment, shape, and skin.
- Palpate ankles and feet for tenderness, heat, swelling, and nodules. Palpate the toes from the distal end proximally, noting tenderness, swelling, boney prominences, nodules, or crepitus of each interphalangeal joint.
- Test ROM. Ask the client to point toes upward then downward, turn soles outward then inward, rotate foot outward then inward, turn toes under foot and then upward.
Problems with other body systems may affect the neurologic system, and neurologic system disorders can affect all other body systems. Regardless of the source of neurologic problems, the client’s total lifestyle and level of functioning are often affected.
Numbness and Tingling
- Do you experience any numbness or tingling? When and where does this occur?
- Do you experience seizures ?
- Describe what happens before you have the seizure and where on your body the seizure starts. Does anything seem to initiate a seizure? Do you lose control of your bladder during the seizure? How do you feel afterward? Do you take medications for seizures? Do you wear medical identification to alert others that you have seizures? Do you take safety precautions regarding driving or operating dangerous machinery?
- Do you experience headaches? When do they occur, and what do they feel like?
- Do you experience dizziness or lightheadedness or problems with balance or coordination ? If so, how often? Does it occur with activity? Or have you experienced any falling ? Do you have any clumsy movements?
- Have you noticed a decrease in your ability to smell or taste?
- Have you experienced any ringing in your ears or hearing loss?
- Have you noticed any change in your vision?
Difficulty Speaking
- Do you have difficulty understanding when people are talking to you? Do you have difficulty in making others understand you? Do you have difficulty forming words or verbally interpreting your thoughts?
Difficulty Swallowing
- Do you experience difficulty swallowing?
Muscle Control
- Have you lost bowel or bladder control, or do you retain urine?
- Do you have muscle weakness ? If so, where?
- Do you experience any tremors? If so, where?
Memory Loss
- Do you experience any memory loss?
- Have you ever had any type of head injury with or without loss of consciousness? If so, describe any physical or mental changes that have occurred as a result. What type of treatment did you receive?
- Have you ever had meningitis , encephalitis , injury to the spinal cord , or a stroke ? If so, describe any physical or mental changes that have occurred as a result. What type of treatment did you receive?
- Do you have a family history of high blood pressure , stroke, Alzheimer’s disease, epilepsy , brain cancer , or Huntington’s chorea?
- Do you take any prescription or nonprescription medications? How much alcohol do you drink? Do you use recreational drugs such as marijuana , tranquilizers, barbiturates , or cocaine ?
- Do you wear your seatbelt when riding in vehicles? Do you wear protective headgear when riding a bicycle or playing sports?
- Describe your usual daily diet.
- Have you ever had prolonged exposure to lead, insecticides, pollutants, and other chemicals?
- Do you frequently lift heavy objects or perform repetitive motions?
- Can you perform your normal activities of daily living?
- Has your neurologic problem changed the way you view yourself? Describe.
- Has your neurologic problem added much stress to your life? Describe.
Neurological status, Mental status, and LOC
- Observe the level of consciousness. Call the client’s name and not the response. If the client does not respond, call the name louder. If necessary, shake the client gently. If the client still does not respond, apply a painful stimulus.
- Observe posture and body movements. Be alert for tense, nervous, fidgety, and restless behavior, which may be seen in anxiety or may simply reflect the client’s apprehension during a physical examination.
- Observe dress, grooming , and hygiene . Keep the examination setting and the reason for the assessment in mind as you note the client’s degree of cleanliness and attire.
- Observe facial expressions. Note particularly eye contact and affect.
- Observe speech. Observe and listen to the tone, clarity, and pace of speech.
- Observe mood, feelings, and expressions. Ask the client, “How are you feeling today?” and “What are your plans for the future?”
- Observe thought processes and perceptions. Observe thought processes for clarity, content, and perception by inquiring about the client’s thoughts and perceptions expressed.
- Observe cognitive abilities. Ask for the client’s name and names of family members, the time, and where the client lives or is now. Note the client’s ability to focus and stay attentive to you during the interview and examination. Ask the client, “What did you have to eat today?” or “What is the weather like today?”. Ask the client, “When did you get your first job?” or “When is your birthday?” Ask the client to repeat four unrelated words. The words should not rhyme, and they cannot have the same meaning. Have the client repeat these words in 5 minutes, again in 10 minutes, and again in 30 minutes
- Perform the Mini-Mental State Examination if time is limited and a quick standard measure is needed to evaluate or reevaluate the cognitive function.
Cranial nerves
- Test CN I (olfactory). For all assessments of the cranial nerves , have the client sit in a comfortable position at your eye level. Ask the client to clear the nose to remove any mucus, then to close their eyes, occlude one nostril, and identify a scented object that you are holding.
- Test CN II (optic). Use the Snellen chart to assess vision in each eye. Ask the client to read a newspaper or magazine paragraph to assess near vision. Assess the visual fields of each eye by confrontation. Use an ophthalmoscope to view the retina and optic disc of each eye.
- Assess CN III ( oculomotor ), IV (trochlear), and VI (abducens). Inspect the margins of the eyelids of each eye. Assess extraocular movements. If nystagmus is noted, determine the direction of the fast and slow phases of movement. Assess pupillary response to light and accommodation in both eyes.
- Assess CN V (trigeminal). Test motor function. Ask the client to clench the teeth while you palpate the temporal and masseter muscles for contraction. Test sensory function. Tell the client: “I am going to touch your forehead, cheeks, and chin with the sharp or dull side of this safety pin or paper clip. Please close your eyes and tell me if you feel a sharp or dull sensation. also, tell me where you feel it.”
- Test CN VII (facial). Test motor function. Ask the client to smile, frown and wrinkle the forehead, show teeth, puff out cheeks, purse lips, raise eyebrows, and close eyes tightly against resistance.
- Test CN VIII (acoustic/vestibulocochlear). Test the client’s hearing ability in each ear and perform the Weber and Rinne tests to assess the cochlear (auditory) component of cranial nerve VIII.
- Test CN IX (glossopharyngeal) and X (vagus). Test motor function. Ask the client to open their mouth wide and say “ah” while you use a tongue depressor on the client’s tongue. Test the gag reflex by touching the posterior pharynx with the tongue depressor.
- Test CN XI (spinal accessory). Ask the client to shrug the shoulders against resistance to assess the trapezius muscle. Ask the client to turn the head against resistance, first to the right and then to the left, to assess the sternocleidomastoid muscle.
- Test CN XII (hypoglossal). To assess the strength and mobility of the tongue, ask the client to protrude the tongue, move it to each side against the resistance of a tongue depressor, then put it back in the mouth.
Motor and cerebellar systems
- Assess the condition and movement of muscles. Assess the size and symmetry of all muscle groups. Assess the strength and tone of all muscle groups. Note any unusual involuntary movements such as fasciculations, tics, or tremors.
- Evaluate balance. To assess gait, ask the client to walk naturally across the room. Note posture, freedom of movement, symmetry, rhythm, and balance. Ask the client to walk in heel-to-toe fashion, next on the heels, then on the toes. Perform Romberg test. Ask the client to stand erect with arms at the side and feet together. Note any unsteadiness or swaying.
- Assess coordination . Demonstrate the finger-to-nose test to assess the accuracy of movements, then ask the client to extend and hold arms out to the side with eyes open. Next, say, “Touch the tip of your nose first with your right index finger, then with your left index finger.
Sensory systems
- Assess light touch, pain, and temperature sensations. For each test, ask clients to close both eyes and tell you what they feel and where they feel it. Scatter stimuli over the distal and proximal parts of all extremities and the trunk to cover most of the dermatomes. To test the light touch sensation, use a wisp of cotton to touch the client. To test pain sensation, use the blunt and sharp ends of a safety pin or paper clip. to test temperature sensation, use test tubes filled with hot and cold water.
- Test vibratory sensation. Strike a low-pitched tuning fork on the heel of your hand and hold the base on a bony surface of the fingers or big toe. Ask the client to indicate what he feels.
- Test sensitivity to position. Ask the client to close both eyes. Then move the client’s toes or a finger up or down. Ask the client to tell you the direction it is moved.
- Assess tactile discrimination (fine touch). Remember that the client should have her eyes closed. To test stereognosis, place a familiar object such as a quarter, paper clip, or key in the client’s hand and ask the client to identify it. To test point localization, briefly touch the client and ask the client to identify the points touched. to test graphesthesia, use a blunt instrument to write a number on the palm of the client’s hand. Ask the client to identify the number.
33 thoughts on “Head-to-Toe Assessment: Complete Physical Assessment Guide”
I appreciate the topics you are posting. It helps a lot and very informative. It enhances my nursing practice. Keep up the good work!
all the topics are really helpful!!! thanks a lot! godspeed! keep up the good work :)
Thank you. I appreciate your hard work by putting everything together and sharing
hi, please help me if you have OSCE review notes. Thanks
this is a very reliable source of information for nursing students, I always recommend it to my mates, I really love it. Please make more notes on drug study so we don’t have to look elsewhere
It is a big helpful source of info which today im using it for our activity regarding to physical assestment. I really appreciate it. Thank you. From 1st yr nursing student.
Your post are very helpful. Thank you
you are awesome….thanks
Good site to refer for your care plans and physical assessments. Thank You
thank you so much all your post are very helpful ,it makes our studying much easier
great topics , it makes my studying much easier
Thank you for what you do. It helps when I am trying to understand something the instructors are lecturing about, but don’t have time to answer all the questions we have.
Great detailed cheat sheet. Thanks!
You are awesome! Thanks and God bless!
DEAR MATT VERA, Excellent work you are doing for the nurses world. Your contents are very good. I am Dr.M.Sumathi, PhD Nurse from India. I am a nurse educator. I am proud of you dear. keep doing this for the young budding nurses.
You are definitely doing God’s work. Thank you.
I really appreciate your help. It has really simplified the physical assessment techniques.
Yes you right
Exactly what have looking for! Much blessings
Thank you so much for this!
Excelente trabajo complementa y facilita la enseñanza gracias
Thanks you this gives an excellent insight on health assessment and will surely apply.
Good job, it’s very helpful
This is very informative and I do appreciate your hard work and effort. I will share this information with my classmates I feel it is very useful.
This is very useful and important to read all nurses. Thank you
Hi Estifanos, You’re very welcome! I’m glad you found the head-to-toe physical assessment guide so valuable. It’s definitely a fundamental skill for all nurses. Which part of the head-to-toe assessment do you find most challenging, or is there a particular aspect you’d like to learn more about? Happy to help anytime!
Good job,very helpful
Glad to be of help, Lincy.
I want to be part of this community
Thanks alot for the time and effort taken. Pls guide on communicating a patients condion on an accurate summarized way especially when handing over or when providing updates.
This is so detailed and helpful. Learning this for the first time I’m actually very happy that I finally have a stop for everything place to learn❤️
Leave a Comment Cancel reply

IMAGES
VIDEO
COMMENTS
This essay discusses my own experiences, impressions, and lessons learned from the head nurse's work. Indeed, most of the time, the patient spends with nurses and other nursing staff, and they are the face of the institution through which patients learn about the culture and values of the clinic. Nevertheless, as a leader, the head nurse is ...
Systematic Review of Head Nurse Leadership Style and ...
Head Nurse: Definition, Skills and Job Description Example
A study from Belgium revealed that head nurses and nurse directors were excessively implementing passive-avoidant leadership styles in contrast to transformational leadership styles in nursing homes. Subsequently, all leadership outcomes (extra effort, effectiveness, and satisfaction) were significantly lower among both the head and director of ...
A head nurse is an administrator, a nurse clinician, and a teacher in a specified unit of nursing service, where she is responsible for the planning, coordinating, and rendering of quality nursing care given the patients assigned to her unit. Legally she is responsible, with al the individuals who work with her, to provide quality nursing service. She is expected to know the educational and ...
Jot down your qualifications, anecdotes, and a strong opening statement. Create an outline to organize your thoughts and ensure your essay is concise and easy to read. 2. Distinguish Yourself. Admissions committees read numerous essays, so make yours memorable. Include personal anecdotes that showcase your personality, passion, and suitability ...
10 Tips to Write an Effective Nursing School Essay
A typical nursing essay writing process takes three stages: prewriting, writing, and post-writing. Of course, this also applies when writing a nursing research paper or a case study, for that matter. Note that the time, effort, and dedication required may differ depending on the essay's type, length, and scope.
As a result, nursing essays can take many different forms and cover a wide range of topics. Given below are some examples of different types of nursing essays: Personal Philosophy Of Nursing - Essay Examples. Cal State Fullerton Nursing Essay Examples. Evidence Based Practice Nursing In Medical Field - Essay Examples.
How to Write a Nursing Essay - Examples, Tips and Outline
Impact of Nurse Leaders Behaviors on Nursing Staff ...
As a student nurse, knowledge is easy to get as we experience, learn, read and study. But every knowledge comes with great responsibility, which is to help and share it to others who are innocent about specifically toward to their health. Experiencing being a student head nurse is good as it adds my capabilities to manage my time, and my staff ...
The current Nursing Now work speaks volumes. The collaboration with WHO, ICN, and Nursing Now has already proved a success in a number of projects; facilitating nursing leaders to be more visible in policy and decision making tables. There is certainly more awareness on the complexity of nursing practice and the need for this to be recognised.
When crafting your essay, consider using essay examples as a reference. Focus on highlighting your strengths, motivations to pursue nursing, and unique qualities that make you a strong candidate. Additionally, tailor your essay to each college application to demonstrate your genuine interest. 3.
Personal Statement for Nursing School: Tips + Examples
Description. Emotional intelligence is defined by Ashkanasy et al. (2016) as being a group of capabilities that help in working with emotions. It is the ability to be aware of one's emotions and to control them and express them effectively, with care and utilising empathy (Goleman et al., 2013). As explained by Quinn and Hoffe (2018 ...
Step 1: Understand the Prompt and Requirements. Usually, the school will provide special instructions or prompt for your application essay. It is essential to carefully read and understand the prompt and any specific requirements or guidelines the school offers. Ensure you address all aspects of the prompt and follow any formatting or length ...
Start Broad. When writing essays entirely about why you want to pursue nursing, try to start from a broad interest, then slowly work your way to telling specific personal stories and goals. When first thinking about your general interest in nursing, ask yourself what attracts you to the work of being a nurse. This can lead to powerful potential ...
How to Conduct a Nursing Head-to-Toe Assessment
1. Plan Well. To pen an excellent nursing school essay that gets you accepted, you need to plan the essay. Read the instructions, brainstorm as you take notes, research widely, and create an outline. And even when done, the purpose is to have a reverse outline to help you score the essay against the requirements.
Running Head: Nursing Care Study. E.S. is a 94 year old female, born July 30, 1909. She is widowed. She is of Catholic religion. She stated that her mother was from Germany and her father was from Ireland. She is an only child, and never finished school because she married at a young age. Her date of admission was July 8, 2002 with the ...
Head-to-Toe Assessment: Complete Physical ...